Lymphatic malformations are benign congenital malformations of the lymphatic system that occur predominantly in children. Most lymphatic malformations occur in the head and neck region, with those in abdominal locations, such as the mesentery, omentum and retroperitoneum, being less common, accounting for fewer than 5% of lymphatic malformations in children. This study analyzed the clinicopathologic characteristics and treatment outcomes of abdominal lymphatic malformations in children.
The medical records of 12 pediatric patients treated for abdominal lymphatic malformations at our institution between April 1999 and September 2017 were retrospectively reviewed. Demographic and clinical characteristics, including gender, age, symptoms and signs, diagnostic modalities, and treatment results, were analyzed.
The 12 patients included 11 boys and 1 girl, ranging in age from 3 months to 17 years (median 36.5 months) at presentation. The primary signs and symptoms included abdominal pain, abdominal mass and abdominal distention. Other symptoms and signs included fever, vomiting, scrotal pain and mass, and right inguinal mass. All patients were diagnosed by abdominal ultrasonography and computed tomography, and all underwent surgical excision with or without bowel resection. The lymphatic malformations occurred in the retroperitoneum (n=4), omentum (n=4), jejunal mesentery (n=2), and retroperitoneum and mesentery (n=2). Seven patients underwent complete mass excision, including 3 who underwent laparoscopic excisions, and 3 who underwent mass excision with segmental resection of the adjoining bowel. Two patients underwent incomplete excision because the lesion was extensive and invaded the superior mesenteric vessels. There was no major perioperative morbidity in any patient. At a median follow-up of 50 months (range, 8–183 months), only 1 patient experienced recurrence.
Although abdominal lymphatic malformations are benign, most children present with acute abdominal symptoms, necessitating early surgical treatment.
Although gallbladder (GB) hydrops in childhood is uncommon, it is most commonly associated with Kawasaki disease (KD) and can be a risk factor of poor outcomes in patients with KD. Our patient presented with a fever, diffuse abdominal pain, maculopapular rash, bilateral conjunctivitis, red and fissured lip tissue, and 3 days of right cervical swelling. Abdominal examination revealed abdominal distension and tenderness. Abdominal ultrasonography was performed to identify the source of abdominal symptoms, which revealed dilatation of the GB. Abdominal computed tomography scan was also performed to exclude other hepatobiliary disease, which showed normal hepatobiliary systems. The GB of our patients returned to a normal size without any complications, but it regressed very slowly. We report a case of a 6-year-old boy with KD who presented with markedly distended and unusually prolonged GB hydrops.
Gardner-associated fibroma (GAF) is a benign lesion of soft tissue which has recently been described and is exceedingly rare in children. GAF is associated with adenomatous polyposis coli gene mutation, familial adenomatous polyposis and desmoid. We report a case of patient with soft tissue tumor on her lower back which was turned out to be GAF. The patient was a 19-month-old female who visited out-patient clinic with palpable mass on her lower back and we performed surgical excision. The tumor was located at subcutaneous and we excised the tumor including surrounding soft tissue. She discharged without any complication on surgery day. The pathologic report showed dense collagenous tissue with spindle cell and adipose tissue, suggestive of GAF. We are planning to check gene study and to perform endoscopy and abdominal ultrasonography for at the age of 4.
The aim of this study was to analyze of the risk factors for surgical procedure on ileo-colic intussusception without leading point in children.
We retrospectively reviewed medical records of patient treated for ileo-colic intussusception between January 2003 and December 2014. We exclude the patients who had leading point. Because of the large difference on patient's numbers between non-operative group (cases of ileo-colic intussusceptions successfully reduced by air reduction) and operative group (cases underwent operation due to failed air reduction), we compared the data of operative group of patients without leading point between 2003 and 2014 with the data of non-operative group as control group from 2013 to 2014. Clinical features such as gender, age, body temperature, body weight in diagnosis, growth curves for age-gender-body weight, and laboratory data of blood test were compared.
