The perforation and subsequent panperitonitis as one of the complications of a Meckel diverticulum is a rare complication, especially in infants. Complication of Meckel diverticulum, preoperative and operative patient's mean age is about 5 years old. A 13-month-old male infant presented at our emergency room with currant jelly stool of about 24 hours duration. Intussusception or bacterial enteritis was initially suspected. Gastrointestinal ultrasonography showed no evidence of intussusception or appendicitis. On the 3rd hospital day, he suddenly showed high fever and irritability. Abdominal CT suggested intraperitoneal and retroperitoneal abscess with air collection due to possible bowel perforation. The final diagnosis of perforation of Meckel diverticulum was made by laparoscopy and biopsy. We report a very rare case with perforation of Meckel diverticulum in infant period.
The survival of Very Low Birth Weight (VLBW) infants has been improved with the advancement of neonatal intensive care. However, the incidence of accompanying gastrointestinal complications such as necrotizing enterocolitis has also been increasing. In intestinal perforation of the newborn, enterostomy with or without intestinal resection is a common practice, but there is no clear indication when to close the enterostomy. To determine the proper timing of enterostomy closure, the medical records of 12 VLBW infants who underwent enterostomy due to intestinal perforation between Jan. 2004 and Jul. 2007 were reviewed retrospectively. Enterostomy was closed when patients were weaned from ventilator, incubator-out and gaining adequate body weight. Pre-operative distal loop contrast radiographs were obtained to confirm the distal passage and complete removal of the contrast media within 24-hours. Until patients reached oral intake, all patients received central-alimentation. The mean gestational age of patients was 26+2 wks (24+1~33+0 wks) and the mean birth weight was 827 g (490~1450 g). The mean age and the mean body weight at the time of enterostomy formation were 15days (6~38 days) and 888 g (590~1870 g). The mean body weight gain was 18 g/day (14~25 g/day) with enterostomy. Enterostomy closure was performed on the average of 90days (30~123 days) after enterostomy formation. The mean age and the mean body weight were 105 days (43~136 days) and 2487 g (2290~2970 g) at the time of enterostomy closure. The mean body weight gain was 22 g/day after enterostomy closure. Major complications were not observed. In conclusion, the growth in VLBW infants having enterostomy was possible while supporting nutrition with central-alimentation and the enterostomy can be closed safely when the patient's body weights is more than 2.3 kg.
Recently, the survival rates of extremely low-birth-weight (ELBW) infants have improved with the development of neonatal intensive care. However, these infants were susceptible to intestinal perforation due to prematurity, fluid restriction, and injection of indomethacin, etc. Because of the risks of transportation, anesthesia and surgery itself, peritoneal drainage has been compared with laparotomy. Through our experience, we investigate the usefulness of peritoneal drainage retrospectively. From 1997 to 2007, six ELBW (M:F=5:1) underwent primary peritoneal drainage for intestinal perforation. Their median birth weight was 685 g (405~870) and gestational age was 25+1 weeks (24+3~27+0). We noticed the intestinal perforation at median 10.5 days (8~18) after birth, and placed Penrose drain or Jackson-Pratt drain through right lower quadrant incision under local anesthesia. The cause of intestinal perforation was necrotizing enterocolitis in one patient, but that of the others was not clear. Three patients who showed normal platelet count and stable vital signs recovered uneventfully. Two patients (birth weight less than 500 g) who showed unstable vital signs and low platelet count (12,000 / mm3 to 30,000 / mm3) expired despite aggressive resuscitation. One patient required laparotomy due to persistent intestinal obstruction after drain removal and survived. Our experience shows that peritoneal drainage was an acceptable treatment for ELBW infants and the prognosis was related to vital sign and platelet count at the time of intestinal perforation, and birth weight.
A nationwide survey on necrotizing enterocolitis (NEC) was undertaken among members of the Korean Association of Pediatric Surgeons. The members were required to complete a questionnaire and the case registration form for each patient during the three-year period from July 2001 to June 2004. Eighty one patients were included in the questionnaire, but only 71 patients were registered from 22 members in 16 hospitals. At the same time survey on focal intestinal perforation (FIP) was undertaken and 17 patients were registered from 11 members in 10 hospitals. Total 19,041 newborns were admitted to neonatal intensive care unit during the study period. Eighty one patients (17.27 %) were underwent surgery among 469 babies who were managed under the impression of NEC. The male to female ratio was 2.1:1. The premature were 60.6 %. The most common site of involvement was ileum. Overall and operation survival of NEC were 72 % and 79 %, respectively. The survival was lower in smaller babies, multiple segments involvement and involvement of both the small and large intestine. But there was no difference in survival according to sex or prematurity. The FIP showed very similarity with NEC in terms of incidence, and the age of diagnosis and operation. But the survival was much better and 100 %. The results showed the clinical characteristics of NEC and the trend of management in NEC in Korea. In the future we hope we can discuss about this topic in prospective manner.
