Spontaneous neonatal gastric perforation is a rare but fatal disease with unclear etiology. In this study, we reviewed its clinical manifestations, outcomes, and discussed the etiology and prognostic factors.
There were 12 neonates with gastric perforation in our hospital from 1989 to 2015. Their medical records were reviewed retrospectively including birth record, associated disease, site and size of perforation, type of surgical management, clinical outcome. Also, the prognostic factors were analyzed.
The median gestational age and birth weight was 32 weeks (range, 26-43 weeks; preterm birth rate, 66.7%) and 1,883 g (range, 470-4,400 g), respectively. Five patients had associated gastrointestinal anomalies including esophageal atresia and tracheoesophageal fistula (two patients), midgut volvulus, non-rotation and microcolon, and meconium plug syndrome. The median age at surgery was six days after birth (range, 2-13 days), and the median weight at surgery was 1,620 g (range, 510-3,240 g). Upper third part of stomach was the most frequently involved location of perforation. The size of perforation varied from pin point to involving the whole greater curvature. Primary repairs were done in seven cases, and in five cases, resections of necrotic portion were needed. Mortality rate was 33.3% (n=4), morbidity (re-operation) rate was 16.7% (n=2). The causes of death were sepsis (n=3), and heart failure from Ebstein anomaly (n=1). The median hospital stay was 92.5 days (range, 1-176 days). The factors mentioned as prognostic factors in previous studies showed no significant relations to the mortality and morbidity in our study.
There were improvements of outcomes in patients with large size perforation. As previous studies, we assume these improvements were possible due to the improvements of critical care medicine. Given that rare incidence, a multi-center study can help us get a better understanding of this disease, and a better outcome.
The perforation and subsequent panperitonitis as one of the complications of a Meckel diverticulum is a rare complication, especially in infants. Complication of Meckel diverticulum, preoperative and operative patient's mean age is about 5 years old. A 13-month-old male infant presented at our emergency room with currant jelly stool of about 24 hours duration. Intussusception or bacterial enteritis was initially suspected. Gastrointestinal ultrasonography showed no evidence of intussusception or appendicitis. On the 3rd hospital day, he suddenly showed high fever and irritability. Abdominal CT suggested intraperitoneal and retroperitoneal abscess with air collection due to possible bowel perforation. The final diagnosis of perforation of Meckel diverticulum was made by laparoscopy and biopsy. We report a very rare case with perforation of Meckel diverticulum in infant period.
Use of laparoscopic appendectomy (LA) for perforated appendicitis (PA) in children remains controversial because of the development of postoperative intra-abdominal abscess formation. We developed the irrigation method for the prevention of abscess formation after LA performed for PA in children with severe panperitonitis. We called it ‘the shaking irrigation’. The object of this study was to analyze the efficacy of this irrigation method. All cases of PA with severe panperitonitis in children that underwent LA with massive shaking irrigation and drainage between June 2003 and December 2007 were studied retrospectively. We included only PA with panperitonitis and large amounts of purulent ascites throughout the abdomen as well as an inflamed small bowel with ileus. Thirty-four children were involved in this study. The mean patient age was eight years. The mean amount of irrigation fluid was 8.2L (range: 4-15L). The mean operative time was 89.5 min. The mean length of the hospital stay was 5.1 days. There were no postoperative intra-abdominal abscesses. There was no conversion to open surgery. In conclusion, Use of LA in PA with severe panperitonitis in children is safe and effective. Massive shaking irrigation and abdominal drainage appears to prevent intra-abdominal abscesses after LA for PA with panperitonitis.
The survival of Very Low Birth Weight (VLBW) infants has been improved with the advancement of neonatal intensive care. However, the incidence of accompanying gastrointestinal complications such as necrotizing enterocolitis has also been increasing. In intestinal perforation of the newborn, enterostomy with or without intestinal resection is a common practice, but there is no clear indication when to close the enterostomy. To determine the proper timing of enterostomy closure, the medical records of 12 VLBW infants who underwent enterostomy due to intestinal perforation between Jan. 2004 and Jul. 2007 were reviewed retrospectively. Enterostomy was closed when patients were weaned from ventilator, incubator-out and gaining adequate body weight. Pre-operative distal loop contrast radiographs were obtained to confirm the distal passage and complete removal of the contrast media within 24-hours. Until patients reached oral intake, all patients received central-alimentation. The mean gestational age of patients was 26+2 wks (24+1~33+0 wks) and the mean birth weight was 827 g (490~1450 g). The mean age and the mean body weight at the time of enterostomy formation were 15days (6~38 days) and 888 g (590~1870 g). The mean body weight gain was 18 g/day (14~25 g/day) with enterostomy. Enterostomy closure was performed on the average of 90days (30~123 days) after enterostomy formation. The mean age and the mean body weight were 105 days (43~136 days) and 2487 g (2290~2970 g) at the time of enterostomy closure. The mean body weight gain was 22 g/day after enterostomy closure. Major complications were not observed. In conclusion, the growth in VLBW infants having enterostomy was possible while supporting nutrition with central-alimentation and the enterostomy can be closed safely when the patient's body weights is more than 2.3 kg.