In non-operative group, total 94 patients who were treated successfully by the non-operative air reduction. In operative group, total 21 patients treated by surgical procedure. The age under 12 months, weight over upper 75 percentile group, increased segment neutrophil count, decreased hemoglobin level and lymphocyte count were significantly associated with a requirement for surgical procedure.
We conclude that younger age, higher weight percentile group, increased segment neutrophil, decreased hemoglobin and lymphocyte are the independent risk factors related to operative treatment for ileo-colic intussusception in children. If primary air reduction is failed in patients with such risk factors, operative treatment over ultrasonography or secondary reduction can prevent unnecessary effort and complications, thus emphasizing the consideration of operative treatment when selecting treatment methods.
Nodular hidradenoma was diagnosed in a 29-month-old girl on her axilla. Hidradenoma, sometimes designated as acrospiroma, is a benign sweat gland neoplasm, which mostly occurs in adults. Very few cases of hidradenoma have been documented in children in their first decade of life. This case demonstrates that when a child develops a skin nodule, nodular hidradenoma can be a diagnostic option.
The present study compared the postoperative analgesic effects of ilioinguinal and iliohypogastric nerve block with infiltration of local anesthetics (bupivacaine) into the wound in children after inguinal hernia repair. Ninety children below 7 years old who were scheduled elective inguinal hernia repair were randomly allocated into one of three groups. The patients in nerve block (NB) group, ilioinguinal and iliohypogastric nerve block was done with 0.5 mL/kg of 0.25% bupivacaine. The patients in infiltration of local anesthetics (LI) group, 0.5 mL/kg of 0.25% bupivacaine was infiltrated into the wound after surgery. The patients in control group were allocated as a Control group. Postoperative pain was assessed at 1, 3, 5, and 24 hours after operation with FLACC scale and additional analgesic consumption were counted. The three groups were not significantly different in age, sex, body weight, and duration of operation. Pain scores at 1 hour and 3 hours after operation were significantly higher in Control group than in NB group and LI group (
The aim of this study was to identify the risk factor related to the need for operative treatment and avoid unnecessary non-operative management for intussusception in children. We retrospectively reviewed medical records of patient treated for intussusception at our institution between January 2006 and January 2013. Clinical features such as gender, age, seasonal variation, symptoms and signs, treatment results were analyzed. Univariate and multivariate analyses including a chi-square test for categorical variables and logistic regression analysis were performed. During the study period, 356 patients were treated for intussusception. 328 (92.1%) was treated successfully by the non-operative pneumoreduction, and 28 (7.9%) required operative management. On univariate analysis, risk factors which were related to the need for operative treatment were age, vomiting, bloody stool, lethargy, and symptoms duration. A logistic regression analysis in order to assess for independent predictors of operative treatment was performed. Age (<6 vs ≥12 months) (OR 4.713, 95% CI 1.198~18.539,
Foreign body ingestion is a common problem among paediatric populations. Most of the ingested foreign bodies spontaneously pass through the gastrointestinal tract, but approximately less then 10% of them remain without being discharged, and trigger complications. Therefore, proper evaluation and treatment according to the situation is required. In this study, clinical progress and complications were analyzed according to the clinical features and treatment in children who ingested foreign bodies. Among pediatric patients under 18 who were admitted to Chonnam National University Hospital after ingesting foreign bodies between January 2008 to June 2012, only the patients who had their foreign body in the gastrointestinal tract were included in this study. Based on medical records, age, type of foreign body, time spent till admission, and whether the endoscopy was done or not, complication were researched retrospectively. According to symptoms and plain abdomen X-ray findings, treatment was chosen and conducted among endoscopy, observation and emergency operation. Among 273 patients, 9 (3.3%) of them had surgical removal. Seven (2.6%) of them had an emergency operation on the day of admission, and the rest 2 (0.7%) had operation during observation. Removal through initial endoscopic approach was tried in 157 (57.5%) patients. Eleven (70.8%) of them had their foreign body removed at the initial trial, and 5 (4.9%) of them at the second trial. Among 109, who were on observation status, 9 (8.3%) of them needed endoscopic removal, and 2 (1.8%) of them suffered from surgical removal. It is thought to be better to approach slowly considering the type, size and symptoms in foreign body ingestion of pediatric patients, rather than immediate and invasive removal.
