Congenital milia of the nipple are extremely rare, and standard treatment has not yet been established because nipple preserving excision is problematic due to the location. Although most reports show excisional biopsy resulting in good outcomes without recurrence, there is a lack of consensus about treatment modality, with several studies suggesting that incisional evacuation by needle, or a ‘wait and see’ approach represent sufficient treatment. This case report is about a recurrent case after incisional evacuation for congenital milium of the nipple. We recommend nipple preserving excision with exfoliation of the milial capsule as being the most appropriate treatment modality for congenital milium of the nipple.
Early suspicion is essential in diagnosing pyriform sinus cysts. We report two neonatal cases of pyriform sinus cysts presented as neck masses. The first case presented as a right neck mass, which made it more difficult to suspect a pyriform sinus cyst considering the prevalence of left sided cysts. Surgical resection was done in both cases and anatomical investigation suggested both to originate from the fourth branchial pouch. Detection of air bubble containing mass on imaging studies can aid early diagnosis and early use of gastric tube feeding can facilitate treatment by preventing milk contamination which may result in infection of the sinus cyst.
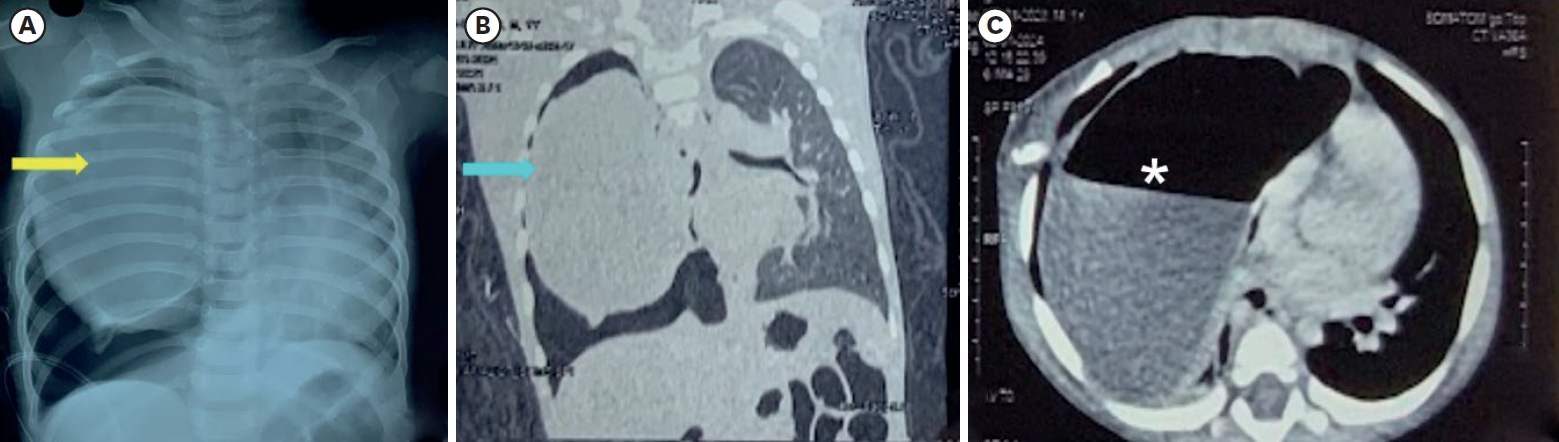
A baby was diagnosed with esophageal atresia (EA) with tracheoesophageal fistula (TEF) on the next day after birth, and end-to-end anastomosis of esophagus with TEF ligation was performed. The distance between proximal and distal esophageal pouch was checked as 3 vertebral body lengths and a 1 cm-sized bronchogenic cyst (BC) was identified near carina on the right side, just below the proximal esophageal pouch. This case report described the baby who have a BC was located between the both esophageal pouch and a longer esophageal gap than usual EA with distal TEF.
We report a neonatal case of “intraluminal” pyloric duplication cyst, causing gastric obstruction after birth. Endoscopy revealed a submucosal cystic lesion approximately 15 mm in size arising from the anterior and inferior surfaces of the pylorus obliterating the pyloric canal. After laparotomy, intraoperative cholangiography was performed, which documented no communication between the cyst and the bilio-pancreatic duct. Gastrotomy was performed transversally over the antrum, and the cyst delivered through the incision. The cyst was incised, the upper part of the cyst wall removed, and a mucosectomy performed on the inner cyst wall of the lower part. The mucosa and muscle of the margin of the cyst were approximated. At follow up of 10 months, the patient is well without any sign of gastric obstruction.
Number of pediatric cholecystectomy has been recently showing a gradually increasing trend. The purpose of this study was to investigate the clinical features of patients who underwent pediatric cholecystectomy, and the latest trend in cholecystectomy.
In the present study, we conducted a retrospective chart review on 47 patients who had undergone cholecystectomy at a single center. The entire patient population was divided into two groups, according to the time of cholecystectomy (early group, January 1999 to December 2006; late group, January 2007 to August 2014).
The comparison between the early and late groups showed that the number of cholecystectomy increased from 13 to 34 cases representing a 2.6-fold increase. The mean patient age also increased from 5.94±4.08 years to 10.51±5.57 years (p=0.01). Meanwhile, laparoscopic surgery also increased from 15.4% to 79.4%, respectively (p<0.001). However, sex, mean body mass index, comorbidities, indications of cholecystectomy, and previous total parenteral nutrition were not statistically significant.
The results of this study showed that pediatric cholecystectomy cases are increasing, particularly in the 10 to 19 years age group and laparoscopic cholecystectomies are also being performed at an increasing rate. When the patients were compared according to the time of cholecystectomy, there were no differences in other risk factors or indications for cholecystectomy.
Median raphe cyst (MRC) of the perineum is rare congenital midline cyst of the male genitalia. MRC is thought to be caused by congenital alterations in the embryologic development of the male genitalia during fetal life. MRC can be found on the midline position between the urethral meatus and the anus. The lesion can be cystic, but sometimes it looks like an elongated configuration called a raphe canal. Diagnosis in childhood is particularly rare because they are usually asymptomatic, but some cases have reportedly been identified after infection. Although conservative treatment can be possible in small asymptomatic lesions, the treatment of choice is simple excision followed by primary closure in symptomatic cases. We describe here the case of 2-year-old boy presented at our institution with a 10-month history of anomaly of the perineal median raphe, which was treated by surgical excision.
