ABSTRACT
-
Purpose
This study aims to investigate and compare the incidence, demographic characteristics, clinical manifestations, preoperative diagnostic methods, anatomical classifications, associated anomalies, operative treatments, and postoperative outcomes of patients with intestinal atresia treated by the members of the Korean Association of Pediatric Surgeons (KAPS) through three nationwide surveys.
-
Methods
KAPS conducted 3 national surveys in 1998, 2010, and 2024 to examine the patients diagnosed with intestinal atresia. In preparation for the survey, we developed a customized case registration form to obtain data on patient sex, birth weight, gestational age, clinical manifestations, preoperative diagnostic methods, anatomical types, associated anomalies, operative treatments, and postoperative outcomes. Authorized KAPS members completed the case registration form.
-
Results
The first, second, and third national surveys included 218, 222, and 236 individuals diagnosed with intestinal atresia, respectively. The male-to-female ratios were 1.5:1, 1.1:1, and 1.1:1, respectively. The first, second, and third national surveys revealed that 34.3%, 43.3%, and 53.4% of patients were born before 37 weeks of gestation, respectively. Additionally, 28.7%, 32.0%, and 40.7% of patients had a birth weight under 2,500 g. In the third national survey, duodenoduodenostomy was the most common procedure, performed in 70 out of 82 patients diagnosed with duodenal atresia. Resection and anastomosis were the main surgical procedures conducted in 47 out of 54 cases of jejunal atresia and 74 out of 92 cases of ileal atresia. The mortality rates in the first, second, and third national surveys were 13.8%, 3.6%, and 1.3% respectively, with the lowest rate observed in the third national survey.
-
Conclusion
These national surveys offer valuable insights into the current state of intestinal atresia, including specific surgical interventions and postoperative outcomes in South Korea. For pediatric surgeons aiming to enhance their understanding of intestinal atresia and its treatment options, these surveys could be an indispensable resource and guide.
-
Keywords: Intestinal atresia; Children; Survey
INTRODUCTION
Intestinal atresia is a severe congenital abnormality characterized by the obstruction of the intestinal lumen, leading to substantial morbidity and mortality. Prompt surgical interventions and comprehensive postoperative care are crucial for ensuring survival and improving the quality of life in affected infants. The cause of intestinal atresia is complex and diverse, involving genetic, environmental, and developmental factors. Duodenal atresia (DA) arises from failed recanalization at the end of the second month of embryonic development, while jejunal atresia (JA) and ileal atresia (IA) are caused by vascular accidents disrupting the blood supply to the small intestine. Advancements in surgical techniques and postoperative intensive care have significantly improved the survival rates for patients with intestinal atresia. The Korean Association of Pediatric Surgeons (KAPS) conducted three retrospective national surveys to examine data on intestinal atresia in South Korea [
1,
2]. The results of these surveys were analyzed and discussed at the 14th, 26th, and 40th annual spring meetings of the KAPS, respectively. The findings of the first and second national surveys were published in the
Journal of the Korean Association of Pediatric Surgeons in 1999 [
1] and 2010 [
2], respectively. This study aims to analyze trends and identify changes in the incidence, demographic characteristics, clinical manifestations, preoperative diagnostic methods, anatomical classifications, associated anomalies, operative treatments, and postoperative outcomes of patients with intestinal atresia in South Korea by comparing the findings of the first 2 national surveys with the recently conducted third national survey.
METHODS
Between 1994 and 1996, 28 KAPS members working in South Korea participated in the first national survey on intestinal atresia. The second national survey was conducted between 2007 and 2009. The third national survey was also conducted between 2021 and 2023. For the third national survey, we developed a case registration form to collect data on patient sex, birth weight, gestational age, clinical manifestations, preoperative diagnostic methods, anatomical types of intestinal atresia, associated anomalies, operative treatments, and postoperative outcomes. This form was distributed to 22 pediatric surgical centers and completed by authorized KAPS members representing 236 patients. Owing to differences in the case registration forms utilized in the first, second, and third national surveys, direct comparison of the data was impeded. Nevertheless, the data collected from the three national surveys were compared using statistical validation methods to the greatest extent possible. Continuous variables were first tested for normality using the Shapiro–Wilk test. Variables with a normal distribution were presented as means and standard deviations, while those with a non-normal distribution were presented as medians and interquartile ranges. Comparisons between the two groups were made using the Independent Samples t-test and the Mann–Whitney U test for normally distributed and non-normally distributed variables, respectively. Categorical variables were analyzed using the χ
2 test or Fisher’s exact test. All analyses were conducted using the R project for Statistical Computing, Version 4.4.0 (R Development Core Team, Vienna, Austria;
https://www.r-project.org), and p-values <0.05 were considered statistically significant. The study protocol was approved by the Institutional Review Board (IRB) of Kyungpook National University Hospital (IRB No. 2024-03-007).