Ketamine is a safe and effective drug for pediatric anesthesia, sedation and analgesia. We hoped to identify that surgeons could operate a pediatric hernia with the ketamine anesthesia without general anesthesia. The study was a consecutive case series of 2230 inguinal hernia patients aged 1 months to 17 years in a Joo's day-surgical clinic during 11-year period. The patients had pediatric inguinal hernia surgery without general anesthesia under the day-surgery system. We retrospectively analyzed the medical record of patients who were registered with the Diagnosis Related Group (DRG) system. All patients received ketamine (5mg/kg) and atropine (0.01mg/kg) intramuscularly before surgery. After anesthesia, we injected 1~2% lidocaine (Less than 5ml) subcutaneously at the site of incision and started operation. The surgical method was the high ligation method of the hernia sac.) In total 2230 patients, male were 1756 and female were 474. 2076 patients were a unilateral inguinal hernia at the time of surgery and 154 were bilateral hernia patients. Less than three months, depending on the age of the patients was 391, and less than 12 months the patient was 592 people (26.5%). After surgery, there were no accidents or long term complications associated with ketamine anesthesia. We think the surgeon can safely do the pediatric inguinal hernia surgery using ketamine and lidocaine without anesthesiologist through 11 years of our surgical experiences.
The purpose of this study is to analyze the early experience of the laparoscopic adhesiolysis for the intestinal obstruction due to postoperative adhesion. Seven patients were included in this study. The median age of those patients was 13, and there were 3 males and 4 females. Previous diagnosis and surgical procedure were various in seven cases, including small bowel resection with tapering enteroplasty, Boix-Ochoa fundopl ication, Ladd's procedure with appendectomy, mesenteric tumor resection with small bowel anastomosis, ileocecal resection and anastomosis, primary gastric repair, and both high ligation. A successful laparoscopic adhesiolysis was performed in one who had high ligation for inguinal hernia and had a single band adhesion. Six out of 7 (86%) cases needed to convert open surgery due to multiple and dense type of adhesion. In conclusion, laparoscopic approach with postoperative small bowel adhesion seems safe. However, it might be prudently considered because of high rates of conversion in children.
Pediatric liver transplantation has evolved into a definite and effective therapeutic modality for various liver diseases in the pediatric patient. During the last 25 years, liver transplant outcomes in Korea have reached international standards and Korea has become the leader in living-donor liver transplantation. This review will present the cumulative outcomes of pediatric liver transplantation performed in Korea and will focus on other issues of interest involving pediatric liver transplant recipients, especially in the field of immunosuppression and post-transplant lymphoproliferative disease.
Branchial cleft anomalies are the second most common head and neck congenital lesions seen in children. Amongst the branchial cleft malformations, second cleft lesions account for 95 % of the branchial anomalies. This article analyzes all the cases of second branchial cleft anomalies operated on at Seoul National University Hospital from September 1995 to February 2011. We analyzed sex, age, symptom and sign, accompanied anomaly, diagnosis, treatment, pathologic report and outcome via retrospective review of medical records. In this series, we had 61 patients (27 female and 34 male). The mean age at the time of operation was 38 months. 31 lesions were on the right, 20 were on the left and 10 were bilateral. The most frequent chief complaints at presentation were non-tender mass and cervical opening without any discharge. According to anatomic type, 29 patients had branchial cleft sinuses, 14 had cysts, 14 had fistulas and 4 had skin tags. Complete excision was attempted if possible and antibiotics challenged when infection was suspected. Complete excision was achieved in 96.7 % of cases. Incision and drainage was done in 2 cases due to severe inflammation, and both recurred. Postoperative complications included wound infection in 2 cases. Microscopic examonation revealed squamous epithelium in 90.2 % and squamous metaplasia in one case in the branchial cleft cyst wall. In summary, second branchial anomaly is found more frequently on right side of neck. Fistulas are diagnosed earlier than cystic forms. Most cases could be diagnosed by physical examination. The definitive treatment is complete excision and sufficient antibiotics coverage for cases with inflammation. After drainage of infected lesions, follow up excision after 1 year might be beneficial for preventing recurrence.