Recently, the survival rates of extremely low-birth-weight (ELBW) infants have improved with the development of neonatal intensive care. However, these infants were susceptible to intestinal perforation due to prematurity, fluid restriction, and injection of indomethacin, etc. Because of the risks of transportation, anesthesia and surgery itself, peritoneal drainage has been compared with laparotomy. Through our experience, we investigate the usefulness of peritoneal drainage retrospectively. From 1997 to 2007, six ELBW (M:F=5:1) underwent primary peritoneal drainage for intestinal perforation. Their median birth weight was 685 g (405~870) and gestational age was 25+1 weeks (24+3~27+0). We noticed the intestinal perforation at median 10.5 days (8~18) after birth, and placed Penrose drain or Jackson-Pratt drain through right lower quadrant incision under local anesthesia. The cause of intestinal perforation was necrotizing enterocolitis in one patient, but that of the others was not clear. Three patients who showed normal platelet count and stable vital signs recovered uneventfully. Two patients (birth weight less than 500 g) who showed unstable vital signs and low platelet count (12,000 / mm3 to 30,000 / mm3) expired despite aggressive resuscitation. One patient required laparotomy due to persistent intestinal obstruction after drain removal and survived. Our experience shows that peritoneal drainage was an acceptable treatment for ELBW infants and the prognosis was related to vital sign and platelet count at the time of intestinal perforation, and birth weight.
A nationwide survey on necrotizing enterocolitis (NEC) was undertaken among members of the Korean Association of Pediatric Surgeons. The members were required to complete a questionnaire and the case registration form for each patient during the three-year period from July 2001 to June 2004. Eighty one patients were included in the questionnaire, but only 71 patients were registered from 22 members in 16 hospitals. At the same time survey on focal intestinal perforation (FIP) was undertaken and 17 patients were registered from 11 members in 10 hospitals. Total 19,041 newborns were admitted to neonatal intensive care unit during the study period. Eighty one patients (17.27 %) were underwent surgery among 469 babies who were managed under the impression of NEC. The male to female ratio was 2.1:1. The premature were 60.6 %. The most common site of involvement was ileum. Overall and operation survival of NEC were 72 % and 79 %, respectively. The survival was lower in smaller babies, multiple segments involvement and involvement of both the small and large intestine. But there was no difference in survival according to sex or prematurity. The FIP showed very similarity with NEC in terms of incidence, and the age of diagnosis and operation. But the survival was much better and 100 %. The results showed the clinical characteristics of NEC and the trend of management in NEC in Korea. In the future we hope we can discuss about this topic in prospective manner.
Gastric perforation of newborn is a rare, serious, and life threatening problem. The pathogenesis of gastric perforation is less well understood, and ranges widely. That ischemia is responsible for intestinal perforation enhances the likelihood that a similar mechanism exists for gastric perforation. Twelve patients with neonatal gastric perforation who were treated upon at the Department of Pediatric Surgery, Hanyang University Hospital from 1987 to 2002 were reviewed. Eight patients were male and four female. The age of perforation was 1 day to 8 days of life. Ten patients undertook operation and 2 patients were treated conservatively. The perforation site was located at the anterior wall along the greater curvature of the stomach in 8 patients and along the lessor curvature of the stomach in 2. The precipitating factors were gastroschisis, premature baby on ventilator and mechanical intestinal obstruction each 2 cases, and cyanotic heart disease and indomethacine medication each one case. In 5 cases the cause of perforation was not identified. The mortality rate was 25%(3 of 12). Earlier recognition and treatment were throught to be crucial prognostic factors.