RESULTS
1. Registered case numbers and incidence by surveys
In the first national survey, 218 patients were included, comprising 73, 72, 71, and 2 patients diagnosed with DA, JA, IA, and colonic atresia (CA), respectively. The second national survey comprised 222 patients, including 76, 65, 78, and 3 patients with DA, JA, IA, and CA, respectively. In the third national survey, 236 patients were included, comprising 82, 54, 92, and 8 patients with DA, JA, IA, and CA, respectively. The respective intestinal atresia incidence rates determined by the surveys were 1 in 9,759, 1 in 6,340 and 1 in 3,135 (
Table 1).
The first national survey included 130 males and 88 females, with a male-to-female ratio of 1.5:1. In the second national survey, the male-to-female ratio was 1.1:1, with 117 males and 102 females. The third national survey comprised 122 males and 114 females, also reflecting a 1.1:1 male-to-female ratio. Gestational age under 37 weeks was observed in 34.3%, 43.3%, and 53.4% of patients in the first, second, and third national surveys, respectively. Additionally, birth weights below 2,500 g were found in 28.7%, 32.0%, and 40.7% of patients in the first, second, and third national surveys, respectively. In the first, second, and third national surveys, 43.6%, 68.9%, and 69.1% of the patients were diagnosed via prenatal examination, respectively. Polyhydramnios was observed in 28.9%, 36.5%, and 39.0% of pregnancies in the first, second, and third national surveys, respectively (
Table 2).
The most common symptom of intestinal atresia in the third national survey was abdominal distention, affecting 26, 39, 75, and 6 patients with DA, JA, IA, and CA, respectively. Other prevalent symptoms included bilious aspirate, observed in 24, 34, 44, and 2 patients, and feeding intolerance in 33, 12, 41, and 4 patients with DA, JA, IA, and CA, respectively (
Table 3).
Abdominal X-rays were the most frequently used diagnostic imaging, performed on 81 (98.8%), 54 (100.0%), 88 (95.7%), and 7 (87.5%) patients with DA, JA, IA, and CA, respectively. Abdominal ultrasonography was also performed on 72 (87.8%), 45 (83.3%), 74 (80.4%), and 7 (87.5%) patients with DA, JA, IA, and CA, respectively (
Table 4).
The most frequently associated anomalies were cardiovascular in nature, found in 43, 21, 40, and 4 patients with DA, JA, IA, and CA, followed by gastrointestinal anomalies in 25, 21, and 22 patients with DA, JA, and IA, respectively (