Acute appendicitis is one of the most common diseases of young people that requires emergency operation. This is especially true for those age 10 years old and older. However, the numbers of cases of appendicitis are increasing in both the young and the elderly. The main purpose of this study is to understand the clinical features of acute appendicitis in children and elderly patients. We retrospectively compared clinical characteristics in 4 groups of patients who underwent appendectomy in our hospital. There were 16 patients in the pre-school age group, 9 were males and 7 females. The total number of patients in the juvenile group were 287, 156 were males and 131 females. The total numbers of patients in the adult group were 794, 436 were males and 358 females. The numbers of elderly patients were 189, 91 were males and 98 females. Complicated appendicitis was found in 15 patients (93.7 %) in the pre-school age group, 79 patients (27.5 %) in the juvenile group, 332 patients (41.8 %) in the adult group, and 96 patients (50.7 %) in the elderly group. Four patients (40 %) had generalized panperitonitis in the pre-school group. The occurrence of perforated appendicitis was the highest in the pre-school age group and the lowest in the juvenile group. Since generalized panperitonitis has a higher incidence in the pre-school age group, prudent and careful diagnosis and treatment are required for the pre-school age group.
Minimally invasive techniques for pediatric inguinal hernia repair have been evolving in recent years. We applied the laparoscopic method to repair pediatric inguinal hernia using the techniques of sac transection and intra-corporeal ligation. Between November 2008 and August 2010, 67 pediatric patients (47 boys and 20 girls) with inguinal hernias were included in this study. Postoperative activities, pain, and complication were checked prospectively at regular follow-up. One patient presented with clinically bilateral hernia, and three patients had metachronous hernias. Thirty-two cases out of 63 patients with unilateral hernias had a patent processus vaginalis on the contralateral side. Mean operation time was 35±11.4 minutes for unilateral hernias and 43±11 minutes for bilateral hernias. There were no intra-operative complications. One patient had a small hematoma on the groin postoperatively, which subsided spontaneously in a week. Recurrence and metachronous hernia were not found at follow up. In summary, laparoscopic inguinal repair in children is safe, easy to perform and has an additional advantage of contralateral exploration. Further studies should include long term follow-up.
Thyroglossal duct cysts (TGDC) are the most common type of congenital developmental anomaly encountered in the anterior midline of the neck in childhood. The aim of the study was to evaluate the clinical characteristics of TGDC and identify any factors that could be related to recurrence after surgery. This study consisted of a retrospective chart review of 45 patients treated at Kyungpook National University Hospital for TGDC between 1990 and 2008. All records were reviewed for age and sex, length of history, presentation, diagnostic methods, sizes and locations of cyst, surgical management, histopathology of the lesion and recurrences. The statistical analysis of risk factors for recurrence was made using the Fisher's exact test with a significance level of p < 0.05. The male to female ratio was 2.2:1 with a male preponderance. The mean age at operation was 5 years and 2 months (4 months – 17 years). The most common presenting symptom was a nontender cervical mass (78%). Most TGDC were found in the midline position. Twenty four were infrahyoid, 17 were hyoid, and 4 were suprahyoid level. Forty one (91%) patients received the Sistrunk operation, and 4(9%) patients received cyst excision. Postoperative a seroma developed in six patients in the early postoperative days. There were a total of 3(6.6%) recurrences, 2 in patients who had excision only and in one patient who had the Sistrunk operation. Univariate analysis for risk factors with recurrence showed that there was no statistical relationship between the presence of preoperative infection and the development of recurrence. The removal of hyoid bone along with TGDC was a statistically significant risk factor for recurrent disease. This study suggests that the Sistrunk operation is the treatment of choice for TGDC in order to reduce recurrence.
