ABSTRACT
Intrapulmonary bronchogenic cysts are rare congenital anomalies that often present diagnostic and management challenges due to nonspecific symptoms. We report a one-year-old female with progressive respiratory distress who was initially misdiagnosed with pneumothorax. Imaging revealed a large intrapulmonary cyst, and surgical excision confirmed the diagnosis. Early intervention ensured a favorable outcome, with no recurrence in one year. This case highlights the importance of considering bronchogenic cysts in pediatric respiratory distress and emphasizes the value of timely surgical management.
-
Keywords: Bronchogenic cyst; Infant; Respiratory Insufficiency; Thoracotomy
INTRODUCTION
Bronchogenic cysts are congenital malformations arising from abnormal budding of the foregut. Typically lined with ciliated respiratory epithelium, these cysts may also contain cartilage, smooth muscle, and mucosal glands. Mediastinal bronchogenic cysts account for most cases, while intrapulmonary cysts represent approximately 15%–20% of all bronchogenic cysts. These intrapulmonary cysts often communicate with the bronchial tree, and nearly two-thirds are aerated. Intraparenchymal cysts consistently present with respiratory epithelium and cartilage [
1].
The clinical manifestations of bronchogenic cysts vary widely, ranging from asymptomatic lesions to severe respiratory distress. Presentation depends on the size, location, and presence of complications such as infection or rupture. Imaging plays a crucial role in diagnosis, offering detailed anatomical visualization; however, definitive diagnosis requires histopathological confirmation.
This case report describes an infant with an intrapulmonary bronchogenic cyst, highlighting the diagnostic challenges, surgical management, outcomes, and relevant literature.
CASE REPORT