Spontaneous gastric perforation in the newborn is a rare disease that requires early diagnosis and prompt surgical treatment. Between 1988 and 2001 at the Department of Pediatric Surgery, Kyungpook National University Hospital, 9 cases of spontaneous gastric perforation were treated. Seven were males and two females. The mean gestational age and birth weight were 36.7 weeks and 2,455 grespectively. All patients presented with severe abdominal distention and pneumoperitoneum on cross table lateral film of the abdomen. Perforations were located on the anterior wall along the greater curvature of the stomach in six and on the posterior wall along the greater curvature in two. One case showed two sites of perforation on the anterior and posterior wall along the greater curvature. Six patients were managed with debridement and primary closure and the others with debridement and partial gastrectomy. Peritoneal drainage was not performed. There were four deaths; two from sepsis due to leakage from the anastomotic site, one as a result of acute renal failure, and the other by associated respiratory distress syndrome. Spontaneous gastric perforation in the newborn is usually located along the greater curvature. Elevated intragastric pressure is a possible cause of the perforation. Poor prognosis is related to associated diseases and prematurity.
Meckel's diverticulum (MD) occurs in approximately 2 % of the population. The major complications of MD are bleeding, intestinal obstruction, infection and perforation. Perforation is the least common but most serious complication, the incidence od which is about 5-10 %. The causes of perforation are inflammatory diverticulitis and peptic ulceration. the purpose of study is to review the characteristics of perforated MD in children. Six patients with perforated MD who had been operated upon at the Department of Pediatric Surgery, Yeungnam University Hospital from April 1984 to July 2001 were included. Male predominated in a ratio of 5:1 and there were 2 neonates. The chief complaints were abdominal pain and distension. Half of the children showed a past history of bloody stools. The average age was 4 year and 9 months. The mean distance from the ileocecal valve to the diverticulum was 60 cm. Average length of the diverticulum was approximately 3 cm and width was 1.7 cm. The perforation site was the tip of the diverticulum in 3 cases, the base in 2 cases and along the lateral border in one. In two patients, ectopic gastric mucosa was found in the specimen. All of the patients were operated upon with a diagnosis of peritonitis of unknown etiology. In conclusion, when a child shows symptoms of acute abdomen or peritonitis, especially in boys, with the history of bloody stools and episodic abdominal pain, perforated MD should be suspected.
Idiopathic small bowel ulceration distal to the duodenum is rare. Less than 5 % of the reported cases were in children. In the majority of the patients, a single ulcer of unknown cause is found in the jejunum or ileum. The diagnosis is difficult and usually made at the time of surgical exploration for complications, such as perforation, hemorrhage or obstruction. We treated a pediatric patient with perforation of an idiopathic ileal ulceration. The child was an ll-year-old boy who sustained blunt abdominal trauma. The involved ileal segment was resected. Pathologic findings were compatible with idiopathic small bowel ulceration. The clinical and pathological aspects of idiopathic ulcerations are discussed, and the literature reviewed.
Appendiceal perforation is uncommon in the neonate. Diess reported the firs case in 1908. Approximately HI additional cases have been reported since that time. However, with exclusion of neonatal appendicitis' associated with inguinal or umbilical hernias, n,ecrotizing enterocolitis, meconium plug, and Hirschsprung's disease, there are only 36 cases of primary neonatal appendicitis. We treated a 12 days old boy with perforation of the appendix. The infant was 3000 g at birth and had a normal spontaneous vaginal delivary at 35 weeks of gestation. The mother was 31-year-old and had premature rupture of membrane. After normal feeding for the first 5 days of life, the infant had emesis of undigested milk, decreased activity and jaundice. The baby was admitted to the Pediatrics. Progressive abdominal distension, fever, decreased activity, and vomitting developed over the next six days. Erect abdominal radiography showed pneumoperitoneum. At exploratory laparotomy, a 0.8 × 0.6 em sized perforation was noted at antime-senteric border of midportion of the appendix. Trasmural inflammation and the presence of ganglion cells were noticed on histology.
