ABSTRACT
-
Purpose
To report a nationwide survey on neuroblastoma conducted by the Korean Association of Pediatric Surgeons (KAPS) in 2020.
-
Methods
The clinical data of pediatric patients diagnosed with and treated for neuroblastoma from 2005 to 2019 in 19 hospitals of KAPS members were collected. Survival and prognostic factor analyses were performed using the log rank test and Cox proportional hazard analysis. A p-value <0.05 was considered significant.
-
Results
A total of 669 patients with neuroblastoma were registered for the study. The results were presented and discussed at the 36th annual meeting of the KAPS, which was held in Seoul on August 21, 2020.
-
Conclusion
This study provides information on patient demographics, prognostic outcomes, and comprehensive treatment outcomes for neuroblastoma. The study is expected to be an important reference for improving pediatric surgeons’ understanding and treatment of neuroblastoma.
-
Keywords: Neuroblastoma; Pediatrics; Surveys
INTRODUCTION
According to the annual report of cancer statistics, neuroblastoma is the most common extracranial solid tumor of childhood in Korea, with a crude incident rate of approximately 10.0 per million [
1-
5]. According to available statistics, only 340 patients were diagnosed with neuroblastoma and ganglioneuroblastoma between 2016 and 2020 in Korea, accounting for 6.9% of all pediatric patients with cancer [
1-
5]. Primary neuroblastomas arise from cells of the sympathetic nervous system in the adrenal medulla or along the sympathetic chain. Neuroblastomas have remarkably heterogeneous clinical characteristics, which may spontaneously resolve but are often lethal [
6]. Tumors originating in the adrenal gland can manifest as abdominal distension, while tumors of the sympathetic nervous system present various symptoms depending on the site of origin. Extensive liver disease can be associated with hepatic dysfunction and coagulopathy. Patients with bone marrow involvement often present with fever, malaise, pain, and/or cytopenia. Targeted small molecules, radiopharmaceuticals, and immunotherapies can be considered for advanced treatments [
6]. Its rarity and heterogeneity have made it difficult for surgeons to understand this disease and choose optimal treatment methods. Hence, the 2020 annual nationwide survey of the Korean Association of Pediatric Surgeons (KAPS) on neuroblastoma will be helpful. The results were first presented and discussed at the annual meeting of the KAPS in Seoul on August 21, 2020.
METHODS