A one-year-old female presented with a one-month history of progressive respiratory distress, which had worsened over two days. She was born full-term, with an unremarkable perinatal history. On examination, she exhibited tachypnea and decreased air entry in the right lung field. Oxygen saturation was 85% on room air, improving with supplemental oxygen.
At an outside hospital, an intercostal drain (ICD) was inserted for suspected pneumothorax, and conservative treatment was provided for five days. Due to persistent symptoms and failure of lung expansion, she was referred to our center for further evaluation.
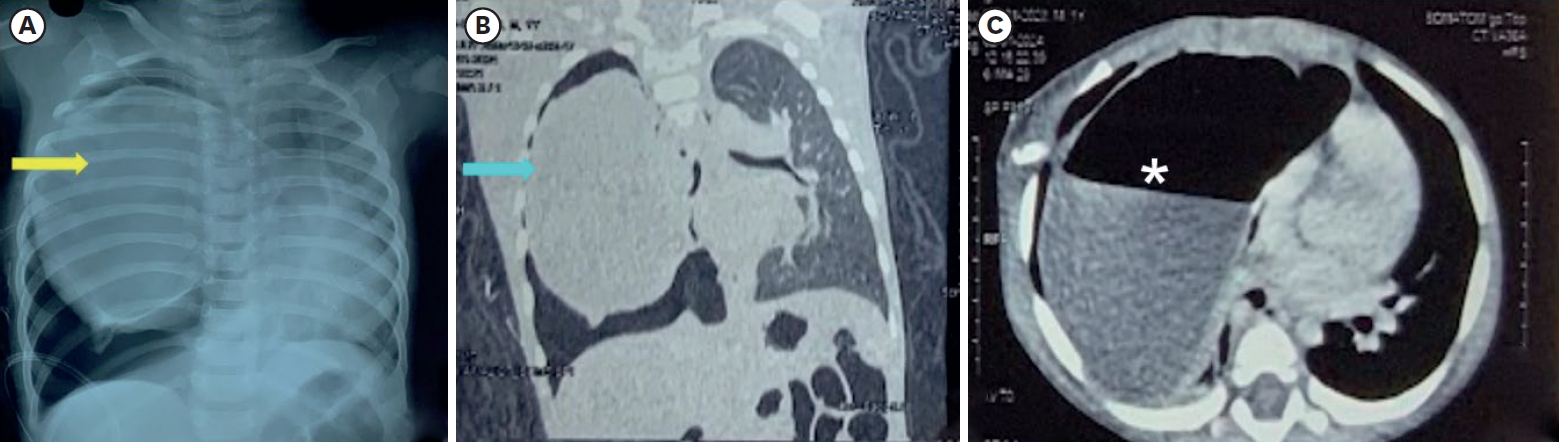
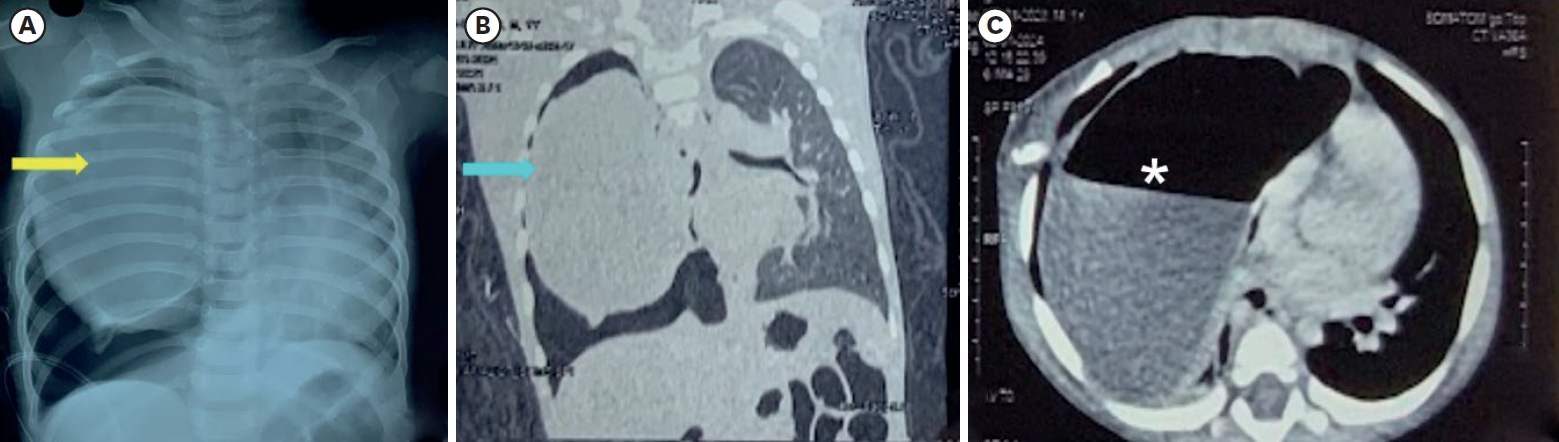
A chest radiograph showed a space-occupying lesion in the right hemithorax (
Fig. 1A). High-resolution computed tomography (CT) (
Fig. 1B and
C) revealed a large cystic lesion measuring 8.8 cm × 8 cm × 6 cm in the right hemithorax, with air-fluid levels in the mid and lower zones, causing a mediastinal shift to the left. Additional smaller cysts were noted but no aberrant vessels were identified. A provisional diagnosis of congenital pulmonary airway malformation (CPAM) versus bronchogenic cyst was made.
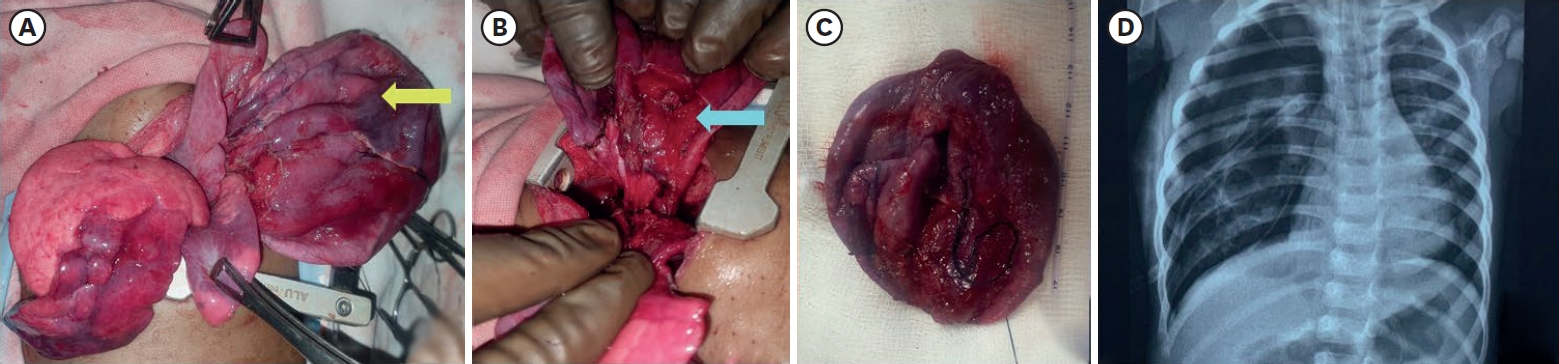
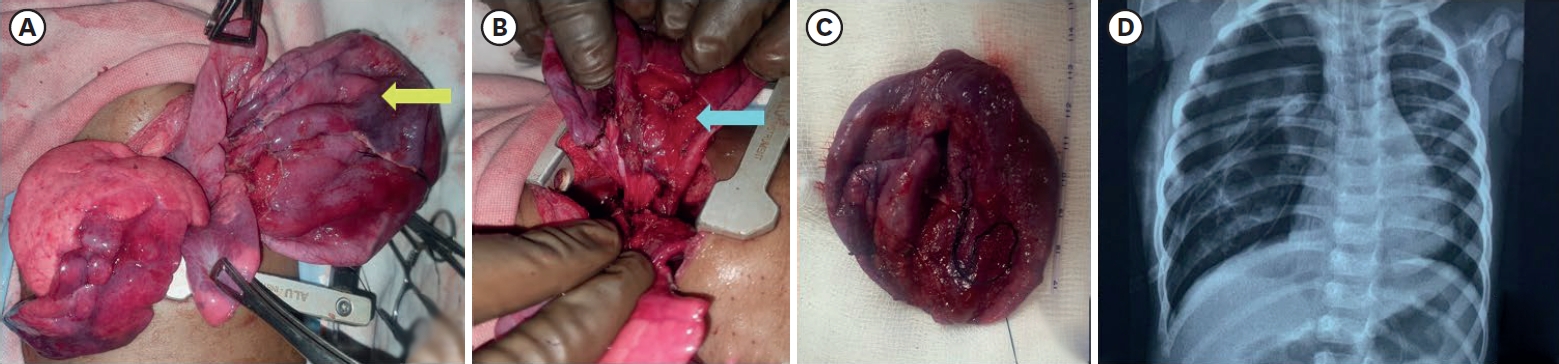
After stabilization, surgical exploration was performed. A right thoracotomy through the fifth intercostal space revealed a large cystic lesion separate from the upper, middle, and lower lobes but within the visceral pleura (
Fig. 2A and
B). The cyst contained approximately 100 mL of purulent fluid. Surrounding tissues were inflamed and highly vascular. The cyst was completely excised (
Fig. 2C), and the thoracic cavity was closed after irrigation and a chest tube placement.
Postoperatively, the child was extubated after 24 hours. A chest radiograph (
Fig. 2D) showed full expansion of the right lung. The ICD was removed on postoperative day five, and she was discharged on postoperative day seven.