The duplication of gastrointestinal tract has been known to be a rare condition and two different forms, cystic and tubular type. This study was conducted to examine its clinical characteristics, especially cystic enteric duplication which was detected antenatally or postnatally.
There were 13 patients, who confirmed as cystic enteric duplication after operation between July 1996 and June 2015. Clinical data, including a gender, age at operation, presenting symptoms, diagnostic modalities, locations of lesion, and results of surgical treatment, were reviewed retrospectively according to cases detected antenatally and postnatally.
Five cases were included in antenatal diagnosis group and 8 cases in postnatal diagnosis group. Both groups show slightly common in female and the lesion most common in ileum. Antenatal diagnosis group shows 2 males and 3 females and the mean age at operation was 12±52 days (range, 5 to 90 days). They received operation regardless of symptom. Postnatal group shows 3 males and 5 females and the mean age at operation was 462.5±777.0 days (range, 4 days to 6 years). Moreover, 6 patients (75.0%) were age before 2 years. They usually presented abdominal pain with vomiting.
Cystic enteric duplication could present symptoms at any time during childhood, mainly before 2 years old, and so a proper management should be considered when suspect it. Although it is uncommon, surgical management including a minimal invasive procedure could be attempted despite the neonatal period.
Branchial cleft anomalies are the second most common head and neck congenital lesions seen in children. Amongst the branchial cleft malformations, second cleft lesions account for 95 % of the branchial anomalies. This article analyzes all the cases of second branchial cleft anomalies operated on at Seoul National University Hospital from September 1995 to February 2011. We analyzed sex, age, symptom and sign, accompanied anomaly, diagnosis, treatment, pathologic report and outcome via retrospective review of medical records. In this series, we had 61 patients (27 female and 34 male). The mean age at the time of operation was 38 months. 31 lesions were on the right, 20 were on the left and 10 were bilateral. The most frequent chief complaints at presentation were non-tender mass and cervical opening without any discharge. According to anatomic type, 29 patients had branchial cleft sinuses, 14 had cysts, 14 had fistulas and 4 had skin tags. Complete excision was attempted if possible and antibiotics challenged when infection was suspected. Complete excision was achieved in 96.7 % of cases. Incision and drainage was done in 2 cases due to severe inflammation, and both recurred. Postoperative complications included wound infection in 2 cases. Microscopic examonation revealed squamous epithelium in 90.2 % and squamous metaplasia in one case in the branchial cleft cyst wall. In summary, second branchial anomaly is found more frequently on right side of neck. Fistulas are diagnosed earlier than cystic forms. Most cases could be diagnosed by physical examination. The definitive treatment is complete excision and sufficient antibiotics coverage for cases with inflammation. After drainage of infected lesions, follow up excision after 1 year might be beneficial for preventing recurrence.
Although laparoscopic surgery for hepatobiliary disease in children is possible, it is technically challenging. In an attempt to overcome these difficulties, the da Vinci Robotic Surgical System(R) was used to facilitate the minimally invasive treatment of choledochal cyst in six children. In early consecutive three cases, we experienced three complications; a case of laparotomy conversion, a case of late stenosis of the hepaticojejunostomy, and a case of leakage from a hepaticojejunostomy. However, in the last three cases the complete resection of the choledochal cyst and Roux-en-Y hepaticojejunostomy were performed using the robotic surgical system without complication.
We think robot-assisted choledochal cyst resection in children appears safe and feasible, and may increase the variety of complex procedures in pediatric surgical fields.
Thyroglossal duct cysts (TGDC) are the most common type of congenital developmental anomaly encountered in the anterior midline of the neck in childhood. The aim of the study was to evaluate the clinical characteristics of TGDC and identify any factors that could be related to recurrence after surgery. This study consisted of a retrospective chart review of 45 patients treated at Kyungpook National University Hospital for TGDC between 1990 and 2008. All records were reviewed for age and sex, length of history, presentation, diagnostic methods, sizes and locations of cyst, surgical management, histopathology of the lesion and recurrences. The statistical analysis of risk factors for recurrence was made using the Fisher's exact test with a significance level of p < 0.05. The male to female ratio was 2.2:1 with a male preponderance. The mean age at operation was 5 years and 2 months (4 months – 17 years). The most common presenting symptom was a nontender cervical mass (78%). Most TGDC were found in the midline position. Twenty four were infrahyoid, 17 were hyoid, and 4 were suprahyoid level. Forty one (91%) patients received the Sistrunk operation, and 4(9%) patients received cyst excision. Postoperative a seroma developed in six patients in the early postoperative days. There were a total of 3(6.6%) recurrences, 2 in patients who had excision only and in one patient who had the Sistrunk operation. Univariate analysis for risk factors with recurrence showed that there was no statistical relationship between the presence of preoperative infection and the development of recurrence. The removal of hyoid bone along with TGDC was a statistically significant risk factor for recurrent disease. This study suggests that the Sistrunk operation is the treatment of choice for TGDC in order to reduce recurrence.
Abdominal cerebrospinal fluid pseudocyst is an uncommon complication of ventriculoperitoneal shunt (VPS) performed for hydrocephalus. The incidence of VPS complications in children is higher than in adults. There are controversies and difficulties in the treatment of the abdominal pseudocyst. We report a case of abdominal pseudocyst complicating VPS in a boy. Partial excision of pseudocyst and replacement of the VP shunt were effective during a followup of 18 months postoperatively with no recurrence.
Splenic cystic lesion is uncommon in children, and cystic lymphangioma of the spleen has not been reported in Korean pediatric patients. Here we report a case of cystic lymphangioma arising from the spleen in a 16 year-old male. The patient presented with left flank pain for 5 days after blunt trauma to the same site. On physical examination, left abdominal tenderness and a palpable spleen were noted. Abdominal ultrasound and MRI revealed multiple septated macro-cystic mass abutting to the spleen medially, suggestive of cystic lymphangioma of the spleen. Laparotomy revealed a 20 cm sized cyst in the spleen, and 2,000mL of dark-brownish fluid was aspirated from the cyst. Splenectomy was performed. Pathological examination revealed the cystic lymphangioma. Post-operative recovery was uneventful, and the patient was discharged at 7 days after surgery.