The clinical data of pediatric patients diagnosed with and treated for neuroblastoma from 2005 to 2019 in 19 hospitals of KAPS members were collected retrospectively. A Google Form was used for patient registration and data collection (
https://forms.gle/2moYzp2hK5MbajEA6). This study was approved by the Institutional Review Board (IRB) of Seoul National University Hospital (IRB No.: 2310-064-1476). All the data were analyzed using the IBM SPSS version 22 statistical software package (IBM Co., Armonk, NY, USA). Survival and prognostic factor analyses were performed using the log rank test and Cox proportional hazard analysis. A p-value <0.05 was considered statistically significant.
RESULTS
1. Demographics
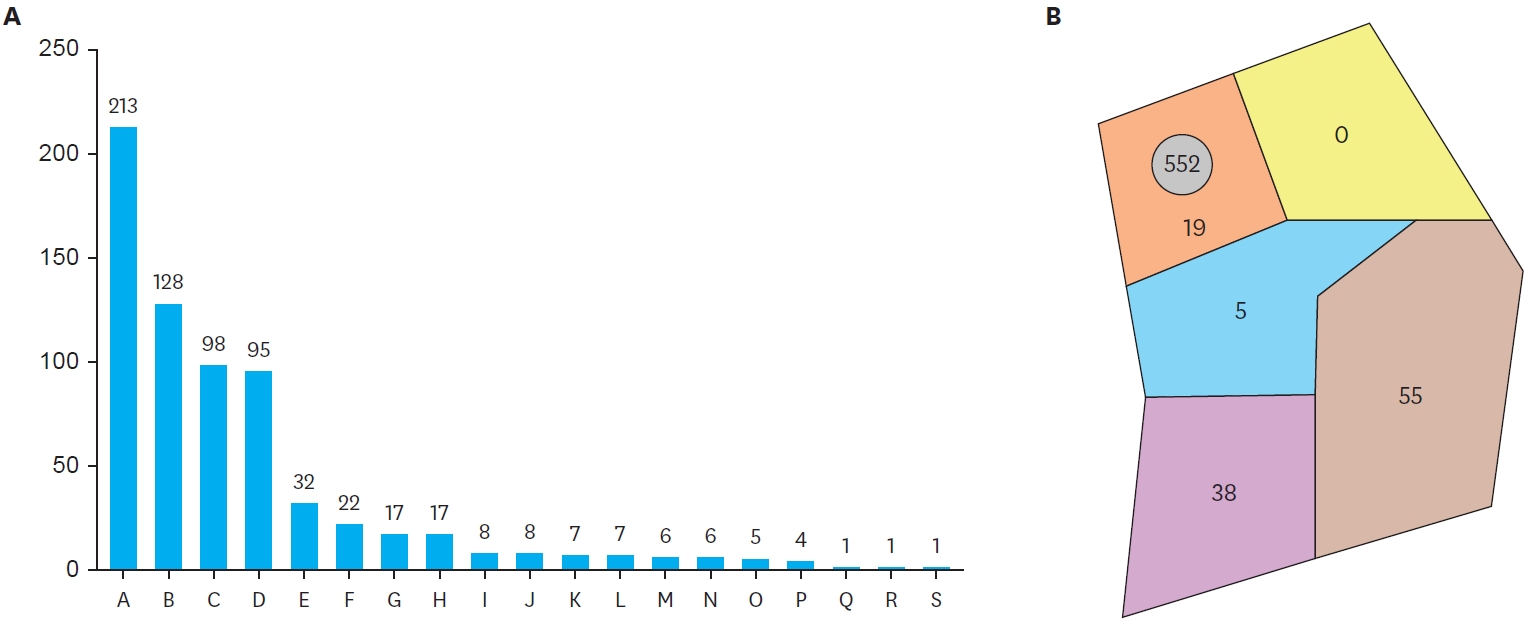
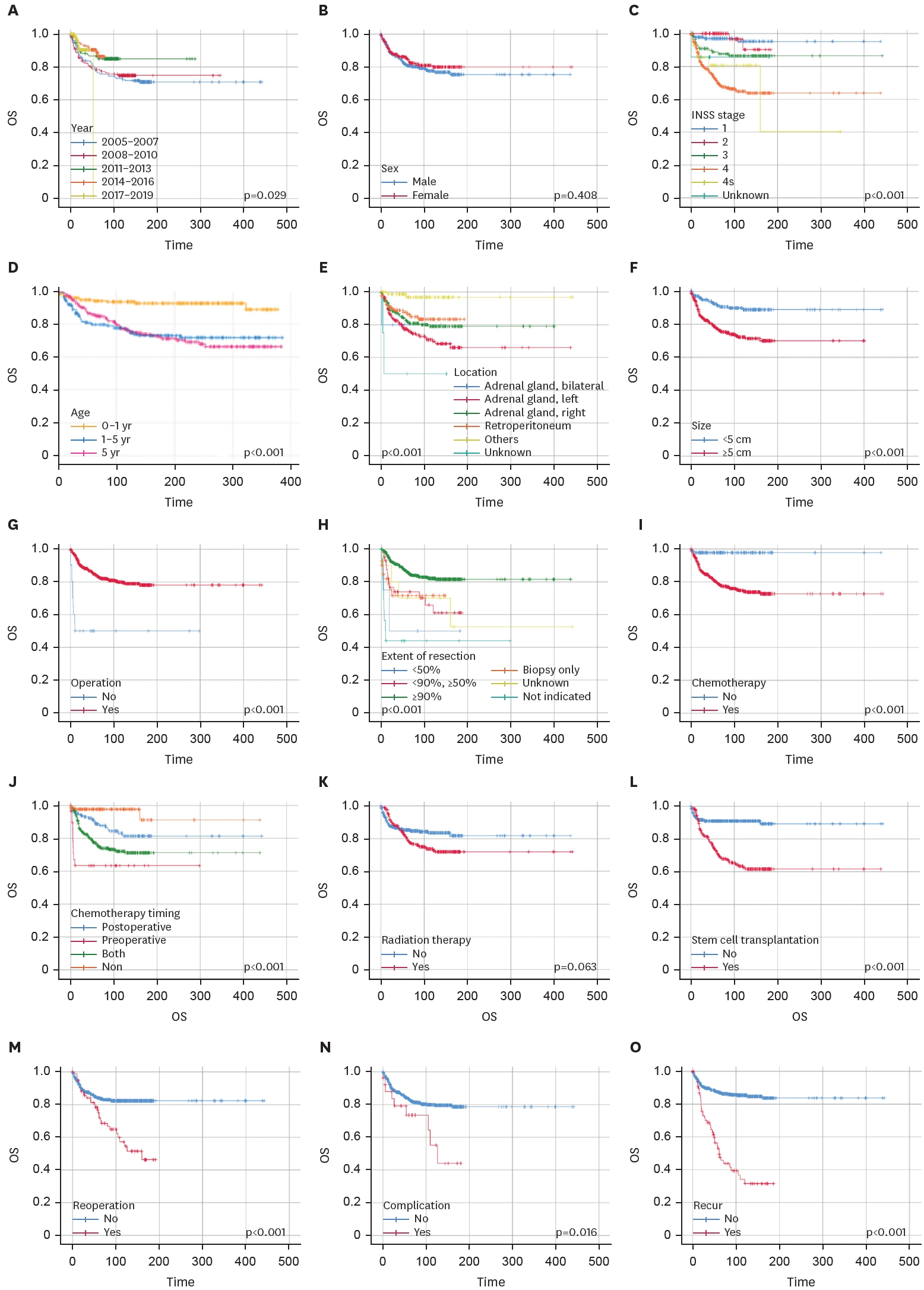
A total of 669 patients were registered for this survey. The registration by hospital and region is shown in
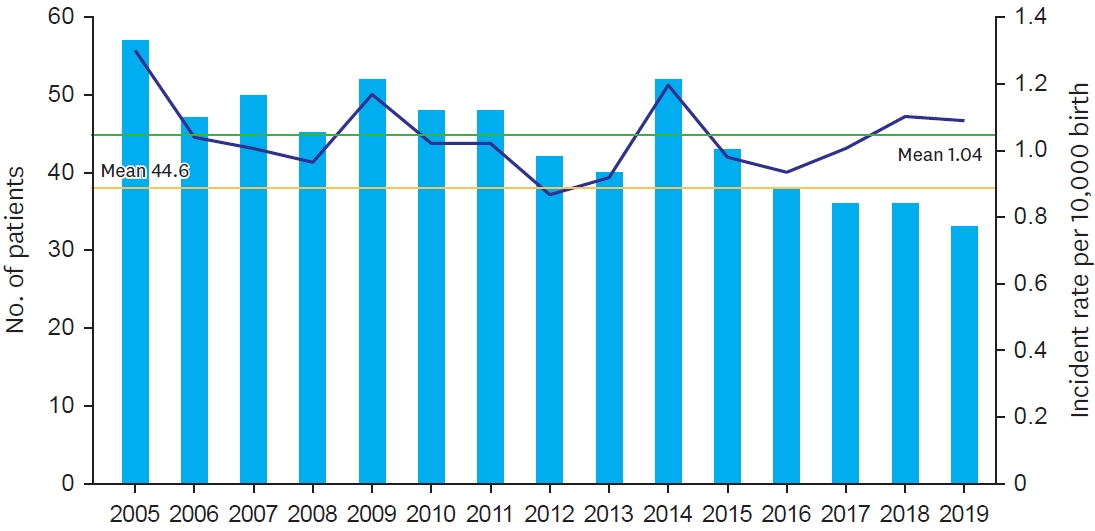
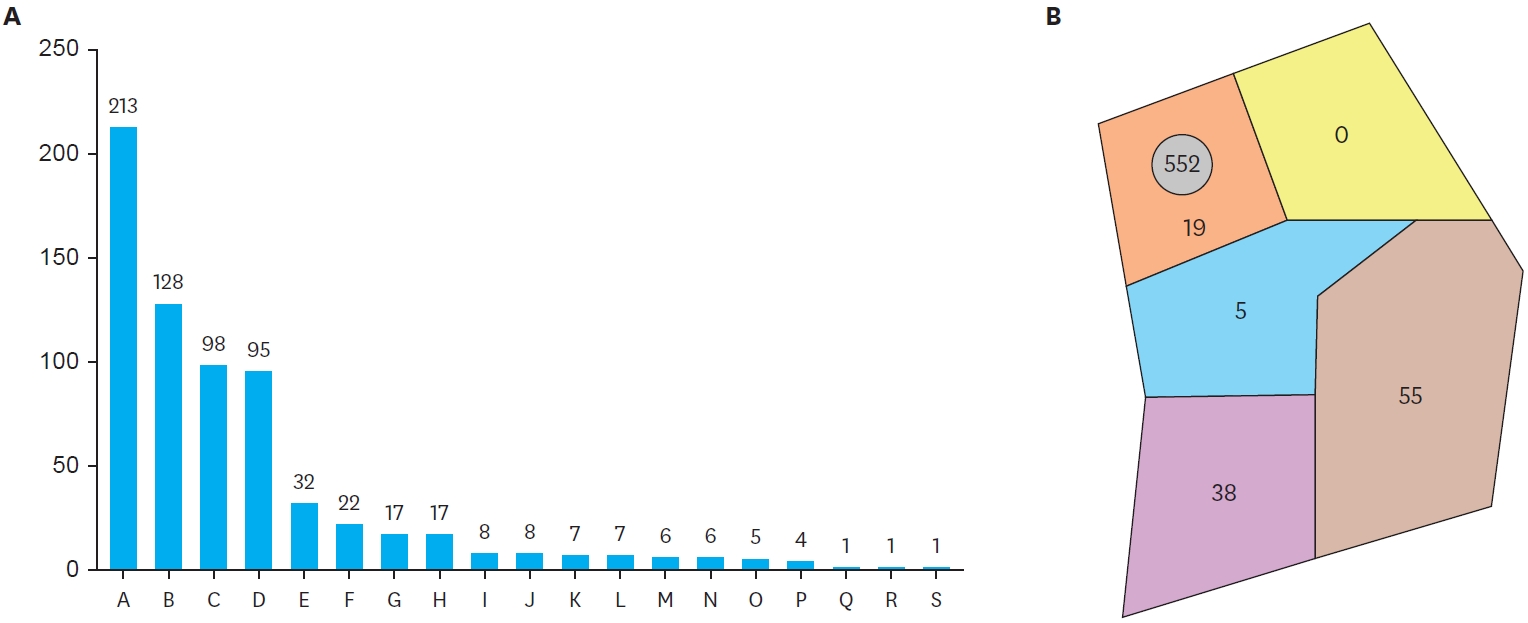
Fig. 1. The mean number of yearly registrations was 44.6, and the incident rate per 10,000 births was 1.04 (
Fig. 2). There were slightly more males than females (M:F=1.36:1). The median age at diagnosis was 2.1 years. Patients who were diagnosed under one year of age 32.4%. The interquartile range of age at diagnosis was 0.6–3.9 years, which means 75% of patients were diagnosed with neuroblastoma at less than 5 years of age. Moreover, only 15.5% of patients were diagnosed with neuroblastoma after 5 years of age. The mean size at diagnosis was 6.6 cm, and the size reduced to 5.1 cm during surgery. The adrenal gland was the most common site (68.4%); other retroperitoneal sites apart from the adrenal gland were the second most common in this study. Laterality in the location of tumors was not observed for tumors of adrenal origin in this study (left: 34.1% vs. right: 33.6%). Bilateral tumors were extremely rare (0.7%). Histologic investigation revealed that neuroblastoma was more common than ganglioneuroblastoma (81.3%, 544:125). Biopsy was performed in 86.1% of all patients. Stage 4 neuroblastoma, according to the International Neuroblastoma Staging System (INSS), was the most common stage (47.1%). Stage 1 was the second most common in this study (n=141, 21.1%). The median follow-up period was 69.4 months. Detailed demographic data are presented in
Table 1.
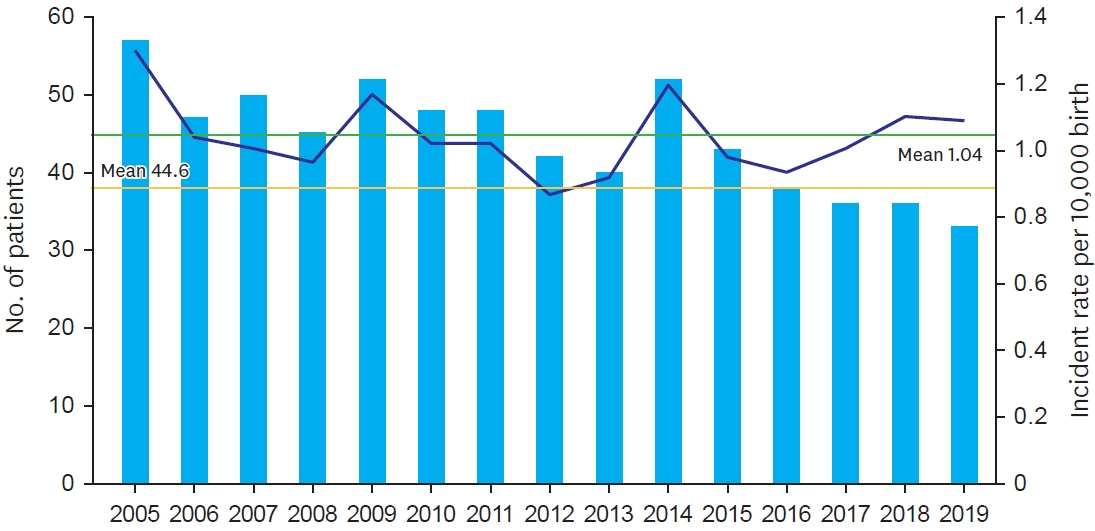
Nearly all patients underwent operation for neuroblastoma (n=648, 96.9%). Chemotherapy was performed for 79.5% (n=532) of all patients. Stem cell transplantation (SCT) and radiation therapy (RT) was performed for 42.2% (n=282) and 40.2% (n=269) of patients, respectively (
Fig. 3).
