INTRODUCTION
Ascariasis is a parasitic infection caused by Ascaris lumbricoides (AL), a nematode that can grow to be 25–35 cm long and is transmitted through the fecal-oral route. Ascariasis has a global prevalence of 25%. It is prevalent in India, China, Africa, and Latin America. In Korea prevalence 2.6% and Japan is only 0.04%. It is estimated that there are 4 million infected individuals in North America. The prevalence in children in tropical and subtropical countries is 70% [
1,
2].
Hepatobiliary ascariasis (HA) is caused by the invasion and migration of the nematode AL into the biliary ducts in the presence of a large number of parasites in the intestine. Clinical manifestations may include biliary colic, cholangitis, cholecystitis, liver abscess, or acute pancreatitis. Ultrasound is a useful tool for identifying nematodes in intestinal and biliary tract. Initial treatment includes antihelminthic drugs, antibiotics, pain medications; however if AL persists in the biliary tract for more than three weeks or if the parasites are dead, extraction should be considered, which can be performed endoscopically or surgically [
1-
10].
CASE REPORT
1. Case 1
A six-year and 10-month-old indigenous female patient was admitted with an eight-day history of right hypochondrial abdominal pain. Abdominal ultrasonography revealed multiple mobile hyper-echoic longitudinal images of the gallbladder and intrahepatic bile ducts identified as AL. Hemogram revealed 18,800 leukocytes (77% segmented, 5.2% eosinophils), alkaline phosphatase (ALP) 901 IU/L, gamma-glutamyl transferase 397 U/L. Anthelminthic and antibiotics were prescribed for ascending cholangitis. After eight days, the pain intensity increased, and because there was no equipment available for endoscopic retrograde cholangiopancreatography (ERCP), the patient was transfer to the operating room for laparoscopic AL extraction. Twenty adult AL were extracted from common bile duct, common hepatic duct, and left and right hepatic ducts. The patient's condition improved satisfactorily without complications. Control ultrasound reported absence of AL in bile ducts and liver function tests returned to normal values.
2. Case 2
Ten-month-old male patient was brought to the emergency department with vomiting, diarrhea, and abdominal pain. Abdominal ultrasonography revealed a liver abscess and AL in the biliary tract, prompting initiation of anthelminthic and antibiotic treatment for the liver abscess. Hemogram revealed 19,390 leukocytes (segmented 17%, eosinophils 20%), ALP 429 IU/L, gamma-glutamyl transferase 184 U/L. A follow-up ultrasound at eight days showed persistent mobile AL in the biliary tract and associated pain crisis; therefore the patient was scheduled for laparoscopic extraction of AL from the biliary tract because there was no equipment available for ERCP and the pain increased. Twelve adult AL were removed from the common bile duct, common hepatic duct and left and right hepatic ducts. The patient showed a good postoperative recovery with liver function tests in normal values.
