An 18-year-old male patient with cerebral palsy and scoliokyphosis came to the emergency department with abdominal distension and vomiting. He was a situs inversus patient with a feeding gastrostomy tube. Sigmoid volvulus was initially suspected, so rectal tube insertion and endoscopic decompression were attempted, but failed. So he went through explorative laparotomy, and transverse colonic adhesion and twisting around the gastrostomy tube and gastric wall was identified. Adhesiolysis and resection with redundant transverse colon and end-to-end colocolic anastomosis was performed. He discharged with symptom free. Suspecting transverse colonic volvulus is important when the patient has anatomical anomalies and feeding gastrostomy tube. Timely diagnosis with proper radiologic imaging should be made. Surgical resection of the redundant colon is needed for successful management of transverse colonic volvulus.
Citations

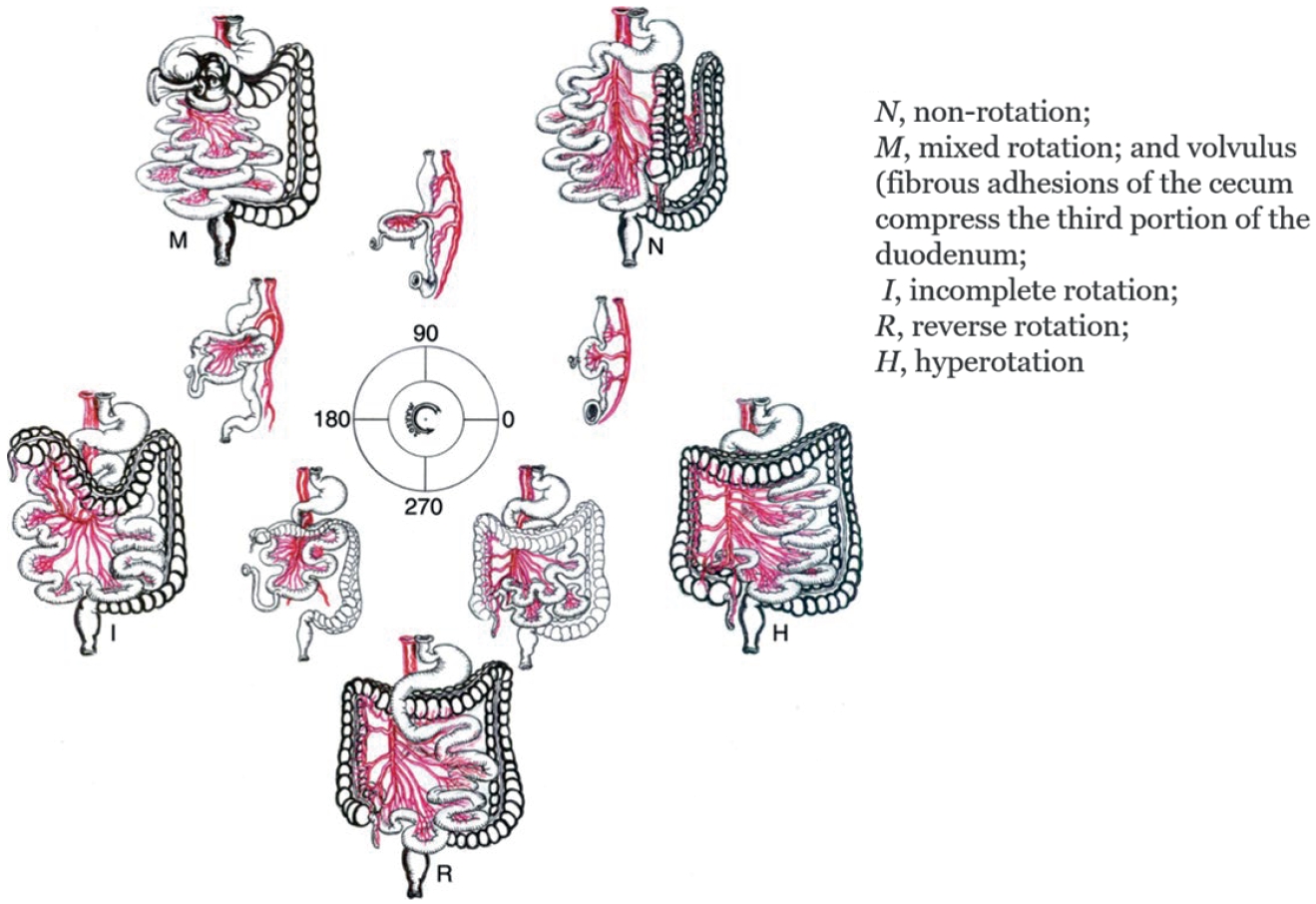
Malrotation is a congenital anomaly that becomes symptomatic more frequently during infancy. The indication for surgical treatment at that age is straightforward. In older children, the diagnosis may be more difficult because of chronic and vague complaint. The aim of this study is to compare the symptoms, rate of volvulus and surgical findings in children younger and older than one year. A retrospective study of 40 patients in a a single medical center diagnosed with malrotation from April 1996 to May 2010 was performed. There were 20 (50%) boys and 20 (50%) girls. At the time of operation, 27 (67.5%) patients were younger and 13 (32.5%) were older than 1 year. Vomiting was seen in 20 cases (74.1%) of the younger group compared to 2 cases (15.4%) of the older group. Abdominal sonography and upper gastrointestinal series showed a sensitivity of 100%. Operative findings: 12 (44.4%) of the younger group presented with volvulus compared to none of the older group. The Ladd's procedure was routinely performed with appendectomy in all cases and bowel resection was requires when volvulus included bowel necrosis or other anomalies were found. After definite procedures, surgical correction for adhesive obstruction was necessary in 5 menbers (18.5%) of the younger group and 1 patient (7.7%) in the older group. There was 1 death due to respiratory failure and pneumonia. Abdominal pain was more frequent symptom and bilious vomiting was less frequent. Volvulus did not occur in the older group. Malrotation should be diagnosed promptly in children over 1 year of age by upper gastrointestinal series and abdominal ultrasonography even though symptoms are not as clear cut as in infants.
Citations

