Department of Pediatric Surgery, Seoul National University Children's Hospital, Seoul, Korea.
Copyright © 2013 Korean Association of Pediatric Surgeons
Abbreviations: WBC; white blood cell, Hb; hemoglobin, CRP; C-reactive protein, BP; blood pressure, PR; pulse rate, RR; respiratory rate, BT; body temperature, APACHE; Acute Physiology and Chronic Health Evaluation
AAST (American Association for the Surgery of Trauma) Classification
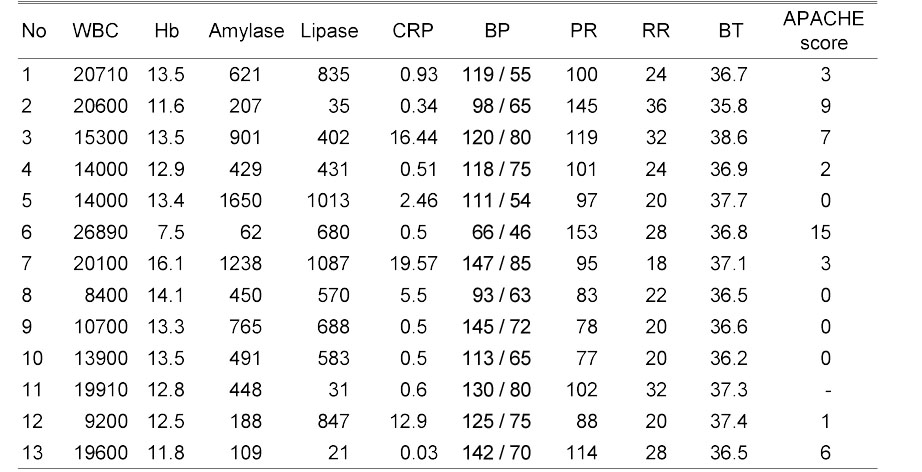
Preoperative Clinical Findings and APACHE Score
Abbreviations: WBC; white blood cell, Hb; hemoglobin, CRP; C-reactive protein, BP; blood pressure, PR; pulse rate, RR; respiratory rate, BT; body temperature, APACHE; Acute Physiology and Chronic Health Evaluation
Comparison between Preoperative Radiologic Findings and Postoperative Findings
Abbreviations: CT; computed tomography, MRI; magnetic resonance imaging, AAST; American Association for the Surgery of Trauma
*Additional examination (ERCP)
Patients Characteristics and Clinical Course
Abbreviations: SPDP; spleen preserving distal pancreatectomy, PPPD; pylorus preserving pancreaticoduodenectomy, DP; distal pancreatectomy, STP; subtotal pancreatectomy
*Combiled operation: S2 segmentectomy, †Combined operation: right hemicolectomy
Abbreviations: WBC; white blood cell, Hb; hemoglobin, CRP; C-reactive protein, BP; blood pressure, PR; pulse rate, RR; respiratory rate, BT; body temperature, APACHE; Acute Physiology and Chronic Health Evaluation
Abbreviations: CT; computed tomography, MRI; magnetic resonance imaging, AAST; American Association for the Surgery of Trauma
*Additional examination (ERCP)
Abbreviations: SPDP; spleen preserving distal pancreatectomy, PPPD; pylorus preserving pancreaticoduodenectomy, DP; distal pancreatectomy, STP; subtotal pancreatectomy
*Combiled operation: S2 segmentectomy, †Combined operation: right hemicolectomy