The introduction of Malone antegrade continence enema) in the management of children with fecal incontinence has brought remarkable improvement in patient care, Malone originally described appendix as a conduit and it has become widely accepted. However, surgeons are faced with situations where appendix is not available, the selection and creation of other conduit is always a challenge. We present our technique and experience with the use of alternative catheterizable conduits for antegrade continence enema (ACE).
Retrospective review of children who underwent ACE procedure in our institution from March 2009 to January 2014. The details retrieved: indication, reason for non availability of appendix, type of conduit, complications and patient's satisfaction.
Five children were identified in whom the appendix was not available or suitable. In four children cecal/colon-based flap was used and in one child, ileal (Monti) segment was used to create a conduit. The mean follow-up was 3.2 years. All patients were satisfied with the procedure and no stenosis or loss of conduit was noted in the follow-up.
Continent catheterizable conduit for ACE can be accomplished with transverse tubularized intestinal segments and cecal/colonic flaps, with excellent outcome, irrespective of tissue used. Surgeon's preference and the patient's peculiar anatomy should determine the surgical technique to be used.
Anorectal duplications account for only 5% of gastrointestinal duplications, and cases with involvement of the anal canal are much rarer. Nearly all anorectal duplications are posterior to the rectum; duplications located anterior to the normal rectum are highly unusual, and only a few cases have been reported. We report the case of an anterior anorectocolonic duplication presenting as a rectovaginal fistula in a 2-month-old infant. After diagnosis, the duplication was excised completely without further intestinal complications.
Colonic atresia (CA) is the rare cause of intestinal obstruction, and diagnosis of CA is difficult. But only few research has been performed, so little information has been available. The purposes of this study was to analyze the clinical findings of CA so that help physicians make decision properly. Children with CA who were treated at the division of pediatric surgery at Asan Medical Center in the period from January 1989 to December 2011 were evaluated retrospectively. A total of 6 children were treated with CA. These accounted for 2.7% of all gastrointestinal atresias managed in Asan Medical Center. Only one child was premature and low birth weight, the others were fullterm neonates and showed normal birth weight. Vomiting and abdominal distension were common symptoms and simple X-ray and barium study were used for diagnose of CA. But only 66.7% of the babies were diagnosed as CA pre-operatively. And 2 children out of 6 underwent re-operation due to missed CA at the time of the first operation. In aspect of types of atresia, the type IIIa were two, type IV were two, type I was one case, and one child showed rectal stenosis due to rectal web. Various operations were done according to individual findings and associated diseases. The 50% (n=3) of children underwent the primary anastomosis and the others (n=3) underwent colostomy first and staged operation later for missed CA or associated disease. All of them were recovered any significant complications. Therefore, the prognosis of CA is satisfactory if diagnosis and surgical management could be made properly. But because of the low incidence of CA, delay of diagnosis and treatment may occur. To prevent delay of diagnosis, we suggest prompt evaluation of doubtful infant and careful inspection of distal patency of bowel including whole colon and rectum when operating patients with intestinal atresia at any level.
Visceral lipoma originating from the mesentery is very rare in childhood. A 29-month-old male presented with painless abdominal distension. Abdominal ultrasonography and CT revealed a huge multilobulated hypodense mass in the peritoneal cavity. Exploratory laparotomy showed a 26 × 25 × 5 cm sized encapsulated, lobulated, homogenous mass, which originated from the transverse mesocolon. Histologic examination revealed a lipoma. The postoperative course was uneventful.
Diffuse cavernous hemangioma of the rectosigmoid is a rare lesion usually presented in children and young adult, often with life threatening hemorrhage. The clinical diagnosis is difficult and often delayed because of lack of awareness of the clinical features. We report a case of diffuse cavernous hemangioma of the rectosigmoid in a 12-year-old boy who had undergone suture ligation under the impression of hemorrhoid at his age 3. Sphincter-saving coloanal pull through procedure were applied as the surgical treatment. Sclerotherapy was needed with recurrent rectal bleeding 6 months after the pull through operation. The patient is well at 12 months follow-up.