Intestinal malrotation presents with different clinical characteristics, depending upon the age of the patient. The medical records of 44 patients treated for intestinal malrotation with/without midgut volvuls between January 2002 and August 2009 at Seoul National University Children's Hospital were reviewed retrospectively. Patients were grouped by the age criteria of 1 and 12 months. Fourteen patients were under 1 month of age (31.8%), 9 patients between 1 month and 12 months (20.5%) and 21 patients over 12 months (47.7%). Twenty patients (45.5%) presented with volvulus. Vomiting (66%) and abdominal pain (20%) were the most common symptoms. UGIS (68.2%) was the most frequent diagnostic tool. Mean postoperative hospital stay was 13.7 days. There were 7 mild postoperative complications. Volvulus was more frequent in patients under 1 month (p=0.025) than over 1 month. The interval between diagnosis and operation was shorter in patients under 1 month (p=0.003) than in patients over one month of age. In the age between under and over 12 months, volvulus was more common in those under 12 months of age, but the difference was not significant. The interval from diagnosis to operation was shorter in patients under 12 months than over 12 months of age (p=0.001). Vomiting was the most frequent symptom in patients under 12 months. On the other hand, abdominal pain was the most frequent symptom in patients over 12 months.
In conclusion, patients with intestinal malrotation had age-related differences in the presence of midgut volvulus, the interval between diagnosis and operation, and clinical symptoms. The age of the patient should be considered in order to determine adequate treatment of malrotation.
Intestinal malrotation is usually asymptomatic and most often is found during abdominal exploration for other surgical diseases. However, a serious complication of intestinal malrotation, midgut volvulus is a true surgical emergency of childhood. The clinical findings, diagnostic procedures, treatment, and prognosis of midgut volvulus were reviewed by a retrospective study. Between 1980 and 2005, 29 patients with midgut volvulus ranging in age from 1 day and 15 years were treated at HanYang University Hospital. Seventy-nine percent of the patients presented before 1 month of age. Midgut volvulus occurred 2 times more frequently in male. The clinical findings were bilious vomiting (96.6 %), irritability (34.5 %), abdominal distention (13.8 %), abdominal pain (10.3 %), and palpable abdominal mass (6.9 %). The diagnosis was made by abdominal simple x-ray (17.2 %), upper gastro-intestinal contrast study (37.9 %), abdominal sonogram (20.7 %), abdominal CT (3.4 %), and abdominal exploration (20.7 %). Among the 29 patients, 5 patients developed gangrene of small intestine due to strangulation and underwent resection of bowel. Two patients died due to sepsis.
Citations