Table 5). Among gastrointestinal anomalies, malrotation was the most common, observed in 15, 8, 5, and 1 patient with DA, JA, IA, and CA, followed by meconium peritonitis in 12 and 13 patients with JA and IA, and esophageal atresia in 4 and 1 patients with DA and IA, respectively (
Table 6).
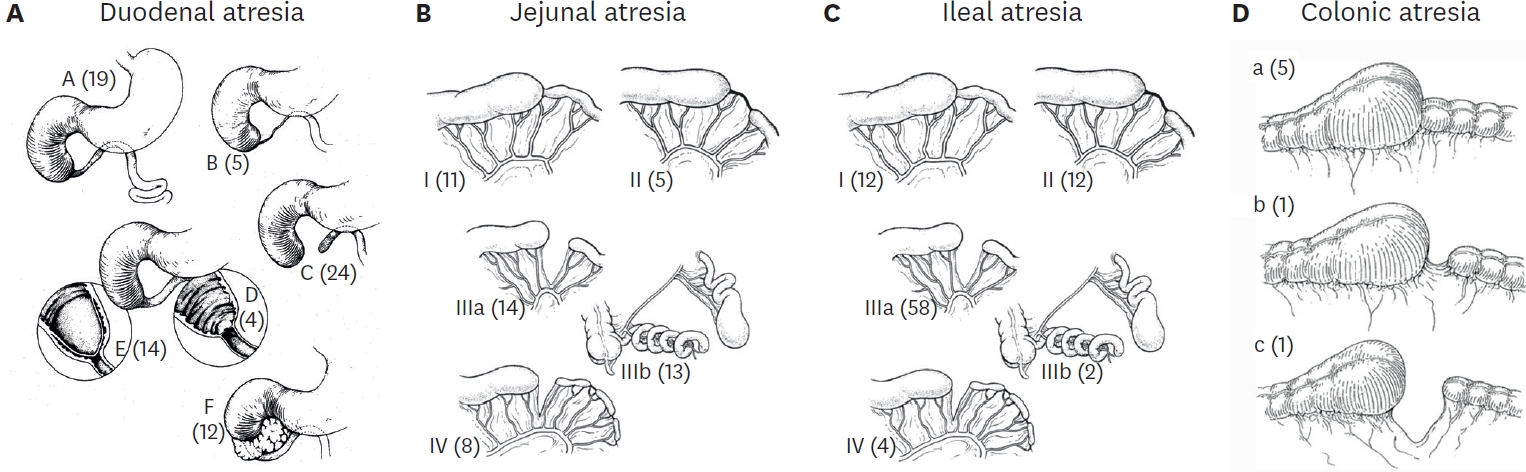
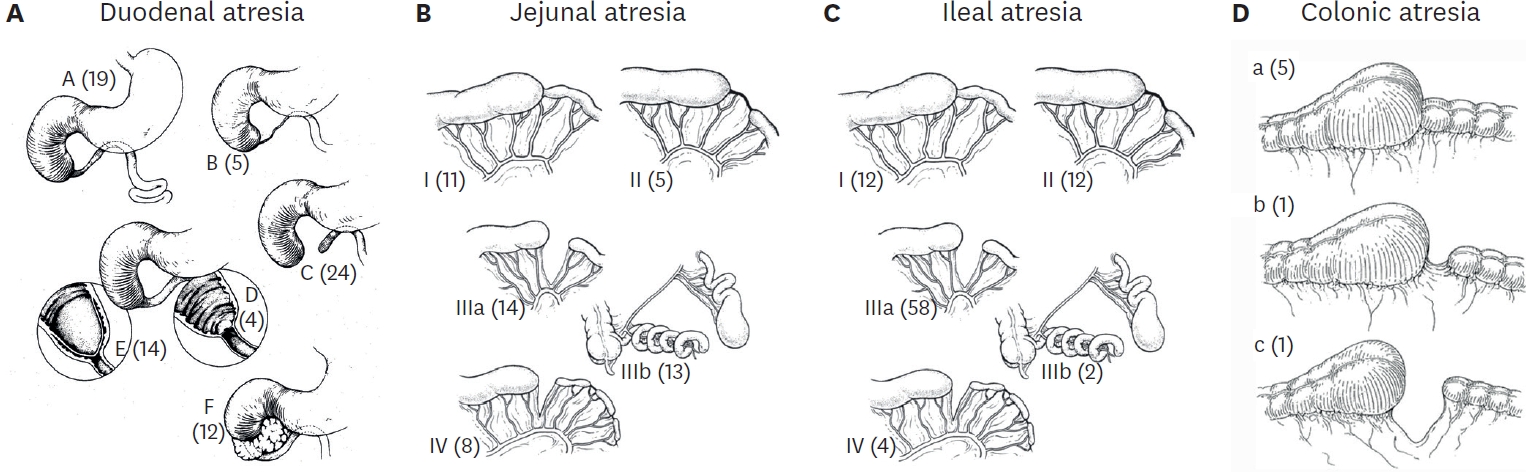
Fig. 1 shows the anatomical classification of DA, JA, IA, and CA. Type C was the most common anatomical type of DA, found in 24 patients, followed by types A, E, and F in 19, 14, and 12 patients, respectively. Type IIIa was the most common anatomical type of JA observed in 14 patients, followed by types IIIb, I, and IV in 13, 11, and 8 patients, respectively. Type IIIa was the most common anatomical type of IA observed in 58 patients, followed by types I and II in 12 and 12 patients, respectively. Type I was the most common anatomical type of CA in 5 patients.
7. Operative treatment of intestinal atresia in the third national survey
Tables 7-
10 summarize the operative treatment of DA, JA, IA, and CA based on their anatomical types, categorized by different surgical procedures. Each table includes the number of cases for each type of operation, with laparoscopic procedures indicated in parentheses. For DA, duodenoduodenostomy was the most common procedure, performed in 70 patients, including 13 laparoscopic surgeries, while duodenojejunostomy was performed in 4 patients. Resection and anastomosis were the most frequently performed in 47 patients with JA, including three laparoscopic surgeries, and in 74 patients with IA, including 1 laparoscopic surgery. For CA, resection and anastomosis were performed in 5 out of 8 patients. Plication or tapering enteroplasty was performed in 13.6% and 8.8% of the patients in the second and third national surveys, respectively (
Table 11).
8. Postoperative complications in the third national survey
Early postoperative complications included intestinal obstruction in three, four, and three patients with DA, JA, and IA and wound infection in two and six patients with DA and IA, respectively. Stenosis occurred in 5, 1, and 1 patients with JA, IA, and CA, respectively. Leakage was observed in 1 patient, each with DA, JA, and IA. Late postoperative complications included intestinal obstruction in 6 and 9 patients with JA and IA and total parenteral nutrition-related cholestasis in 2 and 4 patients with JA and IA, respectively (
Table 12).
