We evaluated perioperative and long-term outcomes of minimally invasive surgery (MIS) and established indications of MIS in solid pseudopapillary tumor (SPT) in pediatric patients.
From October 1992 to April 2018, 66 patients (age, <18 years) diagnosed with SPT underwent either open pancreatectomy (OP) or MIS. Variables including postoperative complications and recurrence rates were retrospectively analyzed.
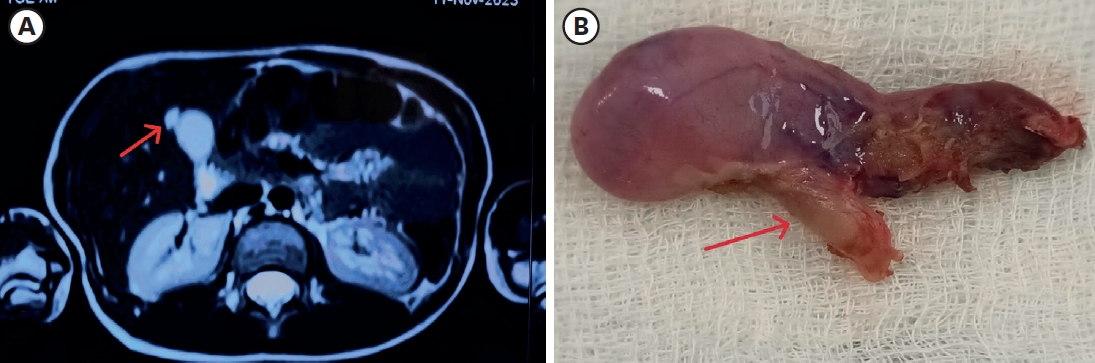
Thirty-five patients underwent open surgery and 31 underwent laparoscopic/robotic surgery. Mean tumor size in MIS was significantly smaller than that in OP (4.3±1.8 cm vs. 7.6±3.5 cm, p=0.005). There were 4 cases of open conversion from laparoscopic surgery because of vessel encasements (n=2), bleeding (n=1), and pancreatic ductal injury (n=1). Solitary pseudopapillary carcinoma was diagnosed in 6 patients. Recurrence was observed in 3 and 1 patients who underwent OP and MIS, respectively (p=0.634). Tumor size, mass size/abdominal diameter (MS/AD) ratio, and degree of the portal or superior mesenteric vein involvement were the most important indications for MIS.
MIS is being widely used in pediatric surgeries with increased expertise and safety, especially in pancreatic diseases. Careful patient selection for MIS in regards with parameters such as MS/AD ratio and vessel abutment might be a feasible choice.
Currently the substantial clinical benefits of single-port laparoscopic appendectomy (SLA) over conventional three-port laparoscopic appendectomy (CLA) are equivocal. The aim of this study was to compare surgical outcomes between SLA and CLA in children with acute appendicitis.
A single blind prospective randomized single center study was performed to compare the surgical outcomes of SLA and CLA. A total of 105 patients were randomized and various parameters were analyzed, 52 patients with SLA and 53 patients with CLA between July 2013 and March 2014. Patients with sonographically confirmed acute appendicitis were randomly assigned to receive either SLA or CLA. The outcome measurements were operating time, wound complication, and intraperitoneal morbidities, postoperative pain score and cosmetic result score.
Operating time is significantly longer in SLA (70.4±26.7 minutes vs. 58.0±23.4 minutes; p=0.016). There were no significant differences in the postoperative wound complication rate and intraperitoneal morbidities between two groups. There were no significant differences in postoperative resting pain score (6.6±2.5 vs. 6.3±2.5; p=0.317) and activity pain score (6.9±2.4 vs. 6.3±2.5; p=0.189), and the cosmetic result score (9.2±1.1 vs. 9.1±1.4; p=0.853).
Although SLA would be a safe and feasible procedure in children, SLA could not demonstrate the clear benefit over CLA.