Histopathological analysis confirmed an intrapulmonary bronchogenic cyst, with a 2 mm-thick wall lined by pseudostratified ciliated columnar epithelium. The stroma included cartilage, smooth muscle, and bronchial glands. Chronic inflammatory infiltrates consistent with secondary infection were also noted.
She remained asymptomatic at follow-up visits at three weeks, three months, six months, and one year.
DISCUSSION
Bronchogenic cysts pose significant diagnostic challenges due to their nonspecific presentations and overlap with other thoracic pathologies. A literature review was conducted using PubMed, Google Scholar, and Scopus, including English-language articles published until April 2025. Search terms included “bronchogenic cyst,” “intrapulmonary,” “infant,” “pediatric lung cyst,” and “congenital pulmonary malformations.” Relevant case reports, case series, and reviews were included (
Table 1) [
2-
7].
Bronchogenic cysts result from abnormal budding of the ventral foregut between days 26 and 40 of gestation. Their location varies based on timing of separation from the airways, with most found in the middle mediastinum near the carina. Less commonly, they occur in paratracheal, hilar, posterior or anterior mediastinal, diaphragmatic, intrapericardial, intracardiac, or even extrathoracic sites such as neck, skin and retroperitoneum.
Most bronchogenic cysts are diagnosed in adults aged between 20 to 40 years, and diagnosis in infants is rare [
8-
10]. Symptoms depend on the size, location, and complications. Common symptoms include cough, fever, dyspnea, and chest pain. Some infants present with persistent cough or recurrent infections, while others exhibit acute symptoms such as tachypnea or respiratory distress. Complications such as infection, rupture, or malignant transformation are more common in symptomatic cases [
8,
11]. Rare complications include superior vena cava obstruction, pneumothorax, dysphagia, severe hemoptysis, and malignant transformation. Our index case appears to be the only patient with preoperative misdiagnosis and ICD placement.