Traumatic injury is one of the leading causes of morbidity and mortality in children. This is a clinical review of pediatric blunt abdominal trauma. A retrospective analysis of the 112 children with blunt abdominal trauma aged 15 years or less treated at the Department of Pediatric Surgery, Chonbuk National University Hospital was performed. The analysis included age, sex, injury mechanism, number and site of the injured organ, management and outcomes. The average age of occurrence was 7.6 years, and the peak age was between 6 and 8 years. There was a male preponderance with a male to female ratio of 2.3:1. The most common cause of blunt abdominal trauma was traffic accidents (61.6%), principally involving pedestrians (79.7%). The accident prone times were between 8:00 AM and 8:00 PM, the weekends (40.2%), and the winter respectively. Thirthy-five patients (31.2%) had multiple intra-abdominal organ injuries and the most common injured organ was the liver. Seventy-four cases (66.1%) were managed non-operatively and eleven cases (9.8%) expired. Of the patients who were treated surgically or were to be operated on one patient died before surgery, the remainder died during or after surgery. Risk factors such as number of injured organ, systolic and diastolic blood pressure, and trauma scores by Glasgow coma scale (GCS), Pediatric trauma score (PTS), revised trauma score (RTS), injury severe score (ISS), TRISS were significantly correlated with mortality rate.
Malignant ovarian tumors in children are very rare, and consist of about 1% of all childhood malignant tumors. The purpose of this study is to examine the clinical characteristics, treatment, and prognosis for children with malignant ovarian tumors. We retrospectively reviewed the medical records of children under 15 years of age with malignant ovarian tumors who had been treated surgically at Asan Medical Center between 1989 and March 2009. There were 32 patients, ranged in age at surgery from 2 to 15 years (mean; 10.4 years). The median follow-up period was 64.7 months (from 1 month to 188 months). Pathologic diagnosis were; immature teratoma (n=10), mixed germ cell tumor (n=10), and dysgerminoma (n=6). Tumor stage was classified by the staging system of the International Federation of Gynecology and Obstetrics (FIGO). The number of patients in stage I, II, III, and IV were 24 (75%), 2 (6.2%), 4 (12.5%), and 2 (6.1%), respectively. The tumor recurred in 4 patients. Seven patients of group 1 did not receive postoperative adjuvant chemotherapy, and in three of them, the tumor recurred. Twenty-five patients (group 2) underwent postoperative adjuvant chemotherapy, and there was only one recurrence. One patient who did not receive postoperative adjuvant chemotherapy and expired 10 months after operation because of tumor recurrence and distant metastasis. The overall 5-year event free survival (EFS) was 84.2%: group 1 in 44.4%, and group 2 in 95.7%. Tumor recurrence was related to the postoperative adjuvant chemotherapy (p=0.004). In conclusion, proper surgical procedures with relevant postoperative adjuvant chemotherapy might improve clinical results in children with malignant ovarian tumors.
Condyloma acuminatum is an uncommon disease but there is an increased incidence reported in recent years in prepubertal children. Anal and perianal condyloma accuminatum in children may suggest sexual abuse and treatment should include the thorough social evaluation as well as medical treatment. A 25 month old girl presented with multiple sessile nodules around her anal and perianal area, Biopsy confirmed the diagnosis of condyloma accuminatum. There was no definite evidence of sexual abuse, but her father had condyloma accuminatum involving his penis. The patient's lesions were excised totally. At three week follow up there was no anal stricture but there were newly developed small lesions around perianal area. Imiquimod onit was applied for 2 weeks and the recurred lesion disappeared completely. At postoperative 5 month, the operative area was fully epithelialized without recurrence.