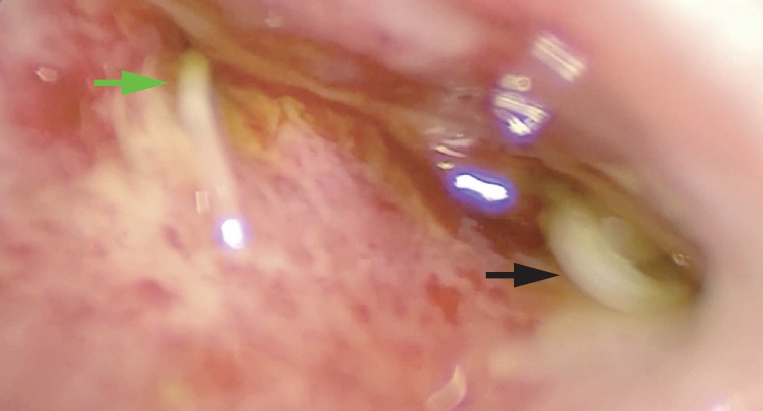
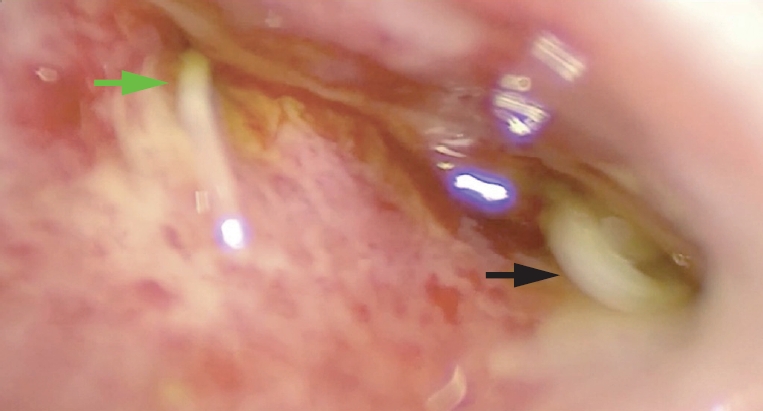
A 10 mm umbilical trocar was placed using an open technique, and a 5 mm trocar was placed in the epigastrium, right hypochondrium, and right iliac fossa. Diagnostic laparoscopy was performed to identify the gallbladder and bile duct. The 5 mm clips were placed on the cystic duct and sectioned to allow greater mobility of the common bile duct. Two traction sutures were placed percutaneously at the level of the common bile duct towards the abdominal wall. A common bile duct incision was performed and AL extraction was initiated (
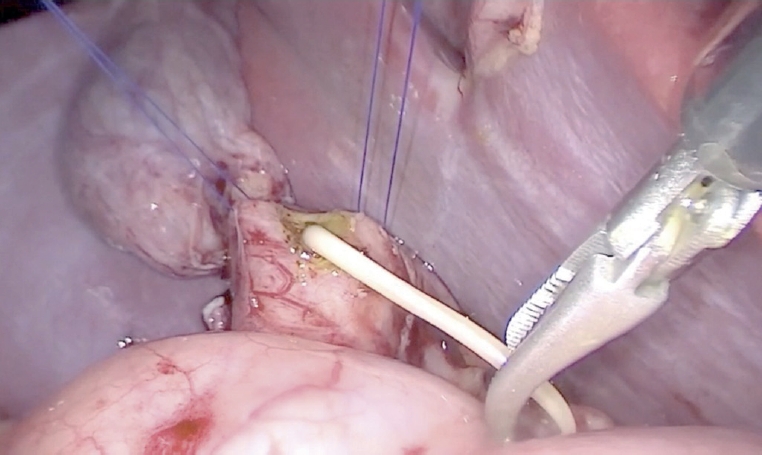
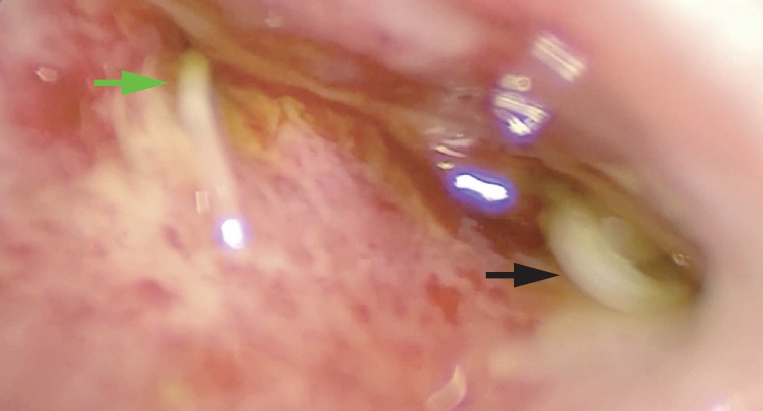
Fig. 1). A 5 mm lens was introduced into the common bile duct to verify complete extraction of AL. More AL was identified within the right and left hepatic ducts, which were removed using a 5 mm Maryland clamp (
Fig. 2). Both hepatic ducts were irrigated with saline solution until no parasites were detected. Intersurgical cholangiography was performed to ensure that the intrahepatic bile duct was free of filling defects. The common bile duct incision was closed and cholecystectomy was performed. A drain was placed and removed after seven days with no evidence of bile leakage.
In the second case the same surgical technique described above was performed; however due to the patient's size, a 5 mm trocar at the umbilical and epigastric levels and a 3 mm trocar in the right hypochondrium and right iliac fossa were used.
3. Ethical compliance
All procedures performed in this report involving human participants were in accordance with the ethical standards of the institution.
DISCUSSION
Ascariasis is a condition present in 25% of the world's population, the prevalence in children in tropical and subtropical countries is 70%. Invasion and migration of AL into the biliary ducts can cause biliary colic, cholangitis, cholecystitis, liver abscess, or acute pancreatitis [
1,
2].
Standard treatment of biliary ascariasis includes antihelminthic drug therapy with mebendazol or albendazol with success rate up to 80%. However, it is not advisable to have dead worms inside the ductal system, which might lead to stricture formation as a result of severe inflammatory reaction. In addition, the liberated ova or existence of fragmented ascaris might act as a nidus for stone formation. Therefore, for the above-mentioned reasons and in failed medical treatment of confirmed biliary ascariasis, endoscopic intervention is indicated. Surgical intervention with worm extraction from bile ducts combined with cholecystectomy should be advised for patients for whom conservative and endoscopic management has failed or complicated by cholangitis [
1,
4,
6].