Perforation of the gastrointestinal tract in neonatal period has been associated with a grim prognosis. Recently there has been some improvement in survival. To evaluate the remaining pitfalls in management, 19 neonatal gastrointestinal perforation cases from May 1989 to July 1996 were analysed retrospectively. Seven patients were premature and low birth weight infants. Perforation was most common in the ileum{56.3%). Mechanical or functional obstruction distal to the perforation site was identified in 7 cases; Hirschsprung's disease 3, small bowel atresia 3, and anorectal malformation 1. These lesions were often not diagnosed until operation. Five cases of necrotizing enterocolitis and 1 of muscular defect were the other causes of perforation. In six cases, the cause of the perforation was not identified. Perinatal ischemic episodes were associated in five cases. Overall mortality was 15.1 %. Because a considerable number of gastrointestinal perforations resulted from distal obstruction, pediatric surgeon should be alert for early identification and intervention of gastrointestinal obstruction, particularly in patients that are premature and have a history of ischemia..
Children tend to ingest foreign bodies. The majority present in children between the ages of 6 months and 3 years. We experienced 2 cases of unusual gastrointestinal complications caused by ingested foreign bodies. First case was a 10-month-old male with intestinal perforation due to two pieces of ingested magnetic beads. Second case was a 7-month-old girl with esophageal stricture due to an ingested particle of plastic toy.
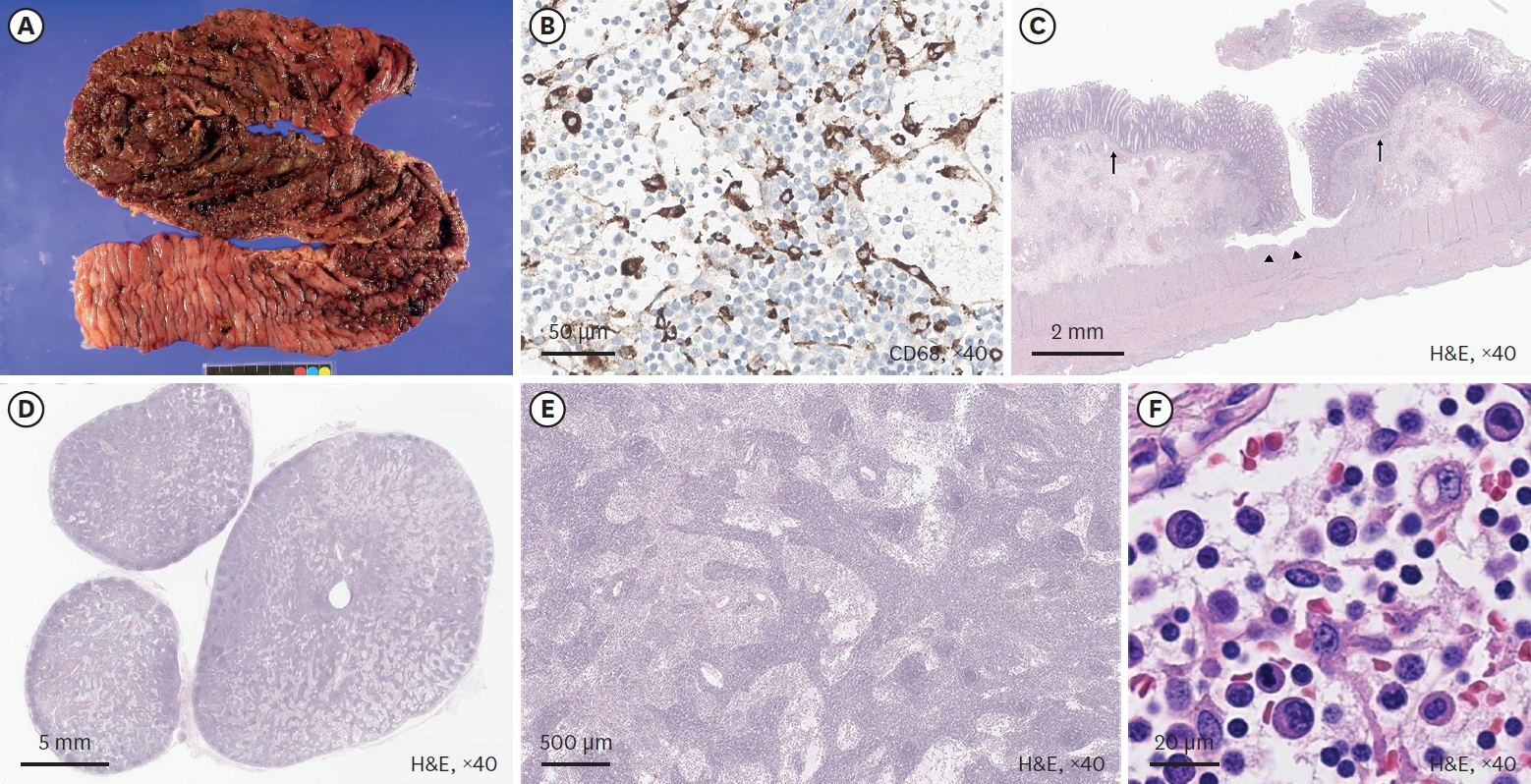
Neonatal intestinal perforation is mainly caused by necrotizing enterocolitis, intestinal atresia, meconium ileus or unknown etiology. Occasionally, Hirschsprung's disease presents with neonatal intestinal perforation, of which, it is known that total colonic aganglionosis is common. Therefore, Hirschsprung's disease should be considered as a cause of neonatal intestinal perforation.
The authors have experienced 3 cases of neonatal Hirschsprung's disease associated with colonic perforations. Cecal perforations were noted in 2 cases with aganglionosis from descending colon and sigmoid perforation in a case with aganglionosis in rectum. These cases will be discussed with literature review.