Choledochal cyst is a congenital dilatation of the bile duct. Intrahepatic bile duct dilatation of type IVa by Todani's classification at the time of diagnosis resolved spontaneously after cyst excision and hepaticojejunostomy in many cases. It should be distinguished from the true cystic dilatation of the intrahepatic ducts, which tends to persist, albeit after some regression. We therefore studied postoperative intrahepatic duct dilatation changes in choledochal cyst. A total of seventy-six choledochal cysts were managed at the Division of Pediatric Surgery, Department of Surgery, Samsung Medical Center from May 1995 to December 2005. The ratio of males to females was 1:2.8. Preoperative radiologic diagnosis by Todani's classification was Type I (n=52, 68.4 %), II (n=1, 1.3 %), IVa (n=23, 30.3 %). Among fifty-five patients with intrahepatic bile duct dilatation we were able to follow up forty-eight by ultrasonography. Twenty-two patients were type IVa, and twenty-six patients were type I and showed intrahepatic duct dilatation. Mean follow-up duration was 35.3 months (9~105 months). Complete regression of dilated intrahepatic duct was observed in fifteen patients of type IVa and twenty-four patients of type I. Incomplete regression of dilated intrahepatic duct was observed in six patients in type IVa and two patients in type I. Only one patient in type IVa showed no change in ductal dilatation during a follow-up period of 15 months. We conclude that true type IVa is much less frequent than what was diagnosed preoperatively by imaging study. Therefore in type IVa patients who are diagnosed preoperatively the decision to perform liver resection should be carefully considered. Postoperative long term follow up of choledochal cyst with intrahepatic bile duct dilation is needed.
Intraabdominal cystic lymphangioma is an uncommon lesion. It is usually found incidentally in patients presenting with an acute abdomen. Laparoscopic excision of intraabdominal cystic lymphangioma is an easy and safe procedure in children. We report one case of cystic lymphangioma in a 6-year-old female. The lesion was located on the left side of the transverse mesocolon. Laparocopic excision of the cyst was performed without complications.
Forme fruste choledochal cyst (FFCC) is one of the diverse types of choledochal cyst with little or no dilatation of the extrahepatic bile duct (EHBD). It is considered that FFCC has to do with the pancreatobiliary malunion (PBM). In children, 3 to 6 millimeters of EHBD is assumed to be normal. Even though there is no clear-cut definition, FFCC is likely to be associated with bile duct dilatation less than 10 millimeters. Almost all cases have PBMs and symptoms of the pancreatitis or cholangitis. We experienced a case of FFCC in a 4-year-old boy. His EHBD measures 10mm diameter. He had symptoms of pancreatitis and elevated hepatic transaminases. The pancreatobiliary common channel was 28 millimeters. He underwent EHBD resection and Roux-en-Y hepaticojejunostomy and was discharged with no specific complications.
Chylous mesenteric cyst is a rare variant of mesenteric cystic lesions. Pathologically there is lack of communication of the main lymphatic vessels, resulting in cystic mass formation. Clinical presentation is diverse and can range from an incidentally apparent abdominal mass to symptoms of an acute abdomen. A 5-year-old girl presented with abdominal distension without pain. CT scan showed a huge and thin-walled cystic mass without solid portion. Laparotomy showed a 20 x 18 cm sized huge mesenteric cyst containing chylous fluid. Pathological diagnosis was cystic lymphangioma.
A 19-month-old boy suffered from stridor and dysphagia. He was taking asthma medication for a few months, but symptoms did not improve. After admission, a chest CT showed a posterior mediastinal mass, which compressed the trachea and esophagus. The removed mass via open thoracotomy was a bronchogenic cyst on histopathology. Postoperatively, stridor and dysphagia disappeared. In case of persistent and refractory stridor or dysphagia in children, congenital lesions including bronchogenic cyst need to be ruled out.
Abdominal cystic lymphangiomas arising from the mesentery, omentum and retroperitoneum are rare and occasionally confused with other cause of acute abdomen. Sixteen children who underwent surgery for abdominal cystic lymphangioma between 1984 and 2005 at the Division of Pediatric Surgery, Keimyung University Dongsan Medical Center were evaluated retrospectively. There were 9 boys and 7 girls. Age ranged from 12 days to 13 years (mean age : 4.7years). The cysts were located in the omentum (4 cases),mesentery (9 cases : jejunum : 3, colon : 6). retroperitoneum (2 cases) and pelvic cavity (one case). The cyst content was hemorrhagic (8 cases), serous (5 cases), and inflammatory (2 cases), and chyle (one). Prenatal diagnosis was made in 3. The clinical features were variable, but abdominal pain, mass, and abdominal distention in order. There were 3 emergency operations in patients with complicated cyst, who were suspected of having panperitonitis and volvulus preoperatively. Complete excision was accomplished in all cases. There was one mortalityin a newborn with E.coli sepsis. Intestinal obstruction developed in 2 cases in long-term follow-up. No recurrence was observed. Although intraabdominal lymphangioma arising from mesentery, omentum and retroperitoneum are rare, it should be considered as a possible cause of acute abdomen.
Laparoscopic cholecystectomy has been increasingly used because of several advantages, less pain, better expectation for cosmesis (requires small incisions), and more rapid recovery compared with open cholecystectomy. Oral intake is tolerated on the day of operation or on the next. In this study, we evaluated the effectiveness and safety of laparoscopic cholecystectomy in children. Nine cases of laparoscopic cholecystectomy for acute and chronic cholecystitis in children were performed at Asan Medical Center between April 2002 and April 2004. Laparoscopic cholecystectomy was performed on a total of 10 patients, but one of them was excluded because of the simultaneous splenectomy for sickle cell anemia. Clinical presentation, operative findings, operation time, length of hospital stay, and postoperative complications were analyzed. Mean age was 10.4 (4–15) years, and only 3 of patients were less than 10 years. One patient was female. In 8 the diagnosis was calculous cholecystitis. Mild adhesions were found in 3 cases and intraoperative bile leakage in 2. There was no conversion to open surgery and there were no vascular, bowel, or bile duct injuries. Mean operation time was 82.2 (20–160) minutes ; mean length of hospital stay was 2.1 (1–3) day. There was no postoperative complication. Laparoscopic cholecystectomy in children was remarkably free of side effects and complications and had a short recovery time. Laparoscopic cholecystectomy for cholecystitis is considered to be a standard procedure in children.