In the second national survey, the time to full feeding for JA (23.7±17.5 days) was longer than that for DA (14.9±7.2 days) and IA (17.1±16.3 days), which was statistically significant (p<0.05). In the third national survey, the time to full feeding for JA (23.5 [15.0–43.5] days) was also longer than that for DA (13.0 [9.0–17.0] days) and IA (13.0 [10.0–23.0] days), which was also statistically significant.
In the third national survey, hospital stays were the longest for JA, with a median of 40.0 (32.0–79.0) days compared to that for DA (26.0 [18.0–44.0] days) and IA (27.0 [17.0–47.0] days) (
Table 13).
The mortality rate of the patients was 13.8% in the first national survey, subsequently decreasing to 3.6% in the second national survey and further declining to 1.3% in the third national survey (
Table 14).
DISCUSSION
Numerous national cohort studies on intestinal atresia have been conducted globally, with their results well-documented [
3-
6]. The incidence, treatment approaches, and surgical outcomes for intestinal atresia vary widely across different geographical areas and healthcare systems. Understanding these differences is crucial for improving clinical practices and patient outcomes worldwide. The national surveys provide valuable insights into the epidemiology, treatment strategies, and prognostic factors associated with intestinal atresia, enabling comprehensive comparisons and identification of optimal treatments. In South Korea, three nationwide surveys on intestinal atresia were conducted between 1994 and 2023, spanning 30 years. The results of these surveys are summarized below. First, despite a declining birth rate in South Korea, the number of patients diagnosed with intestinal atresia showed a slight increase across the surveys: 218, 222, and 236 in the first, second, and third national surveys, respectively. Second, a rise in the number of patients with preterm and low birth weights was observed, along with an increase in the rate of prenatal diagnosis from the first to the third national survey. Third, laparoscopic surgery was not performed during the first or second national survey in South Korea. Nevertheless, the third national survey revealed that laparoscopic duodenoduodenostomy was performed in 40 out of 82 patients with DA, representing 48.8% of cases. The outcomes of this procedure were comparable to those of open surgery. Globally, a significant increase exists in the use of laparoscopic surgical procedures for treating children with DA. This is accompanied by the publication of numerous studies that compare the results of laparoscopic methods with those of open surgery in this population [
7-
10]. Martou and Saxena [
7] report that laparoscopic repair of DA shows equivalent complication rates compared to that of open repair with the added benefit of faster feeding establishment. Zhang et al. [
8] also show that laparoscopic surgery is a safe, feasible, and effective surgical procedure for neonatal congenital duodenal obstruction compared to open surgery. Finally, the mortality rate of patients with intestinal atresia decreased from 13.8% in the first national survey to 3.6% in the second and further declined to 1.3% in the third. Recent advancements in pediatric surgical techniques and the efforts of KAPS members are believed to have contributed to this decline in mortality rate.
Unfortunately, this study has limitations since there were no long-term follow-up data and the three national surveys used different case registration forms, which made it difficult to compare data between them effectively. However, these nationwide surveys provide substantial data on the current status, particular surgical treatments, and postoperative outcomes for patients with intestinal atresia in South Korea. These resources may serve as an invaluable source of guidance and information for pediatric surgeons seeking to expand their knowledge of intestinal atresia and its treatment options.
NOTES
-
Conflict of Interest
No potential conflict of interest relevant to this article was reported.
Fig. 1.Anatomical classification. Anatomical type of (A) duodenal atresia, (B) jejunal atresia, (C) ileal atresia, and (D) colonic atresia. Numbers in brackets indicates number of patients.