CT and magnetic resonance imaging (MRI) are essential diagnostic tools. CT scans typically reveal well-circumscribed cystic lesions, often with air-fluid levels in cases of infection or rupture [
12]. MRI provides superior soft-tissue differentiation, distinguishing bronchogenic cysts from other lesions, such as CPAM or abscesses. Findings from Singer et al. [
7] emphasized the role of contrast-enhanced imaging in delineating cystic boundaries and identifying complications. Almatrafi et al. [
11] described cases of bronchogenic cysts presenting with air-fluid levels on imaging, a finding consistent with our case.
CPAM and congenital lobar emphysema (CLE) are common differentials for bronchogenic cysts in infants. CPAM typically appears as multicystic or mixed solid-cystic lesions with bronchial communication, whereas bronchogenic cysts are unilocular, well-circumscribed, and lack internal septations. CLE shows hyperinflated lung segments with reduced vascular markings distinguishable by CT. Infected bronchogenic cysts may mimic lung abscesses or infected bullae, but differ by having thinner, smoother walls and minimal enhancement unless infected. Pericardial, esophageal duplication, and neurenteric cysts may resemble bronchogenic cysts near the hilum or mediastinum but differ in location and tissue characteristics. MRI aids diagnosis by differentiating cyst content signal intensities; proteinaceous or hemorrhagic cysts show high T1 signal and hyperdense CT appearances that may mimic solid nodules, requiring further imaging or excision.
Surgical excision for symptomatic patients remains the treatment of choice. Complete excision prevents recurrence and complications such as infection or malignancy. There are various methods for treatment, including transbronchial aspiration essentially for acute cyst decompression and for non-surgical candidates and resection by open thoracotomy, mediastinoscopy and video-assisted thoracoscopy. Video-assisted thoracoscopic resection has emerged as a viable approach and with the adoption of the robotic platform for minimally invasive thoracic surgery, thoracoscopic resection has become more feasible [
13,
14]. Almatrafi et al. [
11] reported managing such cases using minimally invasive surgical techniques, underscoring the need for individualized approaches depending on cyst size and location. Surgical option should be individualized, considering cyst size, infection status, patient age, and surgeon experience.
The management of asymptomatic or incidentally detected bronchogenic cysts remains a subject of debate. While some advocate observation with periodic imaging in select asymptomatic cases, most pediatric surgeons recommend elective surgical excision due to the potential risks of infection, progressive enlargement, airway compression, or rare malignant transformation.
Lung development continues well into postnatal life, with alveolarization and microvascular maturation progressing significantly during the first 2–3 years after birth. The presence of a space-occupying lesion like a bronchogenic cyst during this critical window can impair normal lung expansion and alveolar growth, potentially resulting in long-term pulmonary compromise. Early surgical excision of the cyst not only resolves the immediate mechanical obstruction but also facilitates optimal lung re-expansion and growth, supporting better respiratory outcomes in the long term. In infants and young children, where the clinical course can change unpredictably, early surgery is generally favored to prevent complications and achieve definitive diagnosis and cure [
15,
16].
Histopathological findings remain the cornerstone of diagnosis and characteristic findings include ciliated respiratory epithelium lining, smooth muscle, mucous glands, and cartilage [
7]. These features distinguish bronchogenic cysts from congenital anomalies such as enteric or dermoid cysts. Pulmonary lymphangiomas show dilated lymphatic channels lined by flattened endothelial cells, lung abscesses reveal necrosis with inflammatory infiltrates but no epithelial lining, and infected bullae lack alveolar epithelium and show fibrotic lung changes. Pericardial cysts feature mesothelial lining with clear fluid, spinal neurenteric cysts contain gastrointestinal-type epithelium, and solid-appearing cyst contents require exclusion of neoplasms by identifying cellular atypia and disorganized architecture.
Untreated bronchogenic cysts are prone to complications, including infection, rupture, and malignant transformation, although the latter is rare. The long-term prognosis for intrapulmonary bronchogenic cysts following complete surgical excision is generally excellent. Most patients remain asymptomatic, with full pulmonary recovery and normal development, particularly when surgery is performed early. However, infants and young children may benefit from extended clinical follow-up due to the potential for subclinical complications or delayed respiratory sequelae.