The application of laparoscopic techniques for the surgical management of Hirschsprung's disease is the recent trend. We described the surgical technique and postoperative long-term outcomes of the one-stage, laparoscopic-assiseted endorectal pull-through operation for Hirschsprung's disease. The technique uses three to four small abdominal ports. Laparoscopic mobilization of the sigmoid colon and rectum is performed and marginal artery-preserving colon pedicle is prepared. The rectal mobilization is performed using a transanal endorectal sleeve technique. The anastomosis is performed 0.5~1 cm above the dentate line. The age at surgery ranged from 6 days to 4 years. The average operative time was 144 minutes. Almost all of the patients passed stool and flatus within 36 hours of surgery. The average hospital stay after surgery was 6.5 days. Among 42 patients, 32 patients older than 3 years old were evaluated for function on defecation. All 32 patients have been continent, of those who needed laxatives were 11 (34.3%) due to constipation and overflow incontinence. Four children (12.5%) have remained dependent on laxatives. Laparoscopic-assisted endorectal pull-through operation for Hirschsprung's disease appears to be safe, provides the less pain, shorter time to full feeding, shorter hospital stay, and excellent cosmetic outcomes. Helping patients and parents ensure the quality of life, they should be provided with counseling, education, and longer-term follow-up care.
Fundoplication is a common surgical procedure for gastroesophageal reflux Disease (GERD). Recently the procedure has been performed with increased frequency laparoscopically. The aim of this study is to compare laparoscopic Nissen fundoplication (LNF) and open Nissen fundoplication (ONF) for GERD in children. We studied retrospectively the 88 pediatric patients who underwent the Nissen fundoplication for GERD as primary antireflux surgery from 1994 and 2009. ONF was performed in 34 cases and LNF was in 54 cases. 58 patients have neurologic impairment. Time to initial food intake after the surgery were reduced in the LNF group (
Use of laparoscopic appendectomy (LA) for perforated appendicitis (PA) in children remains controversial because of the development of postoperative intra-abdominal abscess formation. We developed the irrigation method for the prevention of abscess formation after LA performed for PA in children with severe panperitonitis. We called it ‘the shaking irrigation’. The object of this study was to analyze the efficacy of this irrigation method. All cases of PA with severe panperitonitis in children that underwent LA with massive shaking irrigation and drainage between June 2003 and December 2007 were studied retrospectively. We included only PA with panperitonitis and large amounts of purulent ascites throughout the abdomen as well as an inflamed small bowel with ileus. Thirty-four children were involved in this study. The mean patient age was eight years. The mean amount of irrigation fluid was 8.2L (range: 4-15L). The mean operative time was 89.5 min. The mean length of the hospital stay was 5.1 days. There were no postoperative intra-abdominal abscesses. There was no conversion to open surgery. In conclusion, Use of LA in PA with severe panperitonitis in children is safe and effective. Massive shaking irrigation and abdominal drainage appears to prevent intra-abdominal abscesses after LA for PA with panperitonitis.
Meckel's diverticulum (MD) has various clinical presentations and due to the limitation of imaging studies, pre-operative diagnosis is a challenge in pediatric patients. Recently, laparoscopic exploration has been suggested as a favorable method for the diagnosis and treatment of complicated MD. We investigated the results of laparoscopic-assisted surgery compared with open technique. We retrospectively studied patients who underwent resection of complicated MD at our institute from 1997 to 2010 and compared 11 treated by laparoscopic-assisted diverticulectomy (LD) with 11 treated by open diverticulectomy (OD) for complicated MD. Operation time was not significantly different in the two groups. Hospital stay and time to diet were not significantly different. Two patients were re-admitted due to mechanical ileus in the LD group. None of patients in either group needed re-operation. Considering the possibility of false-positive results with imaging studies and the cosmetic benefit, laparoscopic-assisted surgery is a safe and effective treatment modality to diagnose and treat complicated Meckel's diverticulum.
Gastric trichobezoars are commonly observed in young women with trichotillomania and trichophagia. We encountered an 8-year-old girl who had trichotillomania and trichophagia with abdominal pain and a mass, which was diagnosed as a large gastric trichobezoar. On physical examination, a huge, firm nontender mobile mass was palpated in her epigastrium. An upper gastrointestinal series and abdominal computed tomography (CT) scan showed a large mass in the stomach. Endoscopic removal was tried but failed. Laparoscopic removal was therefore performed. The trichobezoar was successfully retrieved through a gastrotomy and removed through an extended umbilical trocar incision. This case demonstrates that laparoscopic removal of large gastric trichobezoars is feasible and safe without a large abdominal incision.