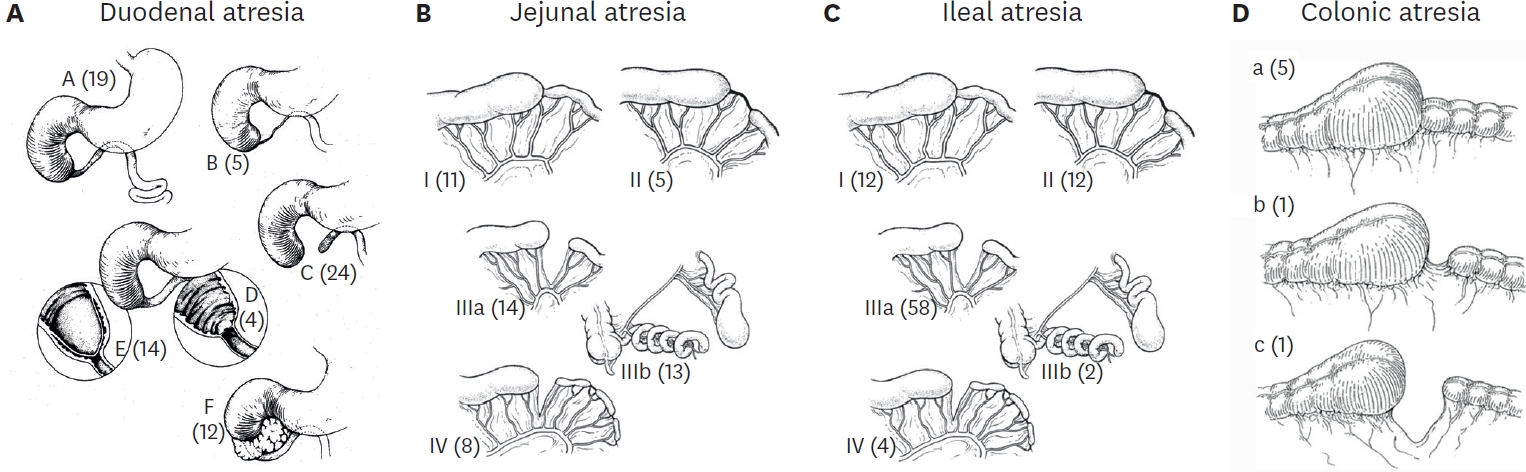
Table 1.Registered case numbers and incidence by surveys
Table 1.
|
National survey (yr) |
DA |
JA |
IA |
CA |
No. of cases/Birth No. |
Incidence |
|
1st (1994–1996) |
73 |
72 |
71 |
2 |
218/2,127,431 |
1/9,759 |
|
2nd (2007–2009) |
76 |
65 |
78 |
3 |
222/1,407,563 |
1/6,340 |
|
3rd (2021–2023) |
82 |
54 |
92 |
8 |
236/739,776 |
1/3,135 |
Table 2.Patient baseline characteristics
Table 2.
|
Characteristics |
Survey |
DA |
JA |
IA |
CA |
Total |
|
Male |
1st |
37 (50.7%) |
41 (56.9%) |
52 (71.2%) |
|
130 (59.6%) |
|
2nd |
35 (46.1%) |
29 (45.3%) |
53 (67.1%) |
|
117 (53.4%) |
|
3rd |
35 (42.7%) |
28 (51.9%) |
54 (58.7%) |
5 (62.5%) |
122 (51.7%) |
|
Preterm |
1st |
25 (35.2%) |
35 (48.6%) |
14 (19.2%) |
|
74 (34.3%) |
|
2nd |
29 (40.3%) |
42 (64.6%) |
23 (28.8%) |
|
94 (43.3%) |
|
3rd |
42 (51.2%) |
40 (74.1%) |
42 (45.7%) |
2 (25%) |
126 (53.4%) |
|
Birth weight <2,500g |
1st |
28 (39.4%) |
24 (33.3%) |
10 (13.7%) |
|
62 (28.7%) |
|
2nd |
29 (38.7%) |
28 (44.4%) |
13 (16.0%) |
|
70 (32.0%) |
|
3rd |
38 (46.4%) |
29 (53.7%) |
27 (29.3%) |
2 (25%) |
96 (40.7%) |
|
Prenatal diagnosis (+) |
1st |
Unknown |
Unknown |
Unknown |
|
92 (43.6%) |
|
2nd |
57 (75.0%) |
55 (84.6%) |
41 (50.6%) |
|
153 (68.9%) |
|
3rd |
70 (85.4%) |
46 (85.2%) |
46 (50%) |
1 (12.5%) |
163 (69.1%) |
|
Polyhydramnios |
1st |
33 (45.2%) |
23 (31.9%) |
7 (9.6%) |
|
63 (28.9%) |
|
2nd |
42 (55.3%) |
26 (40%) |
13 (16.0%) |
|
81 (36.5%) |
|
3rd |
49 (59.8%) |
25 (46.3%) |
18 (19.6%) |
|
92 (39.0%) |
Table 3.Clinical manifestation in the third national survey
Table 3.
|
Clinical manifestation |
DA (n=82) |
JA (n=54) |
IA (n=92) |
CA (n=8) |
|
Abdominal distention |
26 (31.7%) |
39 (72.2%) |
75 (81.5%) |
6 (75.0%) |
|
Bilious aspirate |
24 (29.3%) |
34 (63.0%) |
44 (47.8%) |
2 (25.0%) |
|
Feeding intolerance |
33 (40.2%) |
12 (22.2%) |
41 (44.6%) |
4 (50.0%) |
|
Vomiting |
21 (25.6%) |
9 (16.7%) |
34 (37.0%) |
5 (62.5%) |
|
Meconium passage |
26 (31.7%) |
5 (9.3%) |
21 (22.8%) |
4 (50.0%) |
|
Jaundice |
18 (22.0%) |
6 (11.1%) |
11 (12.0%) |
0 (0.0%) |
Table 4.Preoperative diagnostic methods in the third national survey
Table 4.