Perforation of the gastrointestinal tract in neonatal period has been associated with a grim prognosis. Recently there has been some improvement in survival. To evaluate the remaining pitfalls in management, 19 neonatal gastrointestinal perforation cases from May 1989 to July 1996 were analysed retrospectively. Seven patients were premature and low birth weight infants. Perforation was most common in the ileum{56.3%). Mechanical or functional obstruction distal to the perforation site was identified in 7 cases; Hirschsprung's disease 3, small bowel atresia 3, and anorectal malformation 1. These lesions were often not diagnosed until operation. Five cases of necrotizing enterocolitis and 1 of muscular defect were the other causes of perforation. In six cases, the cause of the perforation was not identified. Perinatal ischemic episodes were associated in five cases. Overall mortality was 15.1 %. Because a considerable number of gastrointestinal perforations resulted from distal obstruction, pediatric surgeon should be alert for early identification and intervention of gastrointestinal obstruction, particularly in patients that are premature and have a history of ischemia..
Hyperimmunoglobulin E syndrome is a relatively rare primary immunodeficiency syndrome characterized by recurrent infection, abscess formation and marked elevation of serum IgE level. The common infectious organism is Staphylococcus aureus and recurrent infection indicates some defects in the immunologic system. Although the infection can affect various organs, gastrointestinal tract involvement is rare and only one case of colon perforation has been previously reported. Herein we report another one case of colon perforation which ocurred in an 8-year-old girl with hyperimmunoglobulin E syndrome. The patient was admitted to the hospital due to an abscess on right neck. The diagnosis of hyperimmunoglobulin E syndrome was made because she had eczematoid dermatitis on the face, pneumatocele on left upper lung field and markedly elevated serum Ig E level(> 15,000 IV/ml) with a past histories of frequent scalp abscesses and otitis media. Abdominal pain developed on the 13th day of admission and abdominal plain X-ray revealed free air. An exploratory laparatomy was performed and two free perforations of the transverse colon were noted. Segmental resection and double barrel colostomy were performed. Colostomy closure was done 4 month later and she had no gastrointestinal problem during a follow up period of 15 months.
Spontaneous perforation of the bile duct in children is a very rare disorder. We experienced a 6 year-old girl with spontaneous perforation of the right hepatic duct. The patient was initially misdiagnosed as hepatitis because of elevation of liver enzyme and then as appendicitis because of fluid collection in the pelvic cavity demonstrated by ultrasonogram. A laparoscopic exploration was done and no abnormal findings were detected except bile-stained ascites. Peritoneal drainage was performed and the patients seemed to improve clinically. Abdominal pain, distention and high fever developed after removal of the drains. DISIDA scan showed a possible of bile leak into the peritoneal cavity. ERCP demonstrated free spiil of dye from the right hepatic duct. At laparotomy, the leak was seen in the anterior wall of the right hepatic duct 2cm above the junction of the cystk duct and common hepatic duct. The perforation was linear in shape and 0.8cm in size. The patient underwent cholecystectomy, primary closure of the perforation and T-tube choedochostomy. We could not identify the cause of the perforation; however, the T-tube cholangiography taken on the 42nd postoperative day showed a little more dilatation of the proximal common bile duct compared with the cholangiography taken on the 14th day. Long-term follow-up of the patient will be necessary because of the possibility for further change of the duct.
Spontaneous gastric perforation is an important but rare cause of gastrointestinal perforation in neonates. Just over 200 cases have been reported in the literatures. In spite of recent surgical advances in its managements, mortality rate has been reported as high as 25~50%. Because of physiologic differences, immature immune mechanisms, variations in gastrointestinal flora and poor localization of perforation, a neonate with gastric perforation is at high risk. The pathogenesis is greatly debated. Five patients with spontaneous neonatal gastric perforation who were operated upon at the Department of Pediatric Surgery, Seoul National University Hospital from 1980 to 1993 were reviewed. Four patients were male and one female. The first indication of perforation was 1 day to 6 days of life. All of 5 perforations were located along the greater curvature of the stomach. The size of perforation ranged from 2 cm to 10 cm. Debridement and primary closure were performed in all patients. The operative mortality was 40%(2 of 5). The cause of perforation was not identified in all cases. Prematurity and necrotizing enterocolitis, synchronous or metachrotlous, were thought to be crucial prognostic factors. Earlier recognition and surgical intervention are necessary to reduce morbidity and mortality.
Children tend to ingest foreign bodies. The majority present in children between the ages of 6 months and 3 years. We experienced 2 cases of unusual gastrointestinal complications caused by ingested foreign bodies. First case was a 10-month-old male with intestinal perforation due to two pieces of ingested magnetic beads. Second case was a 7-month-old girl with esophageal stricture due to an ingested particle of plastic toy.