In the cases presented, the surgical indication was the increase in abdominal pain, the presence of liver abscess and clinical and laboratory data of ascending cholangitis. At that time we did not have the possibility of ERCP.
A cholecystectomy was performed because the patient had AL in the gallbladder, which did not resolve despite antihelminthic treatment; therefore, a cholecystectomy was indicated. Laparoscopic extraction of AL from the biliary tract has been reported in adult patients, this is the first report cases in a pediatric settings. Although there are only two cases, the surgical technique proved to be a safe and reproducible method for resolving HA in pediatric patients when antihelmintic drug. It is not effective and ERCP is not available.
NOTES
-
Conflict of Interest
No potential conflict of interest relevant to this article was reported.
Fig. 1.A common bile duct incision was performed and Ascaris lumbricoides extraction was initiated.
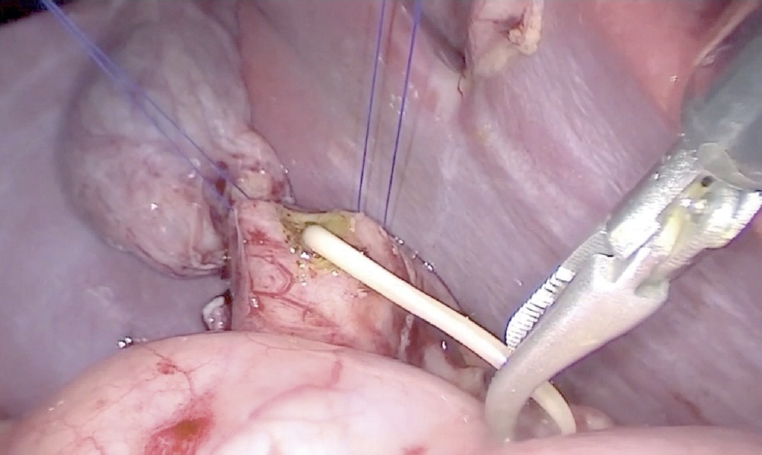
Fig. 2.
A 5 mm lens was introduced into the common bile duct to verify complete extraction of AL. More AL was identified within the right (green arrow) and left hepatic ducts (black arrow).
AL, Ascaris lumbricoides.
REFERENCES
- 1. Khuroo MS, Rather AA, Khuroo NS, Khuroo MS. Hepatobiliary and pancreatic ascariasis. World J Gastroenterol 2016;22:7507-17.
- 2. Canes M, Seaton C, Mawson J, Goldfarb DM, Kang KT. Biliary ascariasis and trisomy 21 in a child newly arrived to Canada. CMAJ 2022;194:E1318-21.
- 3. Roy K, Das J, Mukherjee D, Kundu R. Pancreatic-biliary ascariasis in an infant. J Nepal Paediatr Soc 2017;37:98-100.
- 4. Hajaji K, Aljohary H, Althani H. Laparoscopic management of biliary ascariasis: a case report and review of literature. World J Lap Surg 2010;3:113-5.
- 5. de Almeida BL, Silva DV, do Rosário MS, Gonçalves BSD, Nunes MG, Ney ALCM, et al. Biliary ascariasis and severe bacterial outcomes: report of three cases from a paediatric hospital in Brazil. Int J Infect Dis 2020;95:115-7.
- 6. Cai M, Cheng J, Li W, Shuai X, Gao J, Cai K, et al. Combination of laparoscope and choledochoscope to treat biliary ascariasis: a CARE-compliant case report. Medicine (Baltimore) 2017;96:e6291.
- 7. Temesgen R, Abebe H, Abera Y. Hepatobiliary and pancreatic duct ascariasis: an unusual cause of obstructive jaundice and severe acute cholangitis. Int Med Case Rep J 2022;15:281-6.
- 8. Anand M, Topno N, Hajong R, Baruah AJ, Khongwar D, Agarwal S. Surgical manifestations and management of gastrointestinal and hepato-pancreatobiliary ascariasis: an observational study. Int Surg J 2020;7:3620-2.
- 9. Jethwani U, Singh GJ, Sarangi P, Kandwal V. Laproscopic management of wandering biliary ascariasis. Case Rep Surg 2012;2012:561563.
- 10. Hong ST, Yong TS. Review of successful control of parasitic infections in Korea. Infect Chemother 2020;52:427-40.
Citations
Citations to this article as recorded by