|
Preoperative diagnostic methods |
DA (n=82) |
JA (n=54) |
IA (n=92) |
CA (n=8) |
|
Abdominal X-ray |
81 (98.8%) |
54 (100.0%) |
88 (95.7%) |
7 (87.5%) |
|
Abdominal ultrasonography |
72 (87.8%) |
45 (83.3%) |
74 (80.4%) |
7 (87.5%) |
|
UGI series or SBS |
18 (21.9%) |
6 (11.1%) |
9 (9.8%) |
2 (25.0%) |
|
Colon study |
3 (3.7%) |
4 (7.4%) |
19 (20.7%) |
5 (62.5%) |
|
Abdominal CT |
2 (2.4%) |
1 (1.9%) |
4 (4.3%) |
0 (0.0%) |
Table 5.Associated anomalies in the third national survey
Table 5.
|
Associated anomalies |
DA (n=82) |
JA (n=54) |
IA (n=92) |
CA (n=8) |
|
Cardiovascular system |
43 (52.4%) |
21 (38.9%) |
40 (43.5%) |
4 (50.0%) |
|
Gastrointestinal system |
25 (30.5%) |
21 (38.9%) |
22 (23.9%) |
0 (0.0%) |
|
Central nerve system |
6 (7.3%) |
5 (9.3%) |
8 (8.7%) |
0 (0.0%) |
|
Genitourinary system |
5 (6.1%) |
7 (13.0%) |
5 (5.4%) |
0 (0.0%) |
|
Craniofacial & musculoskeletal system |
10 (12.2%) |
3 (5.6%) |
3 (3.3%) |
0 (0.0%) |
|
Chromosomal anomalies |
10 (12.2%) |
2 (3.7%) |
2 (2.2%) |
0 (0.0%) |
|
Others |
7 (8.5%) |
3 (5.6%) |
2 (2.2%) |
0 (0.0%) |
Table 6.Associated gastrointestinal anomalies in the third national survey
Table 6.
|
Gastrointestinal anomalies |
DA (n=82) |
JA (n=54) |
IA (n=92) |
CA (n=8) |
|
Malrotation |
15 (18.3%) |
8 (14.8%) |
5 (5.4%) |
1 (12.5%) |
|
Meconium peritonitis |
0 (0.0%) |
12 (22.2%) |
13 (14.1%) |
0 (0.0%) |
|
Esophageal atresia |
4 (4.9%) |
0 (0.0%) |
1 (1.1%) |
0 (0.0%) |
|
Volvulus |
0 (0.0%) |
1 (1.9%) |
4 (4.3%) |
0 (0.0%) |
|
Omphalomesenteric duct remnant |
0 (0.0%) |
0 (0.0%) |
2 (2.2%) |
1 (12.5%) |
|
Hirschsprung’s disease |
1 (1.2%) |
1 (1.9%) |
1 (1.1%) |
0 (0.0%) |
|
Anorectal malformation |
2 (2.4%) |
0 (0.0%) |
0 (0.0%) |
0 (0.0%) |
|
Situs inversus |
2 (2.4%) |
0 (0.0%) |
0 (0.0%) |
0 (0.0%) |
|
Intussusception |
0 (0.0%) |
0 (0.0%) |
2 (2.2%) |
0 (0.0%) |
|
Hepatic hemangioma |
0 (0.0%) |
1 (1.9%) |
1 (1.1%) |
0 (0.0%) |
|
Gastroschisis |
0 (0.0%) |
0 (0.0%) |
1 (1.1%) |
0 (0.0%) |
|
Polysplenia |
1 (1.2%) |
0 (0.0%) |
0 (0.0%) |
0 (0.0%) |
Table 7.Operative treatment of duodenal atresia based on the anatomical type in the third national survey
Table 7.
|
Operation |
A |
B |
C |
D |
E |
F |
Others |
Total |
|
Duodenoduodenostomy |
16 (10) |
5 (2) |
23 (11) |
3 (1) |
8 (5) |
11 (8) |
4 |
70 (37) |
|
Duodenojejunostomy |
2 |
0 |
1 |
0 |
1 |
0 |
0 |
4 |
|
Duodenoduodenostomy with WE |
0 |
0 |
0 |
0 |
3 (2) |
0 |
0 |
3 (2) |
|
Gastrojejunostomy |
1 |
0 |
0 |
0 |
0 |
1 |
0 |
2 |
|
WE with duodenoplasty |
0 |
0 |
0 |
1 (1) |
0 |
0 |
0 |
1 (1) |
|
WE |
0 |
0 |
0 |
0 |
1 |
0 |
0 |
1 |
|
Segmental resection of duodenum |
0 |
0 |
0 |
0 |
1 |
0 |
0 |
1 |
|
Total |
19 (10) |
5 (2) |
24 (11) |
4 (2) |
14 (7) |
12 (8) |
4 |
82 (40) |
Table 8.Operative treatment of jejunal atresia based on the anatomical type in the third national survey
Table 8.