Intraabdominal cystic lymphangioma is an uncommon lesion. It is usually found incidentally in patients presenting with an acute abdomen. Laparoscopic excision of intraabdominal cystic lymphangioma is an easy and safe procedure in children. We report one case of cystic lymphangioma in a 6-year-old female. The lesion was located on the left side of the transverse mesocolon. Laparocopic excision of the cyst was performed without complications.
Fundoplication is a common surgical procedure for gastroesophageal reflux disease (GERD). Recently the procedure has been performed with increased frequency laparoscopically. The aim of this study is to review our 11 years experience with fundoplication in infants and children. From October 1994 to December 2005, 59 fundoplications in 55 patients were performed at Sungkyunkwan University Samsung Medical Center. Medical records and laboratory results of these children were retrospectively reviewed for sex, age, symptoms and signs, coexisting disease, diagnostic methods, treatment modalities and length of operative time. Open fundoplication was performed in 41 cases and laparoscopic fundoplication in 18 cases. Simultaneous gastrostomy was done in 27 cases. Recurrent GERD symptom occurred in four patients (7.2 %) within 2 years after first fundoplication and all 4 patients had re-do fundoplication. There were no intra- and immediate post-operative complications. Gastrointesitnal symptoms were the most common indication for fundoplication in neurologically normal patients. The most frequent diagnostic studies were upper gastrointestinal series (76.3 %) and 24 hour esophageal pH monitoring (78.2 %). Fundoplication had been increased since 2004 and mostly done laparoscopically. In conclusion, our 11 years' practice of open and laparoscopic fundoplication indicates that both approaches are safe and effective in the treatment of GERD for infants and children.
A nationwide survey on acute appendicitis (AAP) was undertaken among members of the Korean Association of Pediatric Surgeons. The members were required to complete a questionnaire and the case registration form for each patient during the 6 months period from the 1st October, 2005 to 31st March, 2006. Questionnaires were collected from 23 members. Four hundred seventy six patients were registered from 21 hospitals where the members were working. The male to female ratio was 1.67:1. Average age was 9 years and 5 months (range 21 months-20 years). Operations were performed on average 10.4 hours (range 1-230 hours) from arrival at hospital. The average operation time was 59.1 minutes. The average admission days were 5.8 days (range 2-45 days). The most frequent symptoms were abdominal pain (95.1%), vomiting (50.6%) and fever (43.7%). The average duration of symptoms was 42.2 hours (range 1 hour-22 days). Leukocytosis (WBC count>10,000) was found in 85.9%. The most popular diagnostic tools were ultrasonography and CT. Open surgery was performed in 72.1% and laparoscopic surgery in 27.5%. Two laparoscopic surgeries were converted to open surgery (0.4%). Simple appendicitis was found in 54.5% and complicated appendicitis such as abscess, gangrenous change and perforation in 45.5%. According to the questionnaires 12 hospitals were performing open surgery only in all patients. Four hospitals were performing laparoscopic surgery in all patients. Seven hospitals are performing both surgical methods according to surgeon or occasion. Regarding the use of antibiotics in acute appendicitis, three kinds of antibiotics were used in 40% of total simple appendicitis patients. The results showed the trend of management in acute appendicitis in Korea. Especially it is necessary for the members to discuss the use of antibiotics for prophylaxis in the simple appendicitis
It is known that pediatric inguinal hernia is caused by the incomplete closure of processus vaginalis (PV). In the case of unilateral hernia, possibile contralateral patent PV should be considered because of its delayed appearance as well as its risk of incarceration. Direct visualization of patent PV could be done by contralateral exploration or by indirect exploration through the ipsilateral opening site of the affected hernia assisted with laparoscope. A patient group (321 persons) to whom laparoscopy was not performed from March 2000 to March 2003 was analyzed and compared with a patient group (280 persons) to whom laparoscopy was performed from April 2003 to September 2005. With all 601 patients, the sex ratio (male/female) of patients was 3.8:1. The side distribution was 57.7% in the right, 32.1% in the left and 10.1% in bilateral. There was no difference of sex and side distribution between before and after laparosopy adoption. We did not find an age correlation in natural closure of the residual PV of the peritoneum. Contralateral hernia developed in 14 persons (2.5%) after the operation of unilateral inguinal hernia before laparoscope adoption. But no contralateral hernia developed after April 2003 with laparoscopy. We think that if we use laparoscopy, being a safe and accurate method, to check whether the contralateral residual PV is opened or closed, possible future contralateral operation can be avoided.