Open surgery was performed for 82.4% of the 648 patients who underwent surgery (
Table 2). The proportion of patients who underwent laparoscopy and conversion to open surgery were 13.3% and 4.3%, respectively. Near total excision was achieved in 85.6% of patients, and only 4 patients failed to achieve an extent of operation greater than 50%. Combined resection of the tumor and other organs, such as the kidney, liver, and blood vessels, was required in 11.1% of all patients that underwent surgery. The kidney was the most affected organ (45.9% of all combined resection cases). Only 3.9% of the patients who underwent operation experienced complications after surgery. The most common complication was ileus, accounting for nearly one-third of patients with complications. Wound complications, bleeding, and neurologic deficits, in that order, were the other common complications. Reoperation was needed in 12.2% due to a residual mass or recurrence (n=40, 6.2%), metastasis (n=31, 4.8%), or complications (n=11, 1.7%).
Among those administered chemotherapy, 5.6% were administered only neoadjuvant chemotherapy (
Table 1). Further, administration of both neoadjuvant and adjuvant chemotherapy was most performed for these patients (n=353, 66.4%); 28.0% of these patients were administered only adjuvant chemotherapy. Only one regimen was required in 60.3% of these patients, and more than 4 regimens were used in 6.8% of all patients administered chemotherapy.