|
Operation |
I |
II |
IIIa |
IIIb |
IV |
Others |
Total |
|
R & A |
10 (2) |
3 |
11 (1) |
12 |
8 |
3 |
47 (3) |
|
Stoma formation |
0 |
1 |
2 |
1 |
0 |
0 |
4 |
|
R & A with stoma |
0 |
0 |
1 |
0 |
0 |
0 |
1 |
|
R with stoma |
0 |
1 |
0 |
0 |
0 |
0 |
1 |
|
Web excision |
1 |
0 |
0 |
0 |
0 |
0 |
1 |
|
Total |
11 |
5 |
14 |
13 |
8 |
3 |
54 |
Table 9.Operative treatment of ileal atresia based on the anatomical type in the third national survey
Table 9.
|
Operation |
I |
II |
IIIa |
IIIb |
IV |
Others |
Total |
|
R & A |
9 |
11 (1) |
46 |
2 |
3 |
3 |
74 (1) |
|
R with stoma formation |
1 |
1 |
8 |
0 |
0 |
0 |
10 |
|
Stoma formation |
1 |
0 |
4 |
0 |
1 |
0 |
6 |
|
Anastomosis |
1 |
0 |
0 |
0 |
0 |
0 |
1 |
|
Unknown |
0 |
0 |
0 |
0 |
0 |
1 |
1 |
|
Total |
12 |
12 |
58 |
2 |
4 |
6 |
92 |
Table 10.Operative treatment of colonic atresia based on the anatomical type in the third national survey
Table 10.
|
Operation |
I |
II |
III |
Others |
Total |
|
R & A |
3 |
1 |
1 |
0 |
5 |
|
R & A with stoma |
0 |
0 |
0 |
1 |
1 |
|
Web plasty |
1 |
0 |
0 |
0 |
1 |
|
Stoma formation |
1 |
0 |
0 |
0 |
1 |
|
Total |
5 |
1 |
1 |
1 |
8 |
Table 11.Plication or tapering enteroplasty in the second and third national surveys
Table 11.
|
Survey |
DA |
JA |
IA |
Total |
|
2nd |
5/76 (6.6%) |
18/65 (27.7%) |
7/80 (8.8%) |
30/221 (13.6%) |
|
3rd |
3/82 (3.7%) |
11/54 (20.4%) |
6/92 (6.5%) |
20/228 (8.8%) |
Table 12.Postoperative complications in the third national survey
Table 12.
|
Postoperative complications |
DA (n=82) |
JA (n=54) |
IA (n=92) |
CA (n=8) |
|
Early complications |
|
|
|
|
|
Intestinal obstruction |
3 |
4 |
3 |
0 |
|
Wound infection |
2 |
0 |
6 |
0 |
|
Stenosis |
0 |
5 |
1 |
1 |
|
Leakage |
1 |
1 |
1 |
0 |
|
Sepsis |
1 |
0 |
1 |
0 |
|
CVC related infection |
0 |
0 |
1 |
0 |
|
Acute renal failure |
0 |
0 |
1 |
0 |
|
Late complications |
|
|
|
|
|
Intestinal obstruction |
0 |
6 |
9 |
0 |
|
TPN-related cholestasis |
0 |
2 |
4 |
0 |
|
Short bowel syndrome |
0 |
2 |
2 |
0 |
|
NEC |
0 |
0 |
2 |
0 |
|
Brain hemorrhage |
0 |
1 |
0 |
0 |
|
Sepsis |
0 |
1 |
0 |
0 |
|
Incisional hernia |
0 |
0 |
1 |
0 |
|
UGI bleeding |
0 |
0 |
1 |
0 |
Table 13.Time to full feeding and length of hospital stays
Table 13.
|
Variables |
Survey |
DA |
JA |
IA |
p-value |
|
Time to full feeding (days) |
2nd |
14.9±7.2 |
23.7±17.5 |
17.1±16.3 |
<0.05 |
|
3rd |
13.0 (9.0–17.0) |
23.5 (15.0–43.5) |
13.0 (10.0–23.0) |
0.001 |
|
Length of hospital stays (days) |
3rd |
26.0 (18.0–44.0) |
40.0 (32.0–79.0) |
27.0 (17.0–47.0) |
0.001 |
Table 14.Mortality rate determined via surveys
Table 14.
|
Survey |
DA |
JA & IA |
Total |
|
1st |
10/73 (13.7%) |
20/145 (13.8%) |
30/218 (13.8%) |
|
2nd |
3/76 (3.9%) |
5/146 (3.4%) |
8/222 (3.6%) |
|
3rd |
1/82 (1.2%) |
2/146 (1.4%) |
3/236 (1.3%) |
REFERENCES
- 1. Kim I, Kim S, Kim S, Kim W, Kim J, Kim J, et al. Intestinal atresia: a survey by the Korean Association of Pediatric Surgeons. J Korean Assoc Pediatr Surg 1999;5:75-81.