Laparoscopic cholecystectomy has been increasingly used because of several advantages, less pain, better expectation for cosmesis (requires small incisions), and more rapid recovery compared with open cholecystectomy. Oral intake is tolerated on the day of operation or on the next. In this study, we evaluated the effectiveness and safety of laparoscopic cholecystectomy in children. Nine cases of laparoscopic cholecystectomy for acute and chronic cholecystitis in children were performed at Asan Medical Center between April 2002 and April 2004. Laparoscopic cholecystectomy was performed on a total of 10 patients, but one of them was excluded because of the simultaneous splenectomy for sickle cell anemia. Clinical presentation, operative findings, operation time, length of hospital stay, and postoperative complications were analyzed. Mean age was 10.4 (4–15) years, and only 3 of patients were less than 10 years. One patient was female. In 8 the diagnosis was calculous cholecystitis. Mild adhesions were found in 3 cases and intraoperative bile leakage in 2. There was no conversion to open surgery and there were no vascular, bowel, or bile duct injuries. Mean operation time was 82.2 (20–160) minutes ; mean length of hospital stay was 2.1 (1–3) day. There was no postoperative complication. Laparoscopic cholecystectomy in children was remarkably free of side effects and complications and had a short recovery time. Laparoscopic cholecystectomy for cholecystitis is considered to be a standard procedure in children.
Mature cystic teratoma, commonly called dermoid cyst, is the most common benign germ cell tumor of the ovary in children. Malignant transformation is rare, approximately 2%. As laparoscopic procedures are applied widely in pediatric surgery, a female chlid with a mature cystic teratoma may be an ideal candidate for laparoscopic surgery. Two children received laparoscopic operations successfuly for lower abdominal crises, twisted adnexa. There was no operative complication. Laparoscopic approach for ovarian lesions in infancy and childhood appears to be an effective and safe method for diagnosis as well as definitive therapy.
Superior mesenteric artery (SMA) syndrome is a rare disorder caused by extrinsic compression of the third portion of the duodenum by the SMA. The operative treatment of choice is bypassing the obstructed duodenal segment by duodenojejunostomy. We report one case of SMA syndrome treated by laparoscopic duodenojejunostomy and followed up by 3D-reconstructive CT scan. A fifteen-year-old boy with intermittent vomiting and weight loss was admitted. Ultrasonography showed narrowing of the distance between the SMA and aorta. Hypotonic duodenography showed dilatation of duodenal third portion and barium stasis. On 3D-reconstructive CT scan, the angle between SMA and aorta was 37 °. The postoperative course was uneventful. Three months later, he had gained 3 kg of weight and the angle between SMA and aorta increased to 38-39 ° on 3D reconstructive CT scan. Laparoscopic duodenojejunostomy for bypassing the obstructive duodenum in SMA syndrome is a feasible and safe method.
Appendectomy is the most common emergency surgical operation in children. The laparoscopic treatment of pediatric appendicitis is controversial, particularly in complicated cases. The purpose of this study is to evaluate laparoscopic appendectomy (LA) and open appendectomy (OA) for simple and perforated appendicitis (SA, PA) in children. A total of 188 patients, operated from January 1992 to September 2003, were reviewed. Ninety-one patients underwent OA (65 SA and 26 PA) and 97 had LA ( 67 SA, 30 PA). There was one conversion of LA to OA in PA. Operative time for LA was longer for OA in PA (55.8 vs. 45.7 min; p=0.0467). Recovery of bowel movement, diet starting time, length of hospital stay for LA were significantly shorter than those for OA. Postoperative complication rate was not different between LA and OA in each group. Laparoscopic appendectomy is a safe and effective method for both simple and perforated appendicitis.