Of the 669 patients, 79 (11.8%) experienced recurrence. During the median 69.4-month follow-up period, 120 patients (17.9%) died. Out of them, 101 deaths were tumor-related, and 16 were not directly related to the tumor (
Table 3).
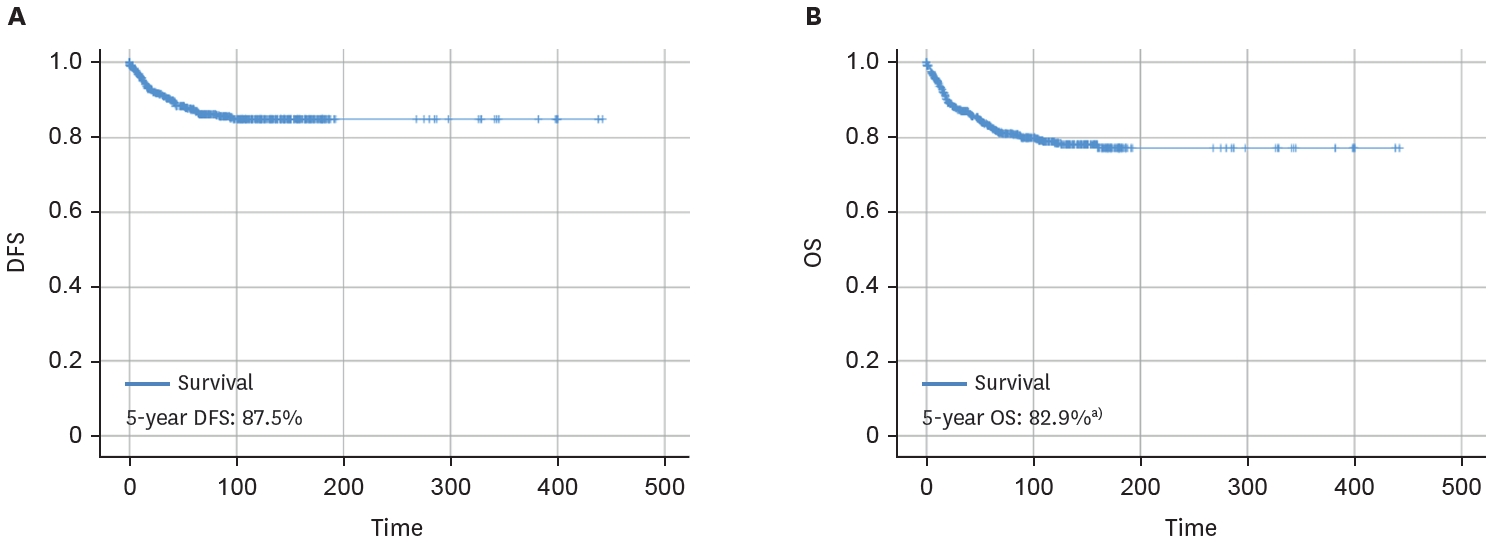
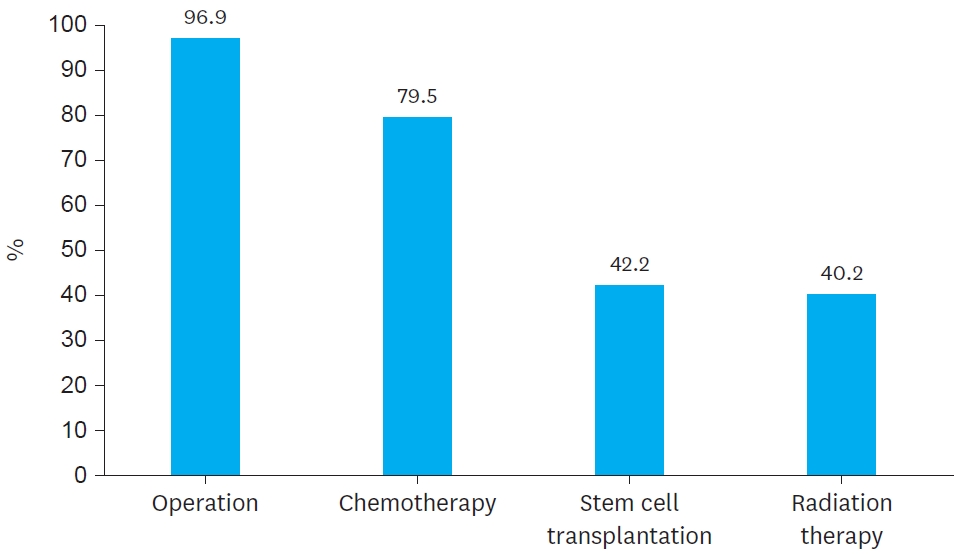
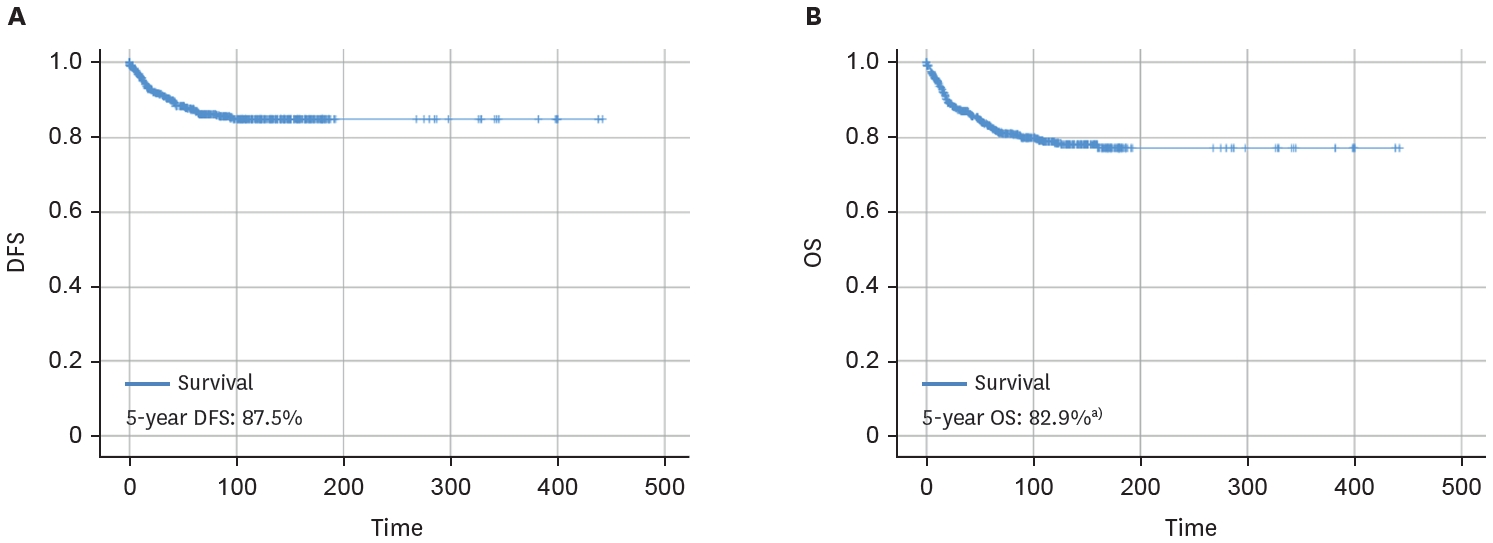
The disease-free survival (DFS) and overall survival (OS) rates at 5 years were 87.5% and 82.9%, respectively (
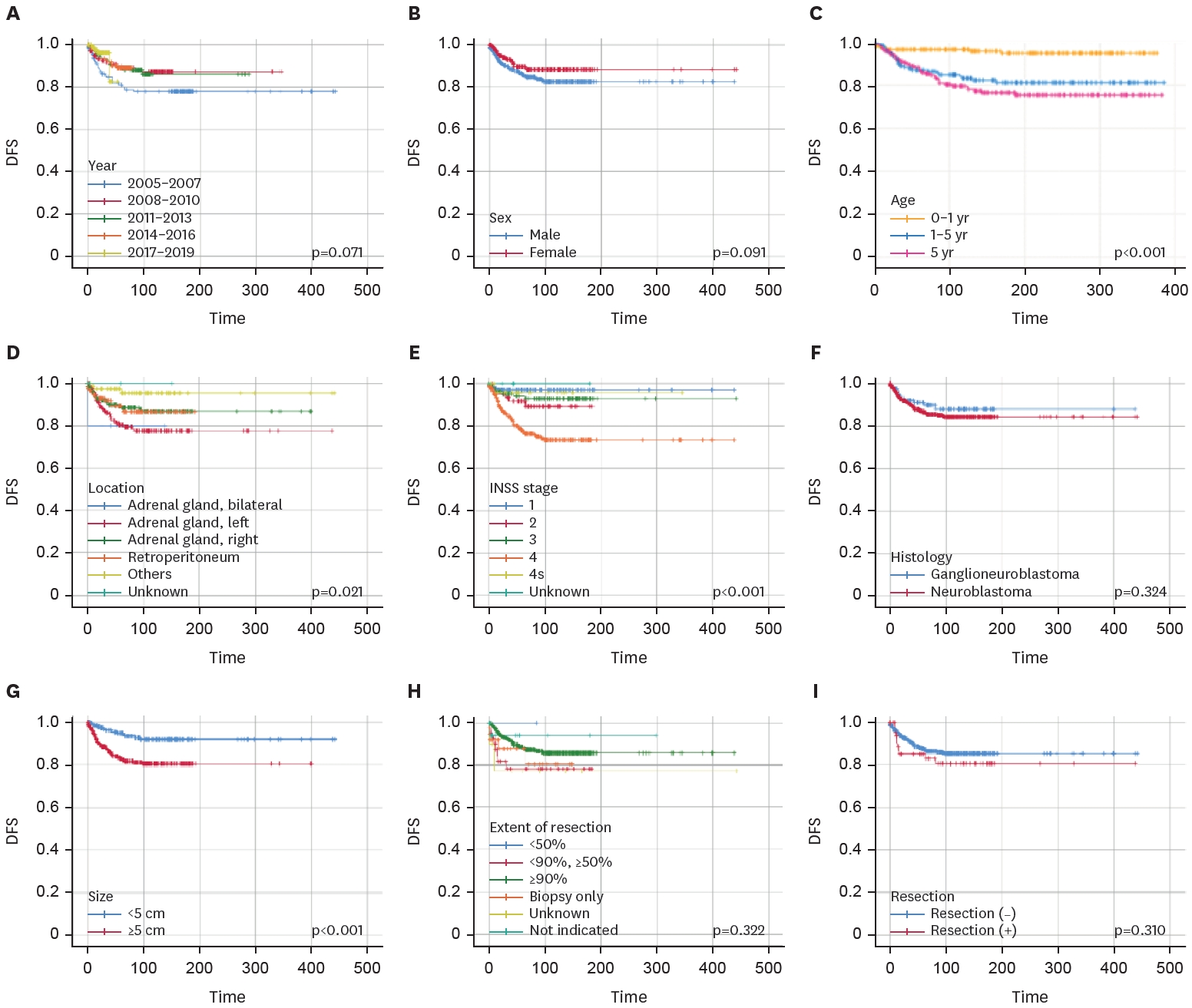
Fig. 4). Significant factors affecting DFS were age at diagnosis, tumor location, INSS stage, and size at diagnosis. Patients in the older age group and those with adrenal gland tumor, stage 4 tumor, and tumor size >5 cm had poor DFS (
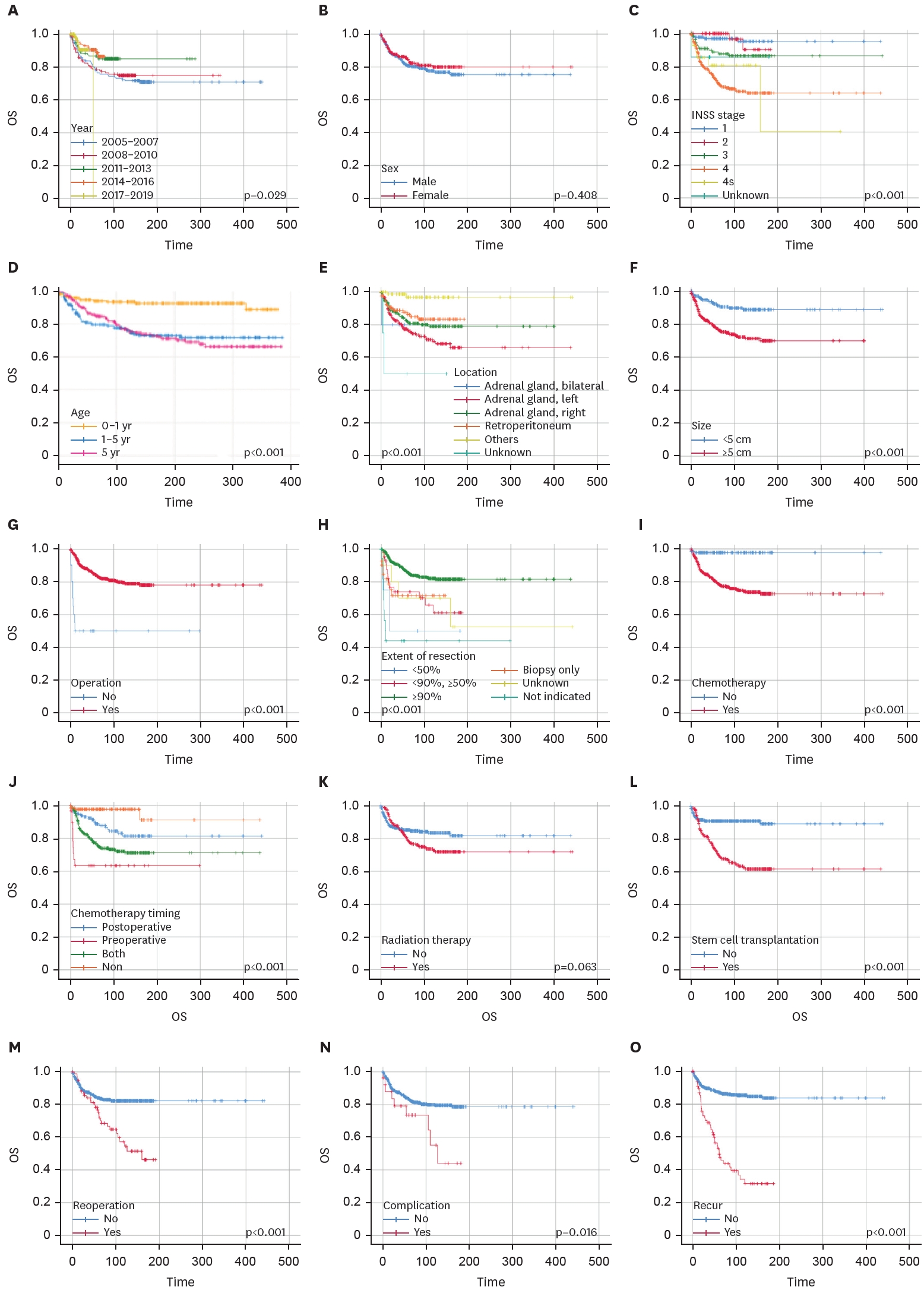
Fig. 5). The most significant factors affecting DFS were age at diagnosis, INSS stage, and size at diagnosis (p<0.001). Significant factors affecting OS were calendar year at diagnosis, age at diagnosis, INSS stage, location, size at diagnosis, whether surgery was performed, extent of operation, whether chemotherapy was administered, chemotherapy timing, SCT, reoperation, complication, and recurrence (
Fig. 6). Diagnosis before 2011, age at diagnosis greater than one-year, abdominal location, stage 4 tumor, and size >5 cm were associated with poor OS. Patients who did not undergo surgery, those with an extent of operation less than 90%, and those who underwent combined resection also had poor OS. Patients who underwent chemotherapy, SCT, and RT survived less than those who did not undergo these therapies. Reoperation, complications, and recurrence also worsened the OS.