Mature cystic teratoma, commonly called dermoid cyst, is the most common benign germ cell tumor of the ovary in children. Malignant transformation is rare, approximately 2%. As laparoscopic procedures are applied widely in pediatric surgery, a female chlid with a mature cystic teratoma may be an ideal candidate for laparoscopic surgery. Two children received laparoscopic operations successfuly for lower abdominal crises, twisted adnexa. There was no operative complication. Laparoscopic approach for ovarian lesions in infancy and childhood appears to be an effective and safe method for diagnosis as well as definitive therapy.
A 10-year-old-girl who underwent Roux-en-Y cystojejunostomy under the diagnosis of choledochal cyst at another hospital at the age of 3 months was referred to our hospital due to abdominal pain. Abdominal ultrasonography (USG) and computed tomography (CT) showed the type I choledochal cyst and multiple gall bladder stones. Severe inflammation and adhesion made difficulty of radical resection and only partial resection of choledochal cyst with Roux-en-Y hepaticojejunostomy could be performed. She complained of intermittent abdominal pain, fever, nausea and vomiting 2 1/2 years after the second operation. Follow-up abdominal CT scan showed the polypoid nodular lesion in the remnant choledochal cyst and suspicious metastatic lesion in the segment 7 of the liver. The duodenum was obstructed by the mass arising from the remnant choledochal cyst. The USG-guided liver biopsy revealed the moderately differentiated adenocarcinoma. A secondary palliative gastrojejunostomy was performed to relieve the obstruction of duodenum. She died of hepatic insufficiency 4 months later of third operation.
Failure of the urachus to regress completely results in anomalies that may be classified as patent urachus, urachal sinus, urachal cyst and bladder diverticula. The presenting symptoms of children with urachal anomalies are variable and uniform guidelines for diagnosis and treatment are lacking. The purpose of this study was to elucidate our conclusions regarding the presentation, diagnosis and treatment of urachal anomalies by reviewing our experiences. We retrospectively analyzed the records of 32 patients who were admitted for urachal anomalies from March 1995 to February 2005. The age distribution of these patients at presentation ranged from 1 day to 14 years old (median age 1 month) and they included 20 boys and 12 girls. The 32 cases comprised 13 cases of urachal sinus (40.6%), 10 urachal cyst (31.3%), and 9 patent urchus (28.1%). The presenting symptoms were umbilical discharge (14 patients), umbilical granuloma (8), abdominal pain and fever (3), fever (3), abdominal pain (2), and a low abdominal mass (2). In 30 patients ultrasonography was used for diagnosis and 2 patients with patent urachus were explored without using a diagnostic method. Twenty-three patients were confirmed by ultrasonography alone and 7 patients were examined using additional modalities, namely, computed tomography for 2 patients with an urachal cyst, magnetic resonance imaging for 1 patient with an urachal cyst, and fistulography for 3 patients with an urachal sinus. Excision was performed in 29 patients, and 3 patients were conservatively managed. Urachal anomalies in children most frequently presented in neonates, and the most common complaint was umbilical discharge with infection. Urachal anomalies can be diagnosed by a good physical examination and an appropriate radiographic test, and ultrasound was found the most useful diagnostic method. Complete surgical excision of an urachal anomaly is recommended to avoid recurrence, and even, though rare, carcinoma development.
Choledochal cysts have been associated with complications such as cholangitis, pancreatitis, and malignancy of the biliary tract. Recently, the incidence of choledochal cyst in neonate and young infant is increasing due to advances in diagnostic imaging. The aim of this study is to investigate the rationale of excision of choledochal cyst during the neonatal period. The clinical outcome and correlation between age at surgery and the degree of liver fibrosis were reviewed retrospectively. A total of 198 patients with choledochal cyst who were managed surgically between January 1985 and December 2000 at the Department of Surgery, Seoul National University Children's Hospital were included in this study. The overall outcome and the outcome of patients who were managed surgically during the neonatal period were compared. Correlation between age and the degree of liver fibrosis was evaluated by chi-square test and Pearson exact test. The mean age of the patients was 2 years 7 months (ranged from 5 days to 15 years). Mean postoperative follow-up period was 7 years 1 month (7 months to 20 years). The results are as follows. Twelve patients (6%) had postoperative complications, cholangitis (7), bleeding (4) and ileus (1). Eleven patients operated during the neonatal period had no postoperative complications. The positive correlation between age group and degree of liver fibrosis was statistically significant (chi-square: p=0.0165, Pearson exact test: p=0.019). The results support the rationale that excision of choledochal cyst can be performed safely without increasing morbidity in neonates.
With the development of fetal ultrasonography, detection of fetal ovarian cysts has been increased. Although ovarian cyst formation during the perinatal period is a self limiting process, there is still considerable controversy regarding the best treatment of the fetal ovarian cyst. The purpose of this study is to evaluate the natural history of fetal ovarian cysts and to analyze the result of treatment. From 1995 to 2004, 31 consecutive fetuses with ovarian cysts were followed by ultrasonography during the perinatal period. The fetal ovarian cyst was diagnosed by prenatal ultrasonography between 25weeks and 38 weeks and the mean size of the cysts was 5cm (ranged from 2 to 8cm). At birth, 3 cysts disappeared. In 2 cases, the diagnoses were changed to multicystic kidney disease and intestinal duplication. During following up of 26 cysts, 15 cysts have resolved completely. Seven cysts required oophorectomy because of cyst torsion (n=3), differentiation of tumorous condition (n=2), increased size of cyst (n=1), and large size (8cm) of cyst at birth (n=1). Fetal ovarian cyst should primarily be observed, and only in the limited cases, surgical treatment would be required for the risk of complications such as torsion and differentiation from benign to malignant pathology.
Biliary atresia (BA) with extrahepatic biliary cysts (EHBC) is a rare disease. It has been generally recognized as type I (correctable with cystic dilatation), which means a good prognosis. From a total of 73 patients with BA who underwent operation from September 1988 to September 2003 at our institute, 7 (9.6 %) cases of type III BA with EHBC (uncorrectable with cystic dilatation) are reviewed. Clinical findings, laboratory data, radiologic findings, treatment methods and outcomes were reviewed. Female was more prevalent (male to female ratio; 2:5). All cases were type III with EHBC according to the intraoperative cholangiography, and underwent Kasai's portoenterostomy. The mean age was 57 days at operation. Three patients(42.9 %) are long term survivors. Further evaluation is needed to determine the correlation between prognostic factors and outcome for.