- 2. Kim SC, Kim DY, Kim SY, Kim IK, Kim IS, Kim JE, et al. Intestinal atresia: the second national survey. J Korean Assoc Pediatr Surg 2010;16:1-10.
- 3. Bethell GS, Long AM, Knight M, Hall NJ; BAPS-CASS. Congenital duodenal obstruction in the UK: a population-based study. Arch Dis Child Fetal Neonatal Ed 2020;105:178-83.
- 4. Walker K, Badawi N, Hamid CH, Vora A, Halliday R, Taylor C, et al. A population-based study of the outcome after small bowel atresia/stenosis in New South Wales and the Australian Capital Territory, Australia, 1992-2003. J Pediatr Surg 2008;43:484-8.
- 5. Schmedding A, Hutter M, Gfroerer S, Rolle U. Jejunoileal atresia: a national cohort study. Front Pediatr 2021;9:665022.
- 6. Best KE, Tennant PW, Addor MC, Bianchi F, Boyd P, Calzolari E, et al. Epidemiology of small intestinal atresia in Europe: a register-based study. Arch Dis Child Fetal Neonatal Ed 2012;97:F353-8.
- 7. Martou L, Saxena AK. Laparoscopic repair of duodenal atresia: systematic review and meta-analysis after consistent implementation of the technique in the past decade. Surg Endosc 2024;38:3296-309.
- 8. Zhang J, Xu X, Wang X, Zhao L, Lv Y, Chen K. Laparoscopic versus open repair of congenital duodenal obstruction: a systematic review and meta-analysis. Pediatr Surg Int 2022;38:1507-15.
- 9. Weller JH, Engwall-Gill AJ, Westermann CR, Patel PP, Kunisaki SM, Rhee DS. Laparoscopic versus open surgical repair of duodenal atresia: a NSQIP-Pediatric analysis. J Surg Res 2022;279:803-8.
- 10. Son TN, Kien HH. Laparoscopic versus open surgery in management of congenital duodenal obstruction in neonates: a single-center experience with 112 cases. J Pediatr Surg 2017;52:1949-51.
 , Dayoung Ko2, Eun-jung Koo2, Hyunhee Kwon2, Ki Hoon Kim2, Dae Yeon Kim2, Seong Chul Kim2, Soo-Hong Kim2, Wontae Kim2, HaeYoung Kim2, Hyun-Young Kim2, So Hyun Nam2, Jung-Man Namgoong2, Junbeom Park2, Taejin Park2, Min-Jung Bang2, Jeong-Meen Seo2, Ji-Young Sul2, Joonhyuk Son2, Joohyun Sim2, Soo Min Ahn2, Hee-Beom Yang2, Jung-Tak Oh2, Chaeyoun Oh2, Joong Kee Youn2, Sanghoon Lee2, Ju Yeon Lee2, Kyong Ihn2, Hye Kyung Chang2, Yeon Jun Jeong2, Eunyoung Jung2, Jae Hee Chung2, Min Jeong Cho2, Yun-Mee Choe2, Seok Joo Han2, In Geol Ho2, Jeong Hong2
, Dayoung Ko2, Eun-jung Koo2, Hyunhee Kwon2, Ki Hoon Kim2, Dae Yeon Kim2, Seong Chul Kim2, Soo-Hong Kim2, Wontae Kim2, HaeYoung Kim2, Hyun-Young Kim2, So Hyun Nam2, Jung-Man Namgoong2, Junbeom Park2, Taejin Park2, Min-Jung Bang2, Jeong-Meen Seo2, Ji-Young Sul2, Joonhyuk Son2, Joohyun Sim2, Soo Min Ahn2, Hee-Beom Yang2, Jung-Tak Oh2, Chaeyoun Oh2, Joong Kee Youn2, Sanghoon Lee2, Ju Yeon Lee2, Kyong Ihn2, Hye Kyung Chang2, Yeon Jun Jeong2, Eunyoung Jung2, Jae Hee Chung2, Min Jeong Cho2, Yun-Mee Choe2, Seok Joo Han2, In Geol Ho2, Jeong Hong2