A multivariable Cox hazard analysis was performed to identify the independent factors affecting OS (
Table 4). Size at diagnosis larger than 5 cm was associated with a 2.013 times higher risk than size at diagnosis less than 5 cm (95% confidence interval [CI], 1.205–3.363). Recurrence was the independent prognostic factor (hazard ratio [HR], 3.237; 95% CI, 2.097–4.996). Greater than or equal to 90% resection was a protective factor (HR, 0.133; 95% CI, 0.029–0.603).
DISCUSSION
This survey on neuroblastoma that was conducted in 2020 was the first nationwide survey of a pediatric malignant tumor among all surveys performed in the last three decades. Annually, only 40 cases occurred in Korea, without a definite yearly trend. Neuroblastoma occurred slightly more in males than in females. The diagnosis was made at an early age (median 2.1 years old). The adrenal gland was the most common site of the tumor. Nearly all patients underwent operation for neuroblastoma. Chemotherapy was performed for 79.5% of all patients. More than 80% of patients with neuroblastoma survived for more than 5 years. The size, extent of operation, and recurrence were the most important factors affecting OS.
The number of hospitals from which cases were registered was 19, which is similar to that in the 2019 survey (n=18). However, the proportion of top-4 hospitals from which cases were registered in this survey was higher than that of the 2019 survey (79.8% vs. 69.5%). Considering the location of these four hospitals, this trend may reflect the concentration of patients with severe diseases around the capital. According to statistics in Korea [
1-
5], approximately 68 patients are diagnosed with neuroblastoma and ganglioneuroblastoma in Korea annually, which means that our cohort was not a perfect reflection of the national patients’ characteristics. Approximately 40 patients were enrolled in our cohort annually.
The difference of age at diagnosis between our findings and data from other countries was not significant. According to the Neuroblastoma Treatment (PDQ
®)-Health Professional Version data, approximately 37% of patients are diagnosed as infants, and 90% are younger than 5 years at diagnosis, with a median age at diagnosis of 17 months [
7-
9]. The median age at diagnosis in our study was 2.1 years, which is similar to the PDQ
® data. A study performed in another Eastern country confirms our finding that neuroblastoma is diagnosed at a very early age [
10]. Ma et al. [
10] reported a case series of neuroblastoma in Eastern China, and 17.8% of the patients were diagnosed later than 5 years of age, which is similar to our finding of 15.5%. Those with stage 4 disease accounted for the highest proportion of patients in our study (47.1%), which is consistent with the findings of the study performed in the other Eastern country (52.0%) [
10]. This characteristic can also be observed in Western countries, as indicated by the findings of the COG ANBL00B1 Analytic Cohort study (44.6%) [
11]. There is already systemic dissemination of the disease in nearly half of patients with neuroblastoma at the time of diagnosis, regardless of their country of origin. Well-known prognostic factors for neuroblastoma include age, INSS stage, and time to first relapse [
9]. In our study, survival varied by age and stage of disease; however, they were not independent prognostic factors after multivariable analysis. Tumor size greater than 5 cm was the independent prognostic factor in our study. Although there are still debates about whether tumor size is a prognostic factor due to other considerations such as location and vessel invasion, one study reported that tumor size may be an important factor [
12]. Wang et al. [
12] reported that tumor size can be an important prognostic factor for neuroblastoma and suggested a cutoff value of 4 cm for predicting prognosis. Tumor size greater than 4 cm was the independent poor prognostic factor, irrespective of age or primary site. However, this prediction was only applicable to patients with unfavorable prognosis, such as those with advanced disease or undifferentiated grade tumor at diagnosis, but not to those with regional disease, local disease, or undifferentiated tumors. The extent of the operation is another debatable prognostic factor. In our study, an extent of operation greater than or equal to 90% was an independent prognostic factor. However, one study reported contradictory results regarding this subject [
13]. Of the four studies, two showed better survival in the complete resection group than in the partial resection group, whereas the other two could not confirm a difference in survival between the two groups. Because stage 4 neuroblastoma is already systemic and not a local disease, it has been suggested that local control by complete resection may not be necessary. In addition, the survival of patients with high-risk neuroblastoma is more strongly related to metastases than to the extent of resection. This inconsistency can partly be explained by the lack of a universal staging system and the diversity of terminology used before the INSS was developed. Heterogeneity of treatment methods other than surgery may be another factor accounting for the inconsistent results with regards to the extent of operation. Some studies may have performed early surgery rather than prolonged chemotherapy or radiotherapy, while others did not. However, recent studies showed a better prognosis in patients with high-risk neuroblastoma when complete resection was achieved [
14,
15]. Although aggressive local control can lead to complications, the incidence of complications is not statistically different from that when this is not done, as demonstrated in previous studies. It is generally appropriate to achieve complete resection whenever possible.
The reason why age at diagnosis and INSS stage are not independent prognostic factors should be further analyzed. This multicenter national cohort analysis suggests that age at diagnosis and disease stage reflect some tumor characteristics that truly affect survival but are not important independent prognostic factors.
There are many limitations to this study. Only 55% of all neuroblastoma patients in Korea were enrolled, according to the national statistics. Several important factors were omitted, such as symptoms, method of biopsy, serum tumor markers, genomic markers, reoperation timing, advanced treatment method other than operation, chemotherapy, SCT, and RT. Data quality should have been examined more thoroughly to resolve incompatibilities between factors. A statistical analysis that evaluates more than survival should be performed in a future study. Despite these limitations, we believe that this study will be an important reference for improving pediatric surgeons’ understanding and treatment of neuroblastoma.
Scientific Presentation
The results of this study were presented and discussed at the 36th annual meeting of the Korean Association of Pediatric Surgeons that held in Seoul on August 21, 2020.
NOTES
-
Conflict of Interest
No potential conflict of interest relevant to this article was reported.
-
Author Contributions
Conceptualization: K.H.Y.; Data curation: Y.H.B., A.S.M., C.M.J., C.Y.H., C.S.J.N., C.Y.M., C.J.H., H.S.J., H.I.G., H.J., I.K., J.Y.J., J.E., K.D.Y., K.H.Y., K.K.H., K.S.C., K.S.H., K.E.J., K.H.H., K.Y.J., L.N.H., L.J.Y., L.S., N.J.M., O.C., O.J.T., P.J.Y., P.J., S.J.M., S.J.H., S.H.B., S.J., S.J., Y.J.K., K.H.Y.; Formal analysis: Y.H.B.; Investigation: K.H.Y., Y.H.B.; Methodology: A.S.M., C.M.J., C.Y.H., C.S.J.N., C.Y.M., C.J.H., H.S.J., H.I.G., H.J., I.K., J.Y.J., J.E., K.D.Y.; Project administration: K.H.Y.; Resources: K.H.Y., K.K.H., K.S.C., K.S.H., K.E.J., K.H.H., K.Y.J., L.N.H., L.J.Y., L.S., N.J.M., O.C., O.J.T., P.J.Y., P.J., S.J.M., S.J.H., S.H.B., S.J., S.J., Y.J.K.; Software: Y.H.B.; Supervision: K.H.Y.; Visualization: Y.H.B.; Writing - original draft: Y.H.B.; Writing - review & editing: Y.H.B., A.S.M., C.M.J., C.Y.H., C.S.J.N., C.Y.M., C.J.H., H.S.J., H.I.G., H.J., I.K., J.Y.J., J.E., K.D.Y., K.H.Y., K.K.H., K.S.C., K.S.H., K.E.J., K.H.H., K.Y.J., L.N.H., L.J.Y., L.S., N.J.M., O.C., O.J.T., P.J.Y., P.J., S.J.M., S.J.H., S.H.B., S.J., S.J., Y.J.K., K.H.Y.
Fig. 1.
Hospital and regional distribution.
Hospital (A) and regional (B) distribution of patients in this survey.