Ovarian cyst is found in 32% of necropsies in neonates, and can be visualized during gestation by ultrasonography. The clinical evolution of these cysts is variable, but in most cases the prognosis is favorable. Ovarian torsion, bleeding, rupture, and peritonitis have been described as complications. We report a newborn girl with torsion of ovarian cyst. A cystic mass measuring 41.9x31.9 mm on left side of abdomen was identified at 32 weeks of gestation by fetal ultrasonography. Surgery was performed after birth.
Improvement in prenatal ultrasonography is leading to diagnose choledochal cyst before birth and before onset of classical symptom more frequently. But, there is a controversy about optimal timing for cyst excision of prenatally diagnosed asymptomatic choledochal cyst. To identify the most appropriate timing for surgery in prenatally diagnosed choledochal cysts, we analyzed 6 patients who had operation for choledochal cysts within 30days after birth at the division of Pediatric Surgery, Samsung Medical Center and Inha University School of Medicine, from June 1995 to June 2002. Males were four and females 2, the mean age at operation was 11.2 days, and the median age 8.0 days. The range of gestational ages of the antenatal diagnosis of bile duct dilatation was 24 weeks to 32 weeks, mean was 38.3 weeks, and mean birth weight was 3,298.3 g. After birth, abdominal ultrasonography, hepatobiliary scintigraphy, and magnetic resonance cholangiopancratography (MRCP) were performed. Mean age at operation was 11.2 days. All patients had the cyst excision and Roux- en-Y hepaticojejunostomy. Immediate postoperative complication was not found. During the median follow-up period of 41 months, one patient was admitted due to cholangitis, and the other due to variceal bleeding. Early operative treatment of asymptomatic newborn is safe and effective to prevent developing complications later in life.
Congenital dilatation of the common bile duct (choledochal cyst) is an uncommon disease. Although the etiology is unknown yet, various theories such as distal obstruction of the common bile duct, congenital weakness of the duct and anomalous union of the pancreaticobiliary duct have been offered to explain the occurrence of choledochal cyst. Thirty - six cases of choledochal cyst over 22 years were analyzed clinically and classified according to Todani's classification and Kimura's anomalous union of pancreaticobiliary duct type. Todani type I consisted with 22 cases which were subdivided into 19 cases of type Ia, 1 case of type Ib and 2 of type Ic. Type IVa consisted with 14 cases including one case of Caroli's disease. There were 25 type BP cases and 10 type PB cases and 1 normal pancreatobiliary junction. Serum alkaline phosphatase was increased significantly in almost all cases. Seven patients (19.4%) had associated congenital anomalies such as double gallbladder, left - sided gallbladder, common bile duct web, biliary atresia, accessory hepatic duct, heterotopic pancreas, cleft lip and 2 cases of intestinal malrotation. All patients underwent cyst excision and Roux - en - Y hepaticojejunostomy and cholecystectomy. There was one death due to methicillin resistant Staphylococcus aureus sepsis.
A 10-year-old boy was admitted with blunt abdominal trauma by bike handle injury. The patient was operated upon for a generalized peritonitis due to pancreaticoduodenal injury. On opening the peritoneal cavity, complete transection of distal end of common bile duct and, partial separation between pancreas head and second portion of duodenum were found. Ligation of the transected end of the common bile duct, T-tube choledochostomy, and external drainage were performed. A pseudocyst was found around the head portion of the pancreas on the 7th postoperative day with CT. An internal fistula had developed between the pseudocyst and ligated common bile duct. The pseudocyst was subsided after percutaneous drainage. In the case of the undetermined pancreatic injury, percutaneous external drainage can be effective in treating the traumatic pancreatic pseudocyst in a pediatric patient.
A nationwide survey on Choledochal cyst was undertaken among 39 members of the Korean Association of Pediatric Surgeons. The members were required to complete a questionnaire and the case registration form for each patient during the five-year period of 1997 to 2001. Three hundred and forty eight patients were registered from 32 institutions. The average number of patients per surgeon was one to two every year. The male to female ratio was 1: 3.4. The age of patients on diagnosis was 49.0±44.4 months. The geographic distribution was 34.8% in Seoul and Kyoungki-do, 33.3% in Kyoungsang-do, 17.9% in Cholla-do, and 8.5% in Choongchung-do, in order of frequency. The three common clinical presentations were abdominal pain (63.8%), vomiting (35.3%), and jaundice (29.1%). Only seven patients (2%) presented with classic triad, and 25 patients were diagnosed by antenatal ultrasonographic examination. According to the Todani classification, 238 patients (71.3%) were type I, 3 (0.9%) type II, and 93 (27.8%) type IV. At the time of the operation, three important associated conditions were choledocholithiasis in 45 patients (15.1%), liver fibrosis (Grade 1-4) in 35, and previous operative procedure for biliary diseases in 10. Associated anomalies were observed in 13 patients (3.8%). Three hundred thirty nine (98.8%) of 343 lesions were treated by cyst excision and Roux-Y hepaticojejunostomy. One hundred seventy-six patients had an anomalous arrangement of the pancreatobiliary ductal system: APBD was not in 92 patients, biliary duct joined to the pancreatic duct in 51, and pancreatic duct joined to the biliary duct in 26. There were 8.5% early, and 7.7% late phase operative complications. The major complications were bleeding, anastomotic leakage, and acute pancreatitis. The combination of acute abdomen and choledochal cyst may suggest spontaneous rupture. Because of the development of late intrahepatic bile duct stones, long-term follow-up after cyst excision and hepaticojejunostomy is required. The optimal time of surgical intervention should also be considered in the situation of routine use of antenatal ultrasonographic examination. This is the first review of the choledochal cyst in Korea and provides baseline data for future comparisons.