Recurrence of bronchogenic cysts is rare but has been reported, typically in cases where excision was incomplete or cysts had significant adhesions to surrounding structures. Recurrence may present months or even years after surgery, emphasizing the need for careful intraoperative dissection and postoperative surveillance through imaging [
17]. Periodic follow-up imaging may be considered, especially in complex or multiloculated cysts. Although uncommon, late complications can include secondary infection, compression of adjacent lung or airway structures, and, in extremely rare cases, malignant transformation [
18,
19].
Managing bronchogenic cysts often requires a multidisciplinary approach involving pediatricians, radiologists, and pediatric surgeons. Early and accurate diagnosis is critical to guiding appropriate treatment strategies and preventing complications such as infection, rupture, or airway obstruction. In this case, a collaboration between specialties facilitated timely surgical intervention and a favorable outcome.
Our case exemplifies the diagnostic challenges posed by intrapulmonary bronchogenic cysts in infants. The initial clinical presentation with progressive respiratory distress mimicked pneumothorax, leading to chest tube insertion, which did not improve symptoms. This highlights the importance of considering bronchogenic cysts in the differential diagnosis of persistent respiratory distress in infancy, especially when symptoms fail to respond to standard interventions. Cross-sectional imaging modalities such as CT proved invaluable in revealing the cystic lesion’s size, localization, and extent, guiding prompt surgical intervention. Early thoracotomy and complete cyst excision resulted in an excellent clinical outcome without recurrence at one year follow-up. This case reinforces the clinical message that high suspicion and judicious imaging can prevent misdiagnosis and enable timely definitive management, improving morbidity and long-term pulmonary prognosis in affected infants.
Intrapulmonary bronchogenic cysts are exceedingly rare in infants, and ours appears to be the only case with preoperative misdiagnosis and ICD placement. This case underscores the importance of considering bronchogenic cysts in the differential diagnosis of pediatric respiratory distress. Early recognition and surgical intervention are critical for preventing complications and achieving favorable outcomes.
NOTES
-
Conflict of Interest
No potential conflict of interest relevant to this article was reported.
-
Author Contributions
Conceptualization: B.R., S.S., D.S., P.N.J., M.J.K.; Data curation: S.S.; Writing - original draft: B.R., S.S., D.S., P.N.J., M.J.K.
Fig. 1.
Radiologic findings.
(A) Chest radiograph at the time of admission showing a cystic lesion in the right hemithorax causing mediastinal shift along with right pneumothorax probably secondary to the chest tube insertion (yellow arrow indicates the cystic lesion). (B) Coronal view of high-resolution computed tomography showing 8.8 cm × 8 cm × 6 cm smooth-walled cystic lesion occupying almost the entire right hemithorax (blue arrow indicates the cystic lesion). (C) Axial view of high-resolution computed tomography (mediastinal window) showing a cystic lesion with air-fluid level (asterisk) in the right hemithorax.
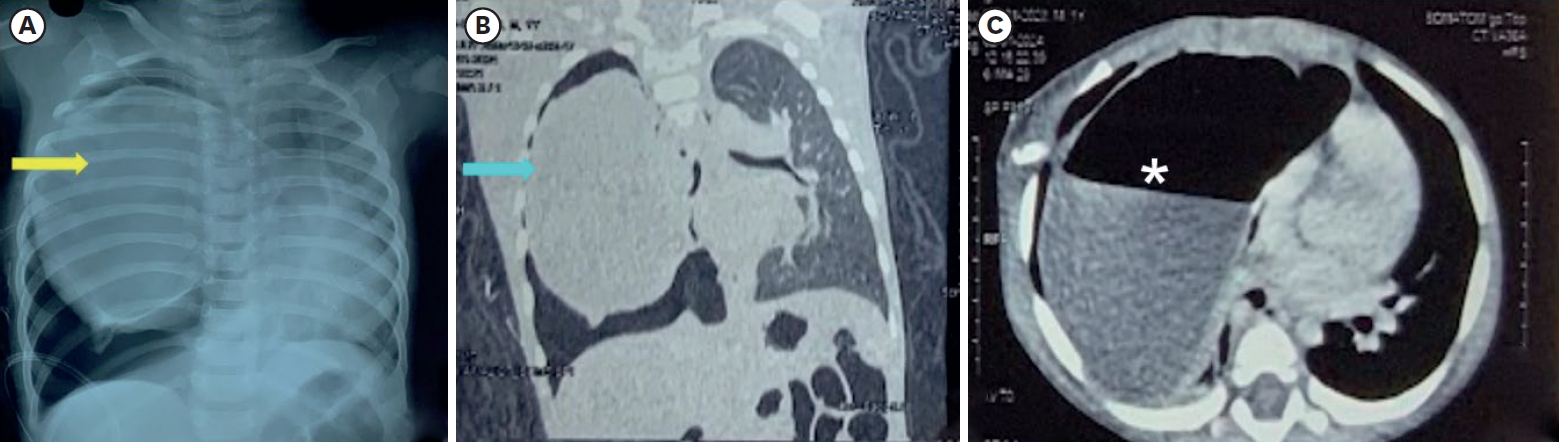
Fig. 2.