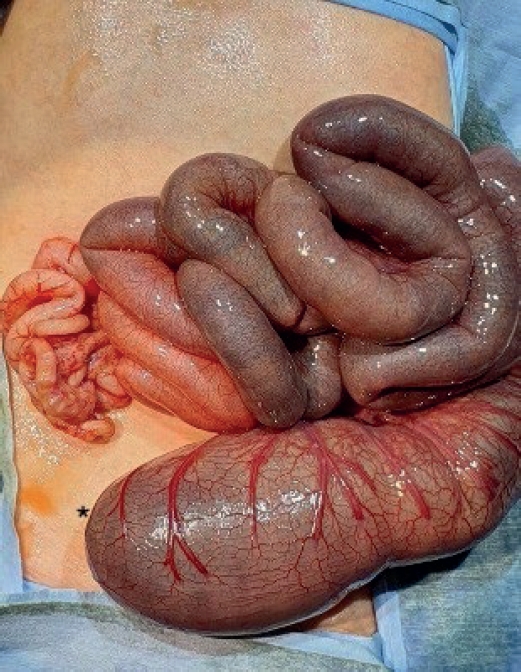
We present a case of a colonic involvement associated with necrotizing pancreatitis, with a review of the literature. A 10 year old boy had an appendectomy at the local clinic ten days ago. On admission, he complained nausea, vomiting and severe constipation. His abdomen was distended and he had tenderness on the left abdomen. Laboratory and radiologic studies revealed findings consistent with acute pancreatitis with colonic complication. He was treated conservatively for 30 days but did not improve. On hospital 30th day, abdominal pain developed and his vital sign changed. Abdominal CT suggested ischemic change of the transverse colon. At laparotomy, the left colon showed stenosis. The greatly distended transverse colon was resected and a transverse end colostomy was done. He was discharged at postoperative 45th day with improvement and colostomy closure was performed 8 months later.
The etiology of several motility disorders, including persistent megacolon after definitive surgery for Hirschsprung's disease, meconium ileus which is not associated with cystic fibrosis and idiopathic megacolon, is still unclear. Interstitial cells of Cajal (ICC) are thought to modulate gut motility as gastrointestinal pace maker cells. The aim of this study was to evaluate the role of ICC in the bowel walls of the patients (n=15) who had variable motility disorders. The ICC were identified by immunohistochemical staining using an anti-C-Kit antibody and the results were compared with control specimens (n=2). The control group (G1) showed evenly distributed ICC in their bowel walls. The second group (G2, n=5) who had normal bowel movements after Duhamel procedures and the third group (G3, n=4) who had persistent megacolon after Duhamel procedures showed absent or scarcely distributed ICC in their aganglionic bowels. The ICC were identified by immunohistochemical staining using an anti-C-Kit antibody and the results were compared with control specimens (n=2). The control group (G1) showed evenly distributed ICC in their bowel walls. The second group (G2, n=5) who had normal bowel movements after Duhamel procedures and the third group (G3, n=4) who had persistent megacolon after Duhamel procedures showed absent or scarcely distributed ICC in their aganglionic bowels. Whereas ICC were evenly distributed in the ganglionic bowels of G2, they were not seen or scarecely distributed in the ganglionic bowels of G3. Two patients (G4) who suffered from idiopathic megacolon showed absence or decrease of ICC in spite of presence of ganglion cells in their colons. Four neonates (G5) who underwent ileostomy because of meconium obstruction showed absent or markedly decreased ICC in the colon at the time of ileostomy and the distribution of ICC was changed to a normal pattern at the time of ileostomy closure between 39-104 days of age and their bowelmotility were restored after that. The results suggest that lack of ICC caused reduce motility in the ganglionic colons and it may be responsible for the development of various motility disorders. Delayed maturity of ICC may also play a role in the meconium obstruction of neinates.
Segmental dilatation of small intestine is a rare form of the congenital intestinal anomaly. Many other congenital anomalies have been reported in these patients, but to our knowledge, the association with colonic duplication has not been reported in literatures. We report a case of segmental dilatation of distal ileum associated with colonic duplication. The main clinical and pathogenic aspects are discussed, and the literatures were reviewed.
The association of congenital colonic atresia with imperforate anus is extremely rare. There are only three cases reported in the English literatures. The authors have recently managed one case in female infant.
We have treated a case of pseudocyst of transverse mesocolon in 3-year-old male child. Operative findings demonstrated that the pseudocyst originated in the transverse mesocolon, and was not connected to the pancreas. A colonic duplication was found incidentally near the pseudocyst. On microscopic examination, ectopic pancreatic tissue was noted in the transverse mesocolon. This pseudocyst was thought to have originated from the ectopic pancreas of the transverse mesocolon. This is the first reported case of pseudocyst originated from ectopic pancreas of the transverse mesocolon, combined with a colonic duplication. The pathogenesis is discussed.