Lymphangiomas or cystic hygromas are quite commonly seen in children. During a 22-year period, from January 1980 to December 2001, 117 patients with lymphangioma were treated and followed in the Department of Pediatric Surgery at Hanyang University Hospital. The male-to-female ratio was 1.9:1 (77:40) with a male preponderance. As for the age incidence at time of diagnosis, 10 (8.5 %) patients were noted under 1 month of age, 37 (31.6 %) were between 1 month and 1 year of age, 12 (10.3 %) between 1 and 2 years of age, so 59 (50.4 %) were under 2 years of age. Sixty one (52.1 %) lymphangioma-cases were located in the neck, including one case at the nape. Axilla was the second in frequency and the rest were scattered at various sites. The intrascrotal lymphangioma is very rare but we have experienced one case of primary intrascrotal lymphangioma. Eighteen (15.4 %) cases were located in the intraabdominal area, 10 in the mesentery, 2 in the greater omentum and 6 in the retroperitoneum. The chief complaints of intraabdominal lymphangioma were abdominal pain, intestinal obstruction, inguinal hernia, palpable mass, and/or abdominal distension. Among 77 histologically proven cases, 14 cases were cavernous lymphangiomas and the rest were cystic lymphangiomas. Bleeding in the lymphangioma was noted in 20 (17.1 %) cases of all. As for the treatment, a complete excision was performed in 77 (65.8 %) patients and AgNO3 sclerotherapy after incomplete excision was performed in 23 (19.7 %). Picibanil (OK-432) sclerotherapy was performed in 17 (14.5 %) patients. Recurrence rate was 7.7 % and mortality occurred in one case who had a large neck lymphangioma extending into the mediastinum.
Mesenteric and omental cysts are rare intra-abdominal lesions in childhood, and may present various clinical features such as an asymptomatic mass or an acute abdomen. Therefore, these entities are frequently misdiagnosed preoperatively or are found only incidentally at operation for other conditions. We analyzed our experiences of 19 cases in a 19 year period from 1981 to 1999, at College of Medicine, Catholic University of Korea. There were 12 boys and 7 girls with a mean age of 4.8 years (range, 3 days to 15 years). Common presenting symptoms were abdominal pain (47%), abdominal distension (31%), abdominal mass (24%), vomiting (15%) and fever (10%). Ultrasonography was the most preferred method of diagnosis. Other diagnostic modalities include CT, MRI, and abdominal ascites tapping in selected patients. Location of the mesenteric cysts was small bowel mesentery in nine, the right mesocolon and retroperitoneum in one, the left mesocolon in one, and the jejunum, sigmoid-colon mesentery in one. Most of the patients underwent cyst excision, but six patients required concomitant bowel resection for complete removal of the lesions, and two patients underwent unroofing and simple aspiration respectively. There was one mortality case due to sepsis.
Branchial anomaly is a frequently occurring congenital abnormality in childhood. It is important for the pediatric surgeon alike to be familiar with the embryology and differentiation of head and neck structure to accurately diagnose and treat these lesions. Eighty-five patients with branchial anomaly treated at Hanyang University Hospital between 1980 and 2001 were reviewed to determine relative frequency, clinical classification and appropriate treatment. The male to female ratio of branchial anomaly was 1.2:1. The most commonly presenting age was before 1 year (32 %) and the age group between 1 and 3 year (22 %) followed it. According to the classification of branchial anomalies, 73 of 85 cases were second branchial anomaly, 9 had the first type and 3 did fourth type. One patient showed combined anomalies of the first and the second type. Infection sign were seen in 70 % of patients at the time of the first visit to our hospital and also patients' symptoms were frequently related with the infection. Forty-one cases (48 %) were fistula, 21 (25 %) were cysts, 21 (25 %) were sinuses, and two were only cartilage remnants. The most common type of the branchial anomalies is the second branchial fistula and the most common symptoms of the anomalies are related with infection. Initial proper diagnosis and anatomical classification of the anomalies are very important in managing the lesions. The efforts to find the exact anatomical location of the fistula or sinus tract are necessary because total excision of the lesions including those tracts is the only way to prevent recurrence.
Thyroglossal duct cyst is ectodermal remnant, which may develop along the line of descent of the thyroid gland from the foramen cecum of the tongue to the pyramidal lobe of the thyroid gland. Meticulous dissection of the cyst and duct, along with the body of the hyoid bone is necessary to avoid recurrence. Eighty-one patients with thyroglossal duct cyst treated at Hanyang University Hospital between January 1980 and December 2000 were reviewed to determine the incidence and to analyze the result of management. The male-to-female ratio was 1.4:1 (47:34) with a male preponderance. They are most commonly present at 3-8years (54.2%) of age, but rarely present at infancy. The most common symptom was a painless midline neck mass (76.5%, 62cases). Eighty-one patients underwent modified Sistrunk operation without evidence of recurrence. Eight-nine percent (72 cases) of these lesions were located between thyroid substance and hyoid bone, and 11% (9 cases) were above the hyoid bone. There were 22 infected cysts (27.2%). The Sistrunk operation is a gold standard for treating the thyroglossal duct cysts. For best results in thyroglossal duct cyst surgery, one should make every effort to remove the cyst intact in continuity with the body of the hyoid bone. In our institute, Sistrunk operation modified by the authors showed a good result.
Congenital anomalies in the head and neck region such as preauricular sinus and skin tag, thyroglossal duct cyst, branchial anomaly, cystic hygroma and dermoid cyst are common in pediatric population. It is important for pediatricians and pediatric surgeons to be familiar with the embryology and the anatomical characterics of these lesions in order to diagnose and treat properly. Three hundred nineteen patients with congenital head and neck anomalies treated at Hanyang University Hospital between 1980 and 1999 were reviewed to determine the relative frequency of the anomalies and to analyze the method of management. Eight-four patients(25.1%) of 335 lesions had preauricular sinus and skin tag, 81 patients(24.2%) had thyroglossal duct cyst, 81 patients(24.2%) had branchial anomaly, 58 patients(17.3%) had cystic hygroma, 31 patients(9.2%) had dermoid cyst. The male-to-female ratio was 1.4:1. The thyroglossal duct cyst was most commonly present at 3-5years, however branchial anomaly was commonly diagnosed in children younger than 1 year. Preauricular sinus shoeed familial tendency in three patients and bilaterality is 33.8%. Most head and neck anomalies in children had clinical and anatomical characterics. A careful history and physical examination were very useful for diagnosis and proper management. The initial surgery should be done by experienced pediatric surgeonsl since the recurrence rate after incomplete surgical excision could be high.
