1Department of Surgery, Inje University Haeundae Paik Hospital, Busan, Korea.
2Department of Pediatrics, Inje University Haeundae Paik Hospital, Busan, Korea.
3Department of Surgery, Dong-A University College of Medicine, Busan, Korea.
Copyright © 2015 by the Korean Association of Pediatric Surgeons
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (https://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
No potential conflict of interest relevant to this article was reported.
The abstract of this article was presented at the 30th Annual Meeting of the Korean Association of Pediatric Surgeons on June 2014 in Busan, Korea.
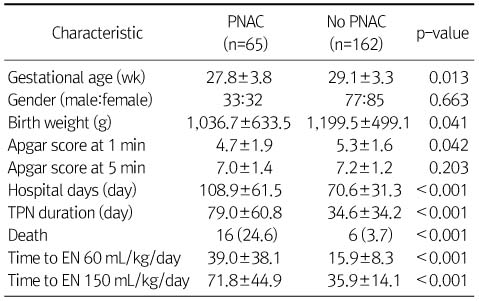
Values are presented as mean±SD, ratio, or n (%).
PNAC, parenteral nutrition associated cholestasis; TPN, total parenteral nutrition; EN, enteral nutrition.
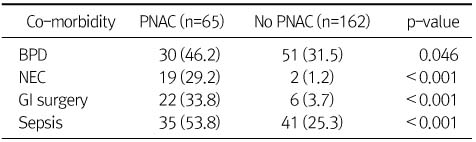
Values are presented as n (%).
PNAC, parenteral nutrition associated cholestasis; BPD, bronchopulmonary dysplasia; NEC, necrotizing enterocolitis; GI, gastrointestinal.
Clinical Characteristics
Values are presented as mean±SD, ratio, or n (%).
PNAC, parenteral nutrition associated cholestasis; TPN, total parenteral nutrition; EN, enteral nutrition.
Cause of Death
PNAC, parenteral nutrition associated cholestasis; PPHN, pulmonary hypertension of the newborn.
Co-morbidities
Values are presented as n (%).
PNAC, parenteral nutrition associated cholestasis; BPD, bronchopulmonary dysplasia; NEC, necrotizing enterocolitis; GI, gastrointestinal.
Laboratory Findings
Values are presented as mean±SD.
PNAC, parenteral nutrition associated cholestasis.
Radiologic Findings
Values are presented as n (%) or n only.
PNAC, parenteral nutrition associated cholestasis.
Macronutrients
Values are presented as n (%).
PNAC, parenteral nutrition associated cholestasis; LCT, long chain triglycerides; MCT, medium chain triglycerides.
Values are presented as mean±SD, ratio, or n (%).
PNAC, parenteral nutrition associated cholestasis; TPN, total parenteral nutrition; EN, enteral nutrition.
PNAC, parenteral nutrition associated cholestasis; PPHN, pulmonary hypertension of the newborn.
Values are presented as n (%).
PNAC, parenteral nutrition associated cholestasis; BPD, bronchopulmonary dysplasia; NEC, necrotizing enterocolitis; GI, gastrointestinal.
Values are presented as mean±SD.
PNAC, parenteral nutrition associated cholestasis.
Values are presented as n (%) or n only.
PNAC, parenteral nutrition associated cholestasis.
Values are presented as n (%).
PNAC, parenteral nutrition associated cholestasis; LCT, long chain triglycerides; MCT, medium chain triglycerides.