Operative findings and postoperative radiologic image.
(A) Intraoperative photograph showing the cystic mass (yellow arrow) separate from the normal lung parenchyma but within the visceral pleura. (B) Intraoperative photograph showing the cyst (blue arrow) after dissection. (C) Photograph of the excised cystic mass measuring 7.5 cm × 8 cm. (D) Post-operative chest X-ray showing the expanded right lung with a chest tube in situ.
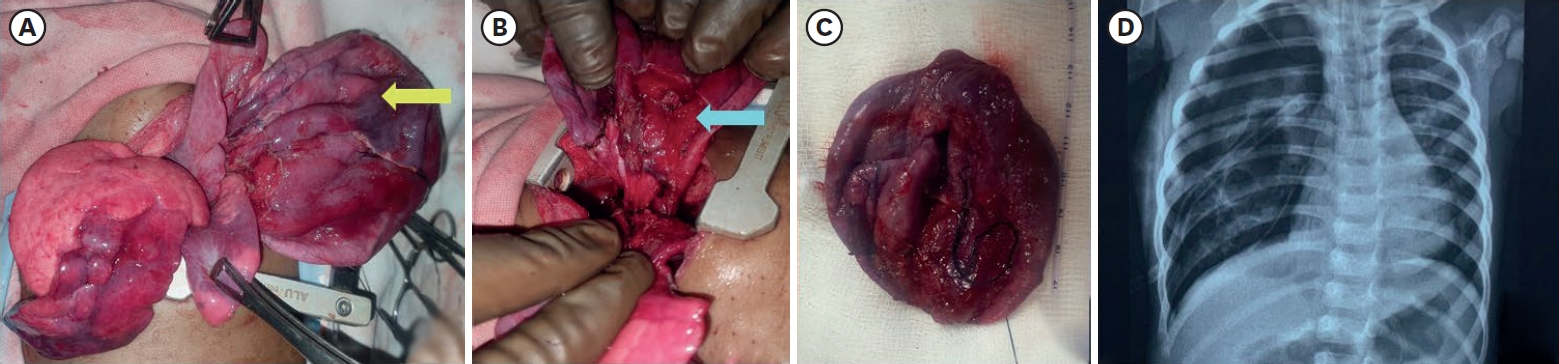
Table 1.Previously reported cases of intrapulmonary bronchogenic cysts in infants
Table 1.
|
Study No. |
Study |
Age/sex |
Presentation |
Cyst location |
Surgical intervention |
Outcome |
|
1 |
Di Lorenzo et al. (1989) [2] |
2 mo-1 yr |
Dyspnea, cyanosis, recurrent respiratory issues |
Mediastinal/ intraparenchymal |
Thoracotomy with excision or lobectomy |
Excellent |
|
2 |
Ribet et al. (1996) [3] |
Infant |
Respiratory distress, compression symptoms |
Various lobes |
Lobectomy or excision |
No recurrence reported |
|
3 |
Dembinski et al. (1999) [4] |
Neonate/male |
Prenatally diagnosed; respiratory distress |
Right lung |
Early postnatal surgery |
Excellent |
|
4 |
Al-Bassam et al. (1999) [5] |
1 day- 5 yr |
Respiratory distress, recurrent infections |
Mixed lobes |
Excision, lobectomy |
Mostly uneventful |
|
5 |
Bansal et al. (2017) [6] |
2 mo/male |
Antenatally diagnosed/ respiratory distress |
Left lower lobe |
Cyst excision |
Excellent |
|
6 |
Singer et al. (2022) [7] |
1 mo/male |
Recurrent infections, dyspnea |
Right middle lobe |
Open thoracotomy |
Excellent |
|
7 |
Current case (2024) |
1 yr/female |
Progressive respiratory distress |
Right middle lobe |
Open thoracotomy |
Excellent |
REFERENCES
- 1. Shields TW, LoCicero J 3rd, Reed CE, Feins RH. General thoracic surgery. 7th ed. Philadelphia (PA): Lippincott Williams & Wilkins; 2009.