Pediatric laparoscopic splenectomy has gained increasing acceptance in the surgical management of a variety of splenic disorders, in particular hematologic diseases. We report our experience with 16 patients who underwent this procedure because of hematologic disorders during the past 3 and a half years at the Department of Surgery, St. Mary's Hospital, Catholic University Medical College. The mean age was 10 years (Range 6-16 years) and the mean spleen weight was 210 gm (Range 85-500 gm). The indications for splenectomy were hereditary spherocytosis (6 cases), idiopatic thrombocytopenic purpura (8 cases), autoimmune hemolytic anemia (1 case), and idiopatic splenomegaly (1 case). All splenectomies were performed safely with mean estimate blood loss of 233 ml. Mean operative time and mean postoperative hospital stay was 157 min and 4.5 days. Respectively postoperative pain medication was needed in 3 case, just one injection in immediate postoperative period. Diet was started on posterative second day or third day. In conclusions, Laparoscopic splenectomy in pediatric patients surely is a safe procedure, offering better cosmesis, much less pain, and shorter hospital stay with lower post operative mobidity.
Advances in instrumentation and technique now make laparoscopic correction of some congenital anomalies possible. Author reports a 6-day-old boy with Hirschsprung's disease successfully treated by a laparoscopic endorectal pull-through procedure. The technique and its potential role in the treatment of Hirschsprung's disease are described. One camera port and three working ports were used for access to the peritoneal cavity. The descending and sigmoid colons were mobilized laparoscopically. A submucosal sleeve was developed transanally to meet the dissection from above. The colon was then pulled down in continuity, divided above the transition zone, and secured to the anal mucosa about 10 mm above the pectinate line. Author concludes that the laparoscopic endorectal pull-through procedure could be performed in safe.
Three cases of laparoscopic splenectomy for hereditary spherocytosis are reported. The average operation time was 100 minutes. This was longer than traditional open splenectomy for the same entity( 63 minutes). Average hospitalization period was 3 days. This was shorter than the hospitalization period for the traditional group(6.2 days).
Laparoscopic appendectomy is relatively well-established as an alternative to conventional open appendectomy by many laparoscopic surgeons. However, experience in the pediatric population remains limited. Over a period of 2 years, a total of 155 pediatric patients with acute appendicitis or complicated appendicitis were studied to compare laparoscopic and open appendectomies in childhood. Laparoscopic appendectomy was attempted in 49 patients and completed in 48 patients(98.0%). Open appendectomy was performed in 107 patients. The severity of disease, age, and male to female ratio were similar in both groups. The operation time was shorter in the laparoscopic group than open group but the difference was not significant statistically(43.7±11.3 minutes versus 49.0±21.4 minutes, p=0.066). In the laparoscopic group, the mean duration of surgery for the former half patients was significantly longer than for the latter half(49.6±9.2 minutes versus 38.1±10.3 minutes, p=O.OOl). The mean number of doses of analgesia required postoperatively was significantly less in patients undergoing laparoscopic appendectomy(2.4±1.8 versus 3.3±2.5, p=0.021). There were only 2 (4.2%) wound infections after laparoscopic appendectomy compared with 10(9.3 %) complications including 7 wound infections, 1 intestinal obstruction, and 2 pulmonary complications after open appendectomy, but the difference was not significant( p=0.614). Patients undergoing laparoscopic appendectomy had a shorter period of hospitalization(3.2±2.2 days versus 6.4±1.6 days, p=O.OOl). The present study suggests that laparoscopic appendectomy shortens operating time and hospital stay with diminished postoperative pain. Laparoscopic appendectomy in children offers advantages over open appendectomy as noted in adults. The authors consider laparoscopic appendectomy to be the reasonable alternative to open appendectomy in children.