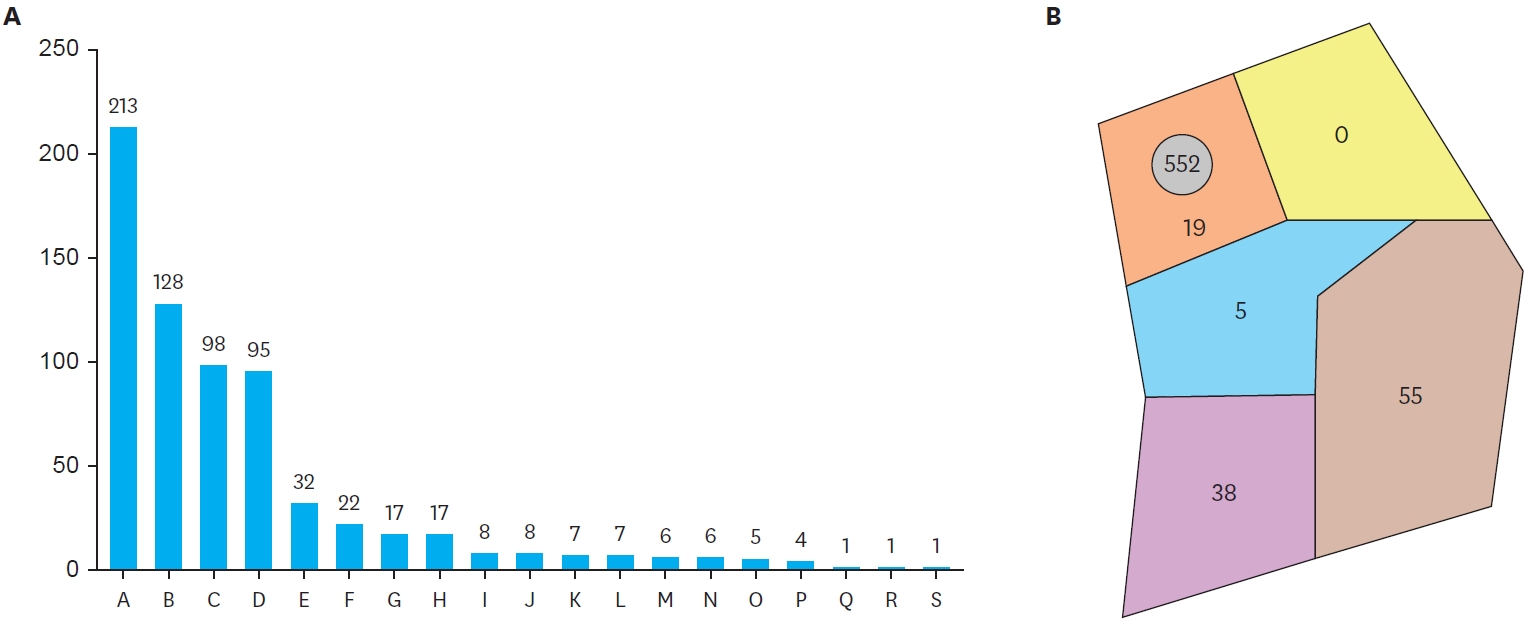
Fig. 2.Annual registration in this survey, not the representative figure of nationwide incidence. Mean value for yearly registration was 44.6, 1.04 for incident rate per 10,000 births.
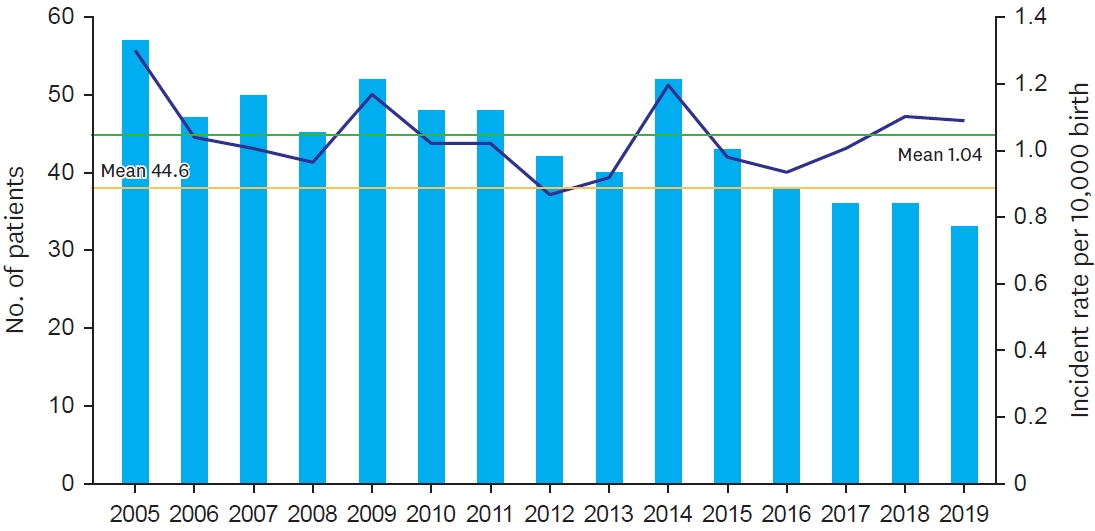
Fig. 3.
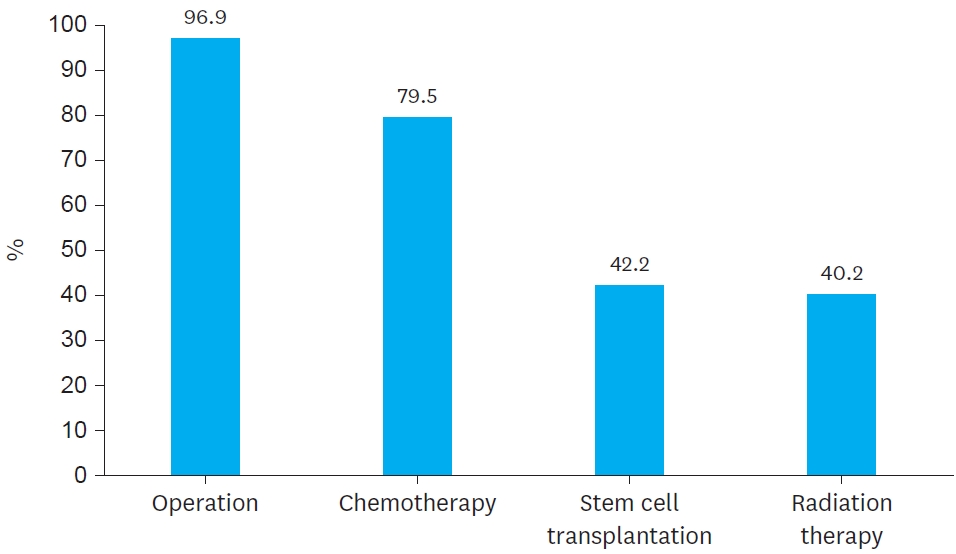
Fig. 4.
Survival graph.
Five-year DFS (A) and 5-year OS (B).
DFS, disease free survival; OS, overall survival.
a)Without recurrence 77 patients died, and 36 patients were alive with recurrence, making OS worse than DFS.
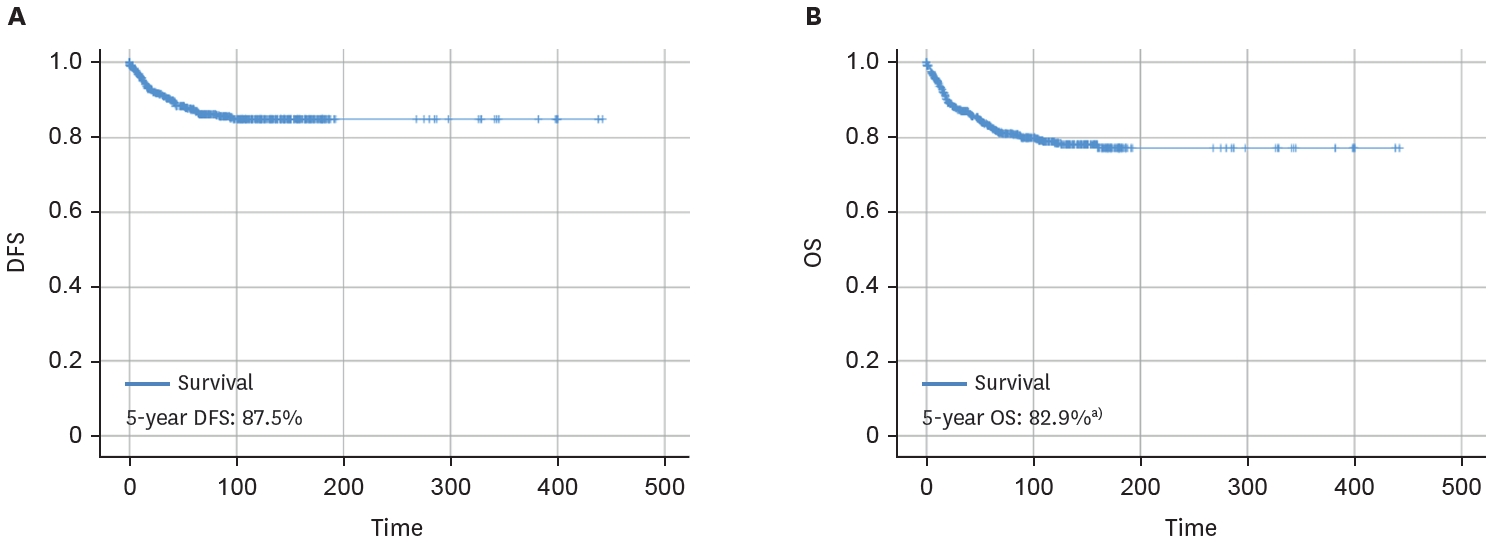
Fig. 5.