Pseudoaneurysm of splenic artery may arise from a vascular erosion by the inflammatory processes around the splenic artery, particularly in acute pancreatitis and chronic pancreatitis, which may cause rupture of pseudoaneurysm and life threatening hemorrhage. Collective experience with this massive hemorrhage is attended by a high mortality rate even with prompt therapy, and conservative management is associated with an almost 100 per cent of mortality rate. Identification of the bleeding site at laparotomy may be exceedingly difficult, which makes the preoperative detection of bleeding source desirable. Peripancreatic vascular lesions can be identified by angiography, and in selected cases the risk of urgent operation to control massive hemorrhage may be obviated by embolization. The authors have recently experienced a case of ruptured splenic artery pseudoaneurysm combined with a pancreatic pseudocyst in a 6 years old boy. A bolus enhanced CT scan and angiography were essential to confirm these complications of pancreatic pseudocyst. We managed this child successfully with an urgent procedure of transcatheter arterial embolization and another elective surgery of pancreatic pseudocyst.
Solid and papillary cystic neoplasm of pancreas is an uncommon low grade malignant tumor found predominantly in young female in their second or third decade of life, and amenable cure by surgical treatment. The authors report two cases of solid and papillary neoplasm of pancreas pathologically verified at Kyung Hee university hospital. The first case was 11-years old male patient and the other case was 12-years old male patient. Symptoms of two patients were abdominal discomfort, nausea and vomiting and abdominal pain in the female patient. CT finding of solid and papillary neoplasm of pancreas depict a well-demarcated mass with solid and cystic necrosis component. In female patient, large hematoma was shown. Gross findings of tumor revealed apparent encapsulation, cystic degeneration and hemorrhagic necrosis. Microscopically the tumors were characterized by distinctive solid and papillary patterns of cellular arrangement without local invasion. All patients were discharged and follow up without any problem.
Splenic cysts are uncommon and classified as either primary(true) or secondary(pseudo-) depending on the presence or absence of a true epithelial lining. True cysts (epidermoid cyst) of the spleen are very rare. Three cases of splenic cysts in childhood were treated at the Yeungnam University Hospital in the last eleven years(1989 - 1999). Two of patients were girls. The ages at diagnosis were 7, 12 and 15 years. Abdominal ultrasonography and computerized tomography were utilized for the diagnosis. Radionuclide scanning was performed in one patient. Surgical resection(one partial splenectomy and two total splenectomies) was performed. The sizes of cysts were 4, 6.5 and gem in maximum demension.
A 6(1/2)-year-old girl developed recurrent cholangitis following hepatic portoenterostomy for biliary atresia. Computed tomogram showed an ovoid cyst (4.5 × 4.0 cm in size) in the left hepatic lobe and another tubular dilatation (2.0 × 0.8 cm in size) in the right hepatic lobe. Percutaneous transhepatic cholangio-drainage (PTCD) with cystogram showed an ovoid cyst in the left hepatic lobe (Tsuchida type A), measuring 6.6 × 5.0 cmin size. She became afebrile and anicteric with aid of PTCD and parenteral antibiotics. However she continued to drain 45-150 cc of bile per day via the tube for over 2 weeks. Then she successfully underwent intrahepatic cystojejunostomy with guidance of intraoperative ultrasonography. This case illustrates relapsing cholangitis caused by Tsuchida type A intrahepatic cyst, which was successfully managed with PTCD followed by internal drainage procedure.
To study the role of anomalous pancreatico-biliary ductal union (APBDU) in the development of choledochal cyst, we reviewed 23 cases. APBDU is defined as a long common channel(>0.4 mm). The patients ages ranged from 1 week to 112 months and the mean age was 22.5 months. Right upper quadrant pain was the most prevalent symptom. The diagnosis was made by ultrasonography and operative cholangiography in most patient. The preoperative diagnosis was made in 100 % of the cases. Gallstones were found in 5 cases. Todani type I and type IV were prevalent. A long common channel was found in all cases. The operative treatment consisted of cyst excision and Reux-en-Y hepaticojejunostomy or choledochojejunosotmy. One patient had postoperative pancreatitis. There was no mortality. We conclude that detection of choledochal cyst is occurring at a younger age and APBDU seems to play an important role in the pathogenesis of type I and IV cysts. Cyst excision is the treatment of choice to eliminate repeated cholangitis and malignant transformation.
Choledochal cyst is rare in the western countries, but common in oriental countries. Complicatioins include ascending cholangitis, recurrent pancreatities, progressive biliary cirrhosis, portal hypertension, stone formation and later malignant transformation. Bile peritonitis secondary to rupture is one of the rarest complications, with an incidence of 1.8 % to 18 %. The anomalous arrangement of the pancreatobiliary ductal system with a long common channel may cause inflammation leading to perforation of the cyst. The authors found 4 cases (14.2 %) of bile peritonitis among 28 cases of choledochal cyst treated from Jan. 1983 to Jan. 1998. The patients ages ranged from 6 months to 3 years and three were female. The perforation sites were located on the common bile duct at its junction with the cystic duct in 2 cases, the distal cyst wall in 1 case and the left hepatic duct at its junction with cyst in 1 case. The types of choledochal cysts by Todani's classification were Type IVa in 3 cases and type I in 1 case. By the new Komi's classification utilizing operative cholangiogram there were 2 cases of Type Ia, 1 case of type IIb and 1 case of type III. One stage cyst excision and hepaticojejunostomy(Roux-en Y type) was done in 3 cases, and two staged operation in 1 case. All patients had an uneventful course postoperatively. The average day of discharge was 9.8th postoperatively. In conclusion, primary excision of the choledochal cyst and biliary reconstruction is a safe and effective treatment of ruptured choledochal cyst in infants.