- 2. Di Lorenzo M, Collin PP, Vaillancourt R, Duranceau A. Bronchogenic cysts. J Pediatr Surg 1989;24:988-91.
- 3. Ribet ME, Copin MC, Gosselin BH. Bronchogenic cysts of the lung. Ann Thorac Surg 1996;61:1636-40.
- 4. Dembinski J, Kaminski M, Schild R, Kuhl C, Hansmann M, Bartmann P. Congenital intrapulmonary bronchogenic cyst in the neonate--perinatal management. Am J Perinatol 1999;16:509-14.
- 5. Al-Bassam A, Al-Rabeeah A, Al-Nassar S, Al-Mobaireek K, Al-Rawaf A, Banjer H, et al. Congenital cystic disease of the lung in infants and children (experience with 57 cases). Eur J Pediatr Surg 1999;9:364-8.
- 6. Bansal T, Kiran S, Kamal K, Bangarwa N. Anesthetic management for lobectomy of a 2-month-old infant with bronchogenic cyst: case report along with review of literature. Saudi J Anaesth 2017;11:340-2.
- 7. Singer C, Coşoveanu S, Petrescu I, Spătaru R, Ciobanu O, Dumitra G, et al. Bronchogenic cyst in infants: clinical and histopathological features. Curr Health Sci J 2022;48:135-40.
- 8. Asseri AA, Shati AA, Moshebah AY, Alshahrani OM, Saad RM, Alzuhari AM, et al. Clinical presentation and surgical management of five pediatric cases with bronchogenic cysts: retrospective case series. Children (Basel) 2022;9:1824.
- 9. Balta C, Gunay S. A rarely seen symptomatic intrapulmonary bronchogenic cyst. Respir Case Rep 2019;8:14-6.
- 10. Ramzisham ARM, Johann KF, Talal AR, Joanna OS, Zamrin DM. Infected intraparenchymal bronchogenic cyst mimicking recurrent lung abscess in a young adult. Med J Malaysia 2007;62:416-7.
- 11. Almatrafi S. Intramural bronchogenic cysts in the pediatric population. Cureus 2020;12:e7111.
- 12. Yoon YC, Lee KS, Kim TS, Kim J, Shim YM, Han J. Intrapulmonary bronchogenic cyst: CT and pathologic findings in five adult patients. AJR Am J Roentgenol 2002;179:167-70.
- 13. Jung HS, Kim DK, Lee GD, Sim HJ, Choi SH, Kim HR, et al. Video-assisted thoracic surgery for bronchogenic cysts: is this the surgical approach of choice? Interact Cardiovasc Thorac Surg 2014;19:824-9.
- 14. Xu S, Liu B, Wang X, Meng H, Wang T, Wang S. Robotic thoracic surgery of the anterior superior mediastinal bronchogenic cyst. Ann Transl Med 2015;3:57.
- 15. Mestan H, Ceylan KC, Kaya ŞÖ. Surgery outcomes of bronchogenic cysts. Eur Respir J 2019;54:PA1094.
- 16. Fievet L, Gossot D, de Lesquen H, Calabre C, Merrot T, Thomas P, et al. Resection of bronchogenic cysts in symptomatic versus asymptomatic patients: an outcome analysis. Ann Thorac Surg 2021;112:1553-8.
- 17. Hynes CF, Marshall MB. Video-assisted thoracoscopic resection of recurrent intrapulmonary bronchogenic cyst after thoracotomy. Innovations Phila Pa 2014;9:142-4.
- 18. Whooley J, White A, Soo A. Bronchogenic cyst: a rare case of malignant transformation. BMJ Case Rep 2022;15:e248916.
- 19. Bouassida I, Hadj Dahmane M, Zribi H, Bessrour H, Hachicha S, Marghli A. A poor prognosis of a mediastinal bronchogenic cyst with malignant transformation: a case report. Int J Surg Case Rep 2023;106:108246.