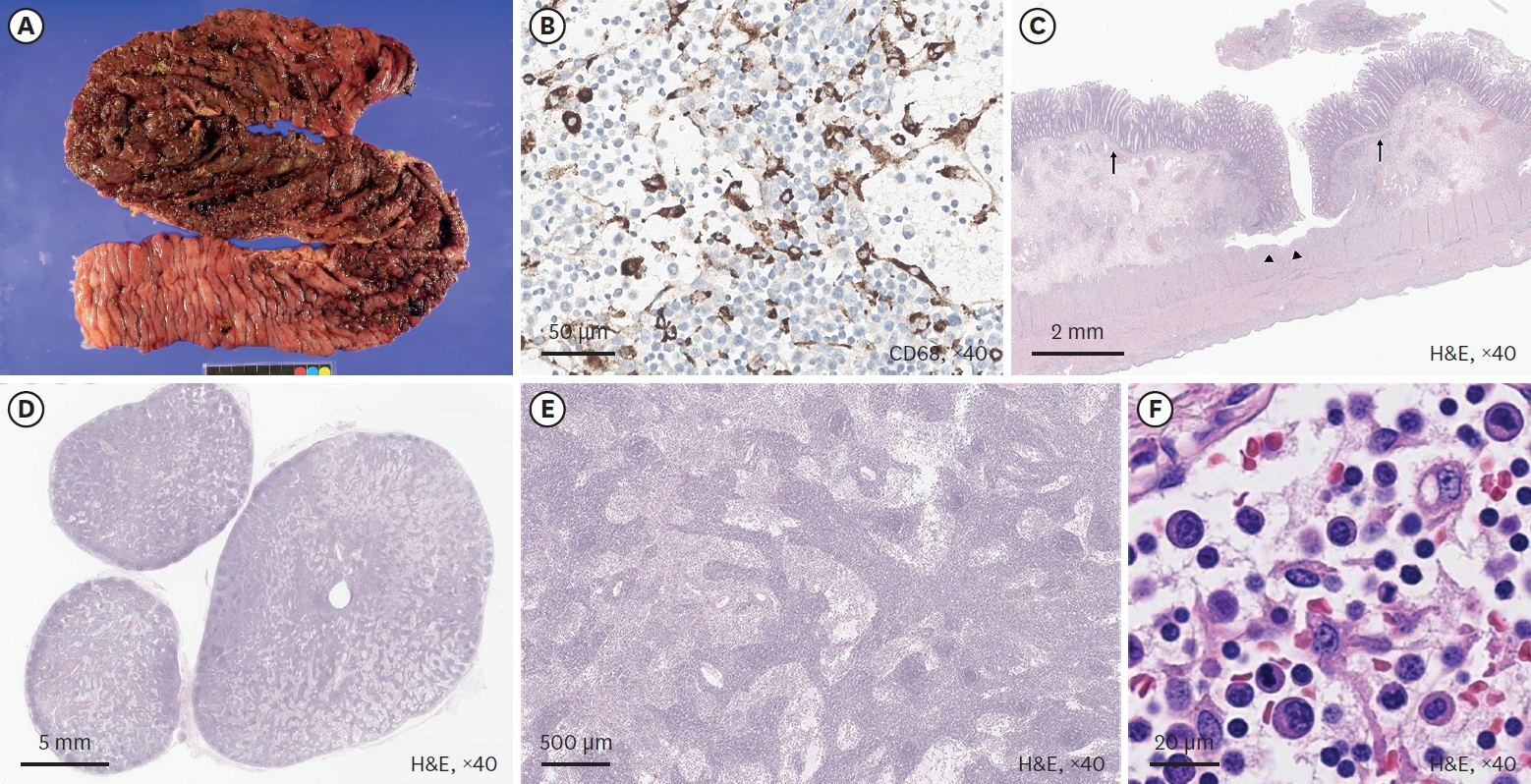
Neonatal intestinal perforation is mainly caused by necrotizing enterocolitis, intestinal atresia, meconium ileus or unknown etiology. Occasionally, Hirschsprung's disease presents with neonatal intestinal perforation, of which, it is known that total colonic aganglionosis is common. Therefore, Hirschsprung's disease should be considered as a cause of neonatal intestinal perforation.
The authors have experienced 3 cases of neonatal Hirschsprung's disease associated with colonic perforations. Cecal perforations were noted in 2 cases with aganglionosis from descending colon and sigmoid perforation in a case with aganglionosis in rectum. These cases will be discussed with literature review.