The embryological and anatomical features of urachal anomalies have been well defined. Because of the variable clinical presentation, uniform guideline for evaluation and treatment are lacking. Although urachal remnants are rarely observed clinically, they often give rise to a number of problems such as infection and late malignant changes. Therefore, a total assessment of the disease with a particular focus on embryology, anatomy and clinical symptoms, as well as the most advisable management, is called for. Twenty six patients with urachal remnants were treated at the Department of Pediatric Surgery from August 1980 to June 1998. Of these 26, 9 were classified as patent urachus, 11 as urachal sinus, 4 urachal cyst, 1 urachal diverticulum and 1 alternating sinus. The group consisted of 11 males and 15 females. The age distribution was 20 neonates, 3 infants, 2 preschoolers and 1 adult. Infection was the most frequent complication and Staphylococcus aureus was the predominant causative microorganism. Fistulogram was performed in 4 cases and ultrasound examination disclosed cysts or sinus in 7 cases. Excision was performed in 24 patients and incision and draniage in 2 cases as a primary treatment. There was no postopreative complication or recurrence.
The anomalous pancreaticobiliary duct union (APBDU) might cause the formation of choledochal cyst and malignancies of hepatopancreaticobiliary system. The purpose of this study is to make an experimental animal model of APBDU similar to that of human. One to two-month-old Mongrel dogs (n=12) were divided into two groups; the control group (n=2) had a sham operation performed, and in the experimental group (n= 10) the end of distal' common bile duct (CBD) was anastomosed to the side of the dorsal pancreatic duct making APBDD. Serum was obtained for chemical analysis on the 10th postoperative day. The dogs were sacrificed at the 5th week (n=3), the 6th week (n=3), the 7th week (n=2), the 8th week (n=2) and the 6th month (n=2) after the experimental surgery. With sacrifice, operative cholangiogram was taken, and bile juice was obtained for chemistry and bacterial culture. The en-bloc specimens of the hepatopancreaticobiliary system were removed for microscopic examination. Serum and bile juice amylase levels were elevated in the experimental group (n=10), but not in the control group (n=2). Operative cholangiograms of control group revealed no evidence of bile duct dilatation.. On the other hand, the bile duct in the experimental group was markedly dilated without any evidence of stenosis at the anastomosis site (n=10). Histologic examination of the hepatopancreaticobiliary system in the experimental group resembled the findings of choledochal cyst in human. The APBDU of this animal model can produce bile duct dilatation by pancreaticobiliary reflux. We think that this animal model can be potentially promising for the research about the APBDU associated hepatopancreaticobiliary diseases.
We have treated a case of pseudocyst of transverse mesocolon in 3-year-old male child. Operative findings demonstrated that the pseudocyst originated in the transverse mesocolon, and was not connected to the pancreas. A colonic duplication was found incidentally near the pseudocyst. On microscopic examination, ectopic pancreatic tissue was noted in the transverse mesocolon. This pseudocyst was thought to have originated from the ectopic pancreas of the transverse mesocolon. This is the first reported case of pseudocyst originated from ectopic pancreas of the transverse mesocolon, combined with a colonic duplication. The pathogenesis is discussed.
Mesenteric and omental cysts are rare lesions in childhood. These cysts are morphologically and pathologically similar to lymphangiomas that occur in other parts of the body. From 1980 to 1997, 8 children were diagnosed and treated for mesenteric or omental cysts. Their ages ranged from 18 days to 6 years. There were 5 boys and 3 girls. The main presenting symptom was abdominal pain. Operative procedures were complete cysts excision, complete excision with intestinal resection, or complete excision with intestinal resection and colostomy. Accurate preoperative diagnosis was possible with the current ultrasonographic imaging techniques. Complete excision of the lesion was possible in all patients and results were excellent.
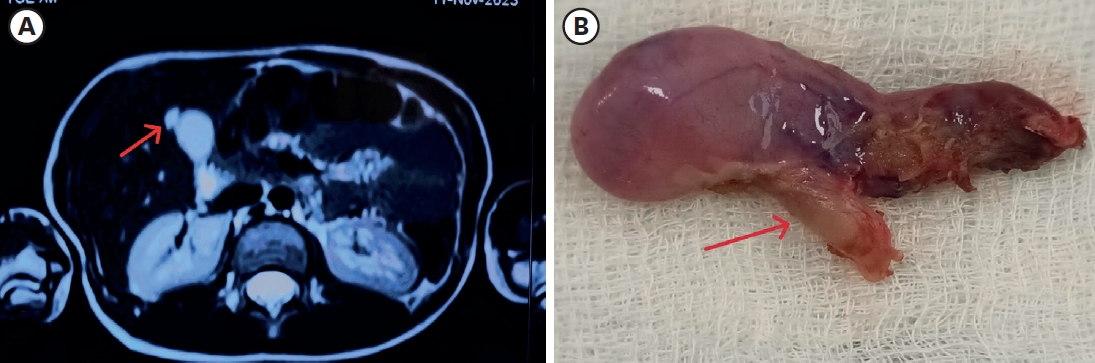
Pulmonary sequestration is a complex anomaly involving the pulmonary parenchymal tissue and its vasculature. It presents as a cystic mass of nonfunctional lung tissue without communication with the tracheobronchial system. Usually, it receives blood supply from anomalous systemic vessels. Therefore, preoperative diagnosis of the pulmonary sequestration is difficult, especially when it is located in the abdomen and combined with congenital cystic adenomatoid malformation (CCAM). We encountered such a mass(CCAM type 2) detected prenatally by ultrasonography. It was a kidney bean shaped, pinkish mass straddling the thorax and abdomen on the right side. Because of the sonographic appearance, neuroblastoma was diagnosed preoperatively. The mass was completely extirpated without difficulty.
Two cases with papillary cystic neoplasm of the pancreas are reviewed and discussed. Up to recently, the tumors have been misclassified as nonfunctioning islet cell tumor or carcinoma, acinar cell carcinoma, papillary cystadenocarcinoma, or pancreatoblastoma. It frequently has been managed with aggressive surgery such as pancreatoduodenectomy. The tumors are well encapsulated and the cut surfaces are characteristically solid and hemorrhagic. Ultrasonography and CT scan are the most useful tools for the diagnosis. The neoplasms usually behave like a very low grade malignancy, so complete removal is the treatment of choice for the tumor arising anywhere in the pancreas. We have a boy and a girl who have papillary cystic neoplasm. The boy was 12 years old and the girl was 14 years old. Both underwent distal panereatectomy and the progress were uneventfuL We have a boy and a girl who have papillary cystic neoplasm. The boy was 12 years old and the girl was 14 years old. Both underwent distal pancreatectomy and the progress were uneventful.