Disease free survivals by clinical factors. (A) Year, (B) Sex, (C) Age, (D) Location, (E) INSS stage, (F) Histology, (G) Size, (H) Extent of resection, (I) Combined resection.
INSS, International Neuroblastoma Staging System.
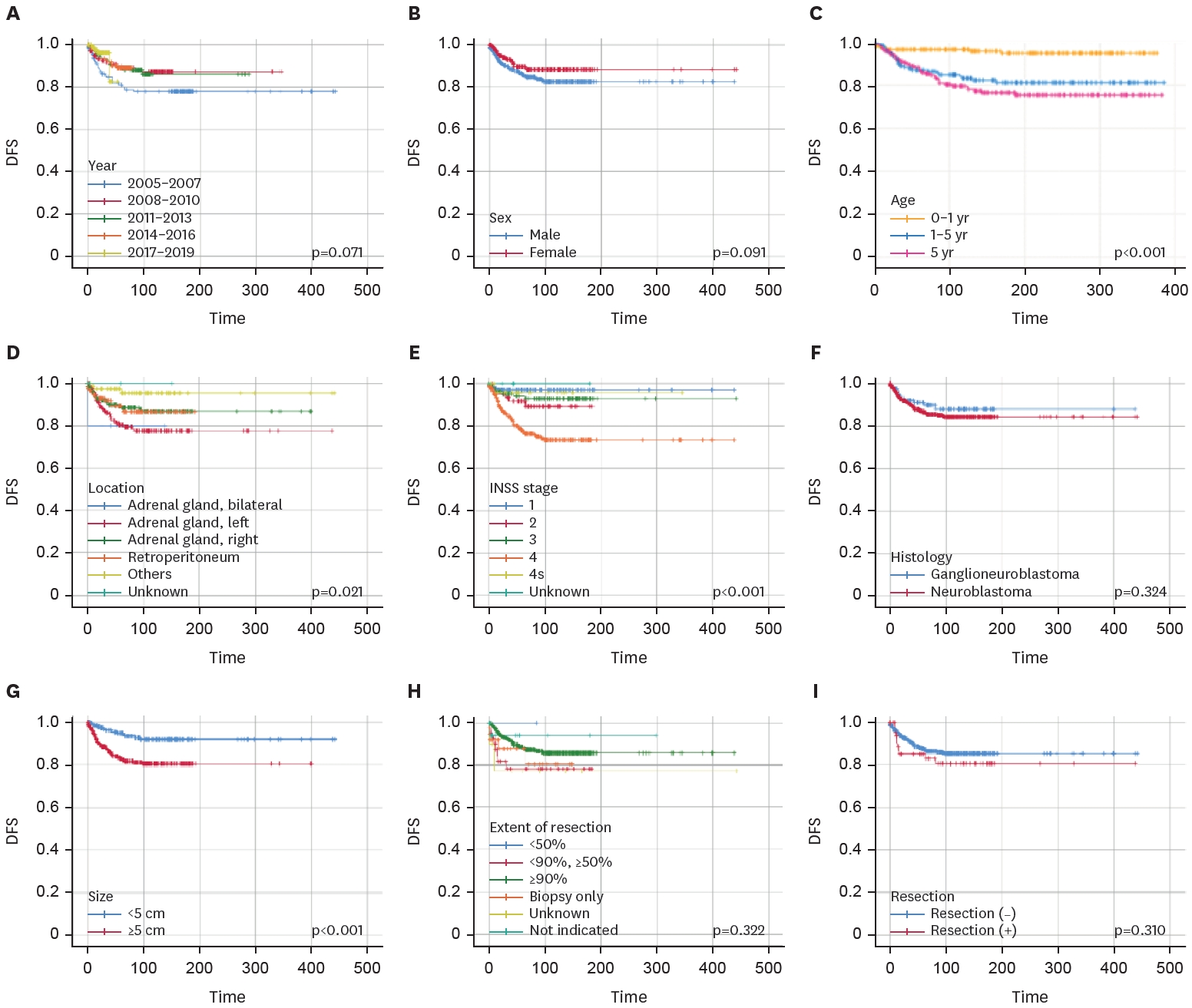
Fig. 6.
Overall survivals by clinical factors. (A) Year, (B) Sex, (C) INSS stage, (D) Age, (E) Location, (F) Size, (G) Operation, (H) extent of resection, (I) Chemotherapy, (J) Chemotherapy timing, (K) Radiation therapy, (L) Stem cell transplantation, (M) Reoperation, (N) Complication, (O) Recur.
INSS, International Neuroblastoma Staging System.
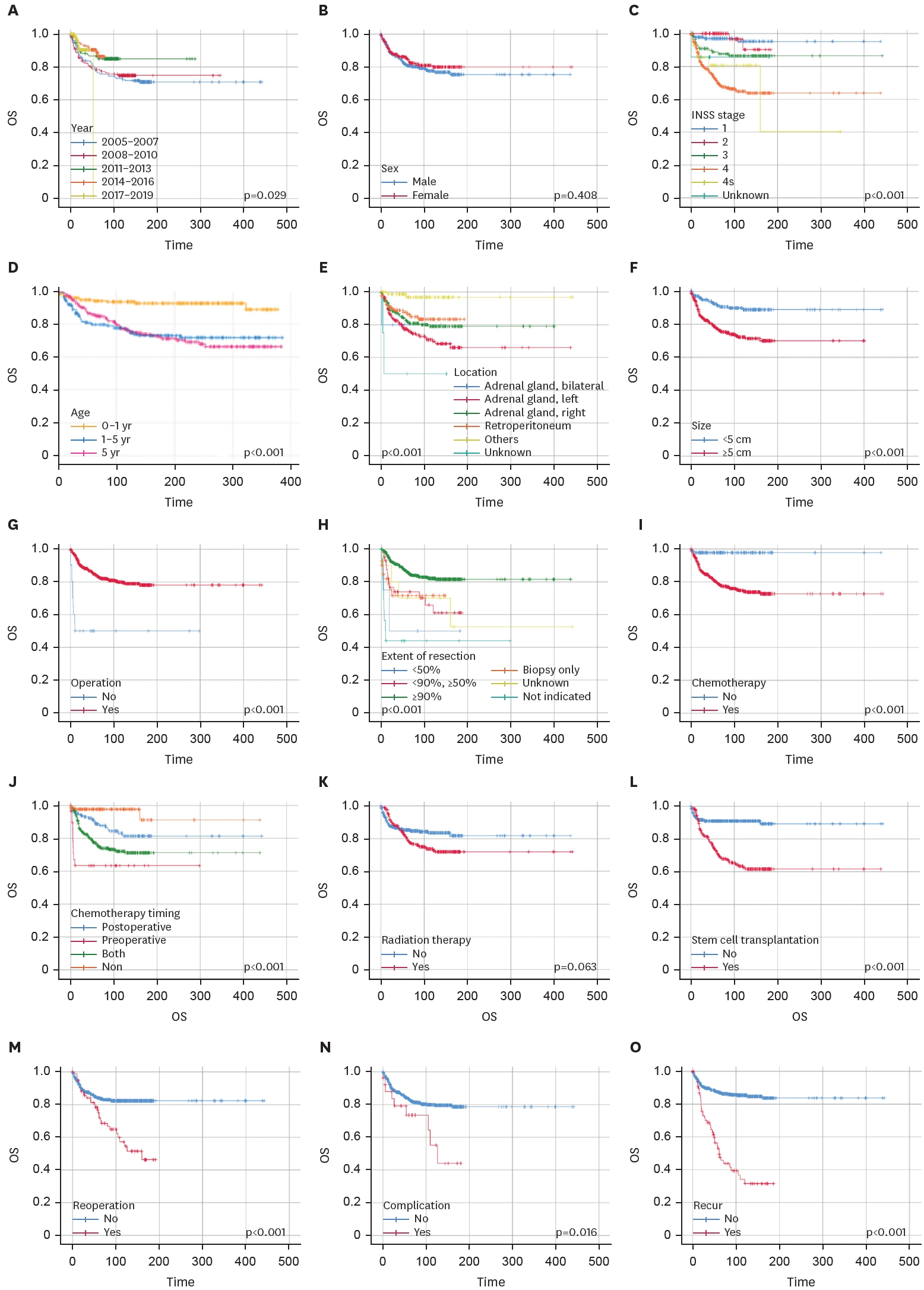
Table 1.