Early recognition and surgical treatment of Hirschsprung's disease prevents serious mortality and morbidity from enterocolitis and obstruction. Usually this disease is characterized by a single aganglionic segment of the colon extending distally to the anal margin. In surgical treatment, the surgeon performs a frozen section biopsy to confirm whether there are ganglion cells. If there are intervening ganglionic sites in aganglionic bowel, there may be confusion in diagnosis and treatment. The authors experienced one case of total colonic aganglionosis with skip area. A transverse loop colostomy was performed on a 7 day-old male baby with colon perforation due to Hirschsprung's disease. But intestinal obstruction persisted and required two more operations to find the true nature of the disease. There were aganglionic segments from the anal margin to the terminal ileum 3.7cm proximal to the ileocecal valve. The entire transverse colon and appendix were normally ganglionated.
Hyperimmunoglobulin E syndrome is a relatively rare primary immunodeficiency syndrome characterized by recurrent infection, abscess formation and marked elevation of serum IgE level. The common infectious organism is Staphylococcus aureus and recurrent infection indicates some defects in the immunologic system. Although the infection can affect various organs, gastrointestinal tract involvement is rare and only one case of colon perforation has been previously reported. Herein we report another one case of colon perforation which ocurred in an 8-year-old girl with hyperimmunoglobulin E syndrome. The patient was admitted to the hospital due to an abscess on right neck. The diagnosis of hyperimmunoglobulin E syndrome was made because she had eczematoid dermatitis on the face, pneumatocele on left upper lung field and markedly elevated serum Ig E level(> 15,000 IV/ml) with a past histories of frequent scalp abscesses and otitis media. Abdominal pain developed on the 13th day of admission and abdominal plain X-ray revealed free air. An exploratory laparatomy was performed and two free perforations of the transverse colon were noted. Segmental resection and double barrel colostomy were performed. Colostomy closure was done 4 month later and she had no gastrointestinal problem during a follow up period of 15 months.
Colonic atresia is the least common form of intestinal atresia. Colonic atresia, like jejunoileal atresia, mostly occurs as a result of an intrauterine vascular accident. According to Sutton's classification, type 1 colonic atresia exibits external continuity with an intraluminal diaphragm(colonic web) which may be imperforate or perforate. Authors experienced a case of colonic web associated with imperforate anus. The patient was treated under the impression of the high type imperforate anus. Posterior sagittal anorectoplasty at the age of 9 months revealed normal anorectal canal. At the age of 12 months, colostomy was repaired. Thereafter abdominal distension was developed. Barium enema noted a membranous obstruction of the colon on the level of the rectosigmoid junction. After exicision of the colonic web, the patient was discharged with no problem.
Segmental dilatation of the colon is a very rare disease entity of unknown etiology and may mimic Hirschsprung's disease. It is characterized by dilatation of a segment of the colon of variable length with obstruction due to lack of peristalsis in a normally innervated intestine. Recently authors experienced a case of segmental dilatation of the sigmoid colon in a 6 month-old male, who presented with severe constipation, abdominal distention, and abdominal mass since 2 months of age. Down's syndrome and congenital nystagmus were associated. Barium enema demonstrated focal dilatation of the sigmoid colon, but the rectum and descending colon proximal to the affected colon were of normal caliber. Rectal suction biopsy with acetylcholinesterase staining was normal and anorectal manometry showed normal rectosphincteric reflex. At operation, there was a massively dilated and hypertrophied sigmoid colon with increased tortuous serosal vessels, measuring 15 cm in length and 10 cm in width. Teniae coli were identifiable in the affected segment. Frozen section biopsies at the proximal, affected, and distal colon showed ganglion cells. Descending loop colostomy was constructed initially and segmental resection and end to end colocolostomy were carried out 3 months later. Final histologic examination showed 1) normal colonic mucosa with ganglion cells, 2) prominent submucosal fibrosis and marked muscular hypertrophy, 3) unremarkable acetylcholinesterase activity and immunohistochemical findings against S-100 protein. On 8 months follow-up, he has been doing well and moves bowels 1-2 times daily.