Midgut volvulus secondary to intestinal malrotation usually presents within the first month of life. Diagnostic delay may result in midgut infarction and mortality. In this retrospective study, we review seventeen cases of midgut volvulus to assess the importance of early recognition for midgut volvulus in pediatric patients of any age.. These patients were diagnosed as having a midgut volvulus by operation at Ewha Womans University Hospital. Eleven patients (64.7 %) were less than 1 month of age, and fifteen were boys (88.2 %). The mean gestational age was 38.3 weeks and the birth weight was 3.1 kg. Eight patients (47.1 %) had one or more combined anomalies such as heart malformation, brain ischemia, Down's syndrome or duodenal atresia. Vomiting was the most common symptom. Only thirteen patients underwent preoperative diagnostic procedures; 13 abdominal sonography demonstrated the whirlpool sign in 8 patients, upper gastrointestinal tract roentgenography showed a cork-screw pattern in 7 patients, and barium enema or small bowel series demonstrated positive findings in 7 patients. A Ladd's procedure was was formed on all patients.. There was no mortality or severe morbidity such as short bowel syndrome. Midgut volvulus should be included in the differential diagnosis in any infant or child who presents with the symptoms of acute abdomen, especially with vomiting.
Gastric volvulus is a rare surgical disorder in the pediatric population. We experienced a case of gastric volvulus. A 2-year-old boy was admitted to hospital with abdominal distension. An upper gastrointestinal series showed reversal of the greater and lesser curvatures. Surgical exploration revealed an organoaxial volvulus of the stomach, and anterior gastropexy was performed.
Citations

Primary segmental volvulus of the small intestine is not associated with malrotation, malfixation of the midgut, nor other primary small bowel lesions such as small bowel tumors. This entity is known to be more prevalent in adult and in certain global areas associated with particular diet habits. There have been very few reports in neonates, but not in this country so far. The author reports two cases of primary segmental volvulus. Case 1 was a septic 4-day-old girl with hematochezia due to jejunal volvulus with partial necrosis and panperitonitis. Resection of the segment and Bishop-Koop enterostomy were successful. Case 2 was a 3-day-old boy, who had ileal volvulus with ultra-short length of ileal atresia, probably due to intrauterine segmental volvulus. Limited resection of the atresia and spreading of the mesenteric base were enough to recovery. The rarity of the pathognomonic findings and limitation of the diagnostic workup due to rapid prqgression limit early diagnosis and good survival rate in this particular condition.
A 2-day-old male {Premie, Large for gestational age(LGA), Intrauterine period (IUP) 33 weeks, birth weight 2,955 gram} was transferred with marked abdominal distention, bilious return via the orogastric tube, respiratory difficulty, and generalized edema (hydrops fetalis). He was born by cesarean section to a 36 year-old mother. Antenatal ultrasonogram at IUP 31 weeks demonstrated multiple dilated bowel loops suggestive of intestinal obstruction. There was no family history of cystic fibrosis. Simple abdominal films disclosed diffuse haziness and suspicious fine calcifications in the right lower quadrant. Barium enema demonstrated a microcolon. Sweat chloride test was not available in our institution. At laparotomy, there noted 1) a segmental volvulus of the small bowel with gangrenous change, associated with meconium peritonitis, 2) an atresia of the ileum at the base of the volvulus, and 3) the terminal ileum distal to the volvulus was narrow and impacted with rabbit pellets-like thick meconium. These findings appeared to be very similar to those of a complicated meconium ileus. In . summary, the ileal atresia and meconium peritonitis seemed to be caused by antenatal segmental volvulus of the small intestine in a patient with probable meconeum ileus.
Citations

Citations