Table 1.
|
Factors |
Values (n=669) |
|
Sex |
|
|
Male |
386 (57.7) |
|
Female |
283 (42.3) |
|
Age at diagnosis (yr) |
2.1 (0.6-3.9) |
|
<1 yr |
217 (32.4) |
|
≥1 yr, <5 yr |
348 (52.0) |
|
≥5 yr |
104 (15.5) |
|
Size (cm, mean) |
|
|
At diagnosis |
6.6 |
|
At operation |
5.1 |
|
Difference |
1.5 |
|
Location |
|
|
Adrenal gland, left |
228 (34.1) |
|
Adrenal gland, right |
225 (33.6) |
|
Adrenal gland, bilateral |
5 (0.7) |
|
Retroperitoneum |
125 (18.7) |
|
Others |
83 (12.3) |
|
Unknown |
4 (0.6) |
|
Histology |
|
|
Neuroblastoma |
544 (81.3) |
|
Ganglioneuroblastoma |
125 (18.7) |
|
Biopsy |
|
|
Done |
576 (86.1) |
|
Not done |
87 (13.0) |
|
Unknown |
6 (0.9) |
|
INSS stage |
|
|
1 |
141 (21.1) |
|
2 |
63 (9.4) |
|
3 |
115 (17.2) |
|
4 |
315 (47.1) |
|
4s |
28 (4.2) |
|
Unknown |
7 (1.0) |
|
Follow up period (mo) |
69.4 (28.0-130.1) |
Table 2.Treatment-related factors
Table 2.
|
Factors |
Values |
|
Operation-related |
n=648 |
|
Operation method |
|
|
Open |
534 (82.4) |
|
Laparoscopy |
86 (13.3) |
|
Conversion to open |
28 (4.3) |
|
Extent of operation |
|
|
≥90% |
555 (85.6) |
|
<90%, ≥50% |
42 (6.5) |
|
<50% |
4 (0.6) |
|
Biopsy only |
41 (6.3) |
|
Unknown |
10 (1.5) |
|
Combined resection |
72 (11.1) |
|
Kidney |
33 (5.1) |
|
Liver |
9 (1.4) |
|
Vessel |
6 (0.9) |
|
Others |
24 (3.7) |
|
Complication |
26 (3.9) |
|
Ileus |
8 (1.2) |
|
Wound complication |
6 (0.9) |
|
Bleeding |
4 (0.6) |
|
Neurologic deficit |
3 (0.5) |
|
Other organ injury |
2 (0.3) |
|
Others |
3 (0.5) |
|
Reoperation |
79 (12.2) |
|
Residual mass or recurrence |
40 (6.2) |
|
Metastasis |
31 (4.8) |
|
Complication control |
11 (1.7) |
|
Chemotherapy-related |
n=532 |
|
Chemotherapy timing |
|
|
Neoadjuvant only |
30 (5.6) |
|
Adjuvant only |
149 (28.0) |
|
Both |
353 (66.4) |
|
Number of regimens |
|
|
1 |
321 (60.3) |
|
2 |
111 (20.9) |
|
3 |
54 (10.2) |
|
≥4 |
36 (6.8) |
Table 3.
Table 3.
|
Factors |
Values (n=669) |
|
Recurrence |
79 (11.8) |
|
Mortality |
120 (17.9) |
|
Tumor-related |
101 (84.2) |
|
Not related |
16 (13.3) |
|
Unknown |
3 (2.5) |
Table 4.Cox proportional hazard analysis for factors affecting overall survival
Table 4.
|
Factor |
Exp (B) |
95% confidence interval |
p-value |
|
Size ≥5 cm |
2.013 |
1.205-3.363 |
0.008 |
|
Resection ≥90% |
0.133 |
0.029-0.603 |
0.009 |
|
Recurrence |
3.237 |
2.097-4.996 |
<0.001 |
REFERENCES
- 1. National Cancer Center. Annual report of cancer statistics in Korea in 2016. Goyang: National Cancer Center; 2018.
- 2. National Cancer Center. Annual report of cancer statistics in Korea in 2017. Goyang: National Cancer Center; 2019.
- 3. National Cancer Center. Annual report of cancer statistics in Korea in 2018. Goyang: National Cancer Center; 2020.
- 4. National Cancer Center. Annual report of cancer statistics in Korea in 2019. Goyang: National Cancer Center; 2021.
- 5. National Cancer Center. Annual report of cancer statistics in Korea in 2020. Goyang: National Cancer Center; 2022.
- 6. Qiu B, Matthay KK. Advancing therapy for neuroblastoma. Nat Rev Clin Oncol 2022;19:515-33.
- 7. London WB, Castleberry RP, Matthay KK, Look AT, Seeger RC, Shimada H, et al. Evidence for an age cutoff greater than 365 days for neuroblastoma risk group stratification in the Children’s Oncology Group. J Clin Oncol 2005;23:6459-65.
- 8. Mahapatra S, Challagundla KB. Neuroblastoma. Treasure Island (FL): StatPearls Publishing; 2023.
- 9. PDQ Pediatric Treatment Editorial Board. Neuroblastoma treatment (PDQ®): health professional version. In: PDQ Cancer Information Summaries [Internet]. Bethesda (MD): National Cancer Institute; 2002.
- 10. Ma Y, Zheng J, Feng J, Chen L, Dong K, Xiao X. Neuroblastomas in Eastern China: a retrospective series study of 275 cases in a regional center. PeerJ 2018;6:e5665.
- 11. Irwin MS, Naranjo A, Zhang FF, Cohn SL, London WB, Gastier-Foster JM, et al. Revised neuroblastoma risk classification system: a report from the Children’s Oncology Group. J Clin Oncol 2021;39:3229-41.
- 12. Wang JX, Cao ZY, Wang CX, Zhang HY, Fan FL, Zhang J, et al. Prognostic impact of tumor size on patients with neuroblastoma in a SEER-based study. Cancer Med 2022;11:2779-89.
- 13. Zwaveling S, Tytgat GA, van der Zee DC, Wijnen MH, Heij HA. Is complete surgical resection of stage 4 neuroblastoma a prerequisite for optimal survival or may >95 % tumour resection suffice? Pediatr Surg Int 2012;28:953-9.
- 14. Fischer J, Pohl A, Volland R, Hero B, Dübbers M, Cernaianu G, et al. Complete surgical resection improves outcome in INRG high-risk patients with localized neuroblastoma older than 18 months. BMC Cancer 2017;17:520.
- 15. Seemann NM, Erker C, Irwin MS, Lopushinsky SR, Kulkarni K, Fernandez CV, et al. Survival effect of complete surgical resection of the primary tumor in patients with metastatic, high-risk neuroblastoma in a large Canadian cohort. Pediatr Blood Cancer 2023;70:e30286.
 , Soo Min Ahn1, Min Jeng Cho1, Yong-Hoon Cho1, Soo Jin Na Choi1, Yoon Mi Choi1, Jae Hee Chung1, Seok Joo Han1, In Geol Ho1, Jeong Hong1, Kyong Ihn1, Yeon Jun Jeong1, Eunyoung Jung1, Dae Youn Kim1, Hae-Young Kim1, Ki Hoon Kim1, Seong Chul Kim1, Soo-Hong Kim1, Eun-Jung Koo1, Hyun Hee Kwon1, Yong Jae Kwon1, Nam-Hyuk Lee1, Ju Yeon Lee1, Sanghoon Lee1, Jung-Man Namgoong1, Chaeyoun Oh1, Jung-Tak Oh1, Jin Young Park1, Junbeom Park1, Jeong-Meen Seo1, Jae Ho Shin1, Hyun Beak Shin1, Joohyun Sim1, Jiyoung Sul1, Joon Kee Youn1, Hyun-Young Kim1,3
, Soo Min Ahn1, Min Jeng Cho1, Yong-Hoon Cho1, Soo Jin Na Choi1, Yoon Mi Choi1, Jae Hee Chung1, Seok Joo Han1, In Geol Ho1, Jeong Hong1, Kyong Ihn1, Yeon Jun Jeong1, Eunyoung Jung1, Dae Youn Kim1, Hae-Young Kim1, Ki Hoon Kim1, Seong Chul Kim1, Soo-Hong Kim1, Eun-Jung Koo1, Hyun Hee Kwon1, Yong Jae Kwon1, Nam-Hyuk Lee1, Ju Yeon Lee1, Sanghoon Lee1, Jung-Man Namgoong1, Chaeyoun Oh1, Jung-Tak Oh1, Jin Young Park1, Junbeom Park1, Jeong-Meen Seo1, Jae Ho Shin1, Hyun Beak Shin1, Joohyun Sim1, Jiyoung Sul1, Joon Kee Youn1, Hyun-Young Kim1,3