Hickman catheters are tunneled central venous catheters used for long-term venous access in children with malignancies. The appropriate management for various kinds of catheter related complications has become a major issue. We retrospectively analyzed the clinical, demographic, and surgical characteristics in 154 pediatric hemato-oncology patients who underwent Hickman catheter insertion between January 2005 and December 2009. There were 92 boys and 62 girls. The mean age at surgery was 7.6±5.1 years old. The mean operation time was 67.4±21.3 minutes and C-arm fluoroscopy was used in 47(30.5%). The causes of Hickman catheter removal were termination of use in 82 (57.3%), catheter related bloodstream infection in 44(30.8%), mechanical malfunction in 11(7.7%), and accidents in 6(4.2%). Univariate and multivariate analysis for associated factors with catheter related bloodstream infection showed that there were no statistically significant associated factors with catheter related infection complications. All cases except two showed clinical improvement with catheter removal and relevant antibiotics treatment. The mean catheter maintenance period in patients of catheter removal without complications was 214.9±140.2 days. And, The mean catheter maintenance period in patients of late catheter related bloodstream infection was 198.0±116.0 days. These data suggest that it is important to remove Hickman catheter as soon as possible after the termination of use. When symptoms and signs of complications were noticed, prompt diagnostic approach and management can lead to clinical improvements.
Pancreatic tumors in children are relatively rare, and their prognosis differs from that in adults. The purpose of this study is to examine the clinical characteristics, treatment, and prognosis for children with pancreatic tumors. We retrospectively reviewed the medical records of children under 15 years of age with pancreatic tumors who were treated surgically at Asan Medical Center between January 1992 and November 2009. There were 16 patients, fourteen of whom were pathologically diagnosed with solid pseudopapillary tumor. The other two patients were diagnosed with pancreatoblastoma and acinar cell carcinoma, respectively. Six patients of the 16 patients (38%) were male, and there was a male-to-female ratio of 1:1.6. The initial presentations were upper abdominal pain in eight patients (50%), palpable abdominal mass in three, and vomiting in one. Four patients were diagnosed incidentally. Six patients' tumors were located in the pancreatic head, six in the pancreatic body, and four in the pancreatic tail, respectively. The surgical procedures performed included distal pancreatectomy (n=7, 44%), median segmentectomy (n=3), enucleation (n=3), pancreaticoduodenectomy (n=2), and pylorus-preserving pancreaticoduodenectomy (n=1). Three patients underwent laparoscopic surgery. The median tumor size was 6.5cm (1.8~20 cm). Early surgical complications included pancreatic fistula (n=4), bile leakage (n=1), and delayed gastric emptying (n=1). A late complication in one patient was diabetes. The median follow-up period was five years and four months, and all patients survived without recurrence. While pancreatic tumors in adults have a poor prognosis, pancreatic tumors of childhood are usually curative with complete resection and thus have a favorable prognosis.
Contralateral groin exploration (CGE) in children with unilateral inguinal hernia remains controversial. Between January 2002 and December 2007, 1967 pediatric patients with inguinal hernia were treated by two surgeons with different criteria of CGE (group A; boys younger than 2 years, older boys prematurely delivered, and all girls, B; birth weight lower than 2kg with inguinal hernia presentation within 6 months after birth, and suspicious physical findings) at Samsung medical center. Patient's age, sex, body weight, diagnosis, and metachronous contralateral inguinal hernia (MIH) incidence were analyzed retrospectively. Among 895 patients in group A, CGE was performed in 460 patients (66.4%) and MIH incidence was 1.7%. In group B, 31 patients (3.5%) had CGE among 1072 patients, and MIH incidence was 4.2%. The average hospital costs of group A and B were 763,956 won and 500,708 won, respectively. The CGE criteria of group B had advantage in total hospital cost. The primary site and the age at presentation had a signiticant effect on the incidence of MIH. But MIH incidence was low and the more contralateral explorations lead to increase of total costs. Therefore, routine contralateral groin exploration and surgery for a patent processus vaginalis could not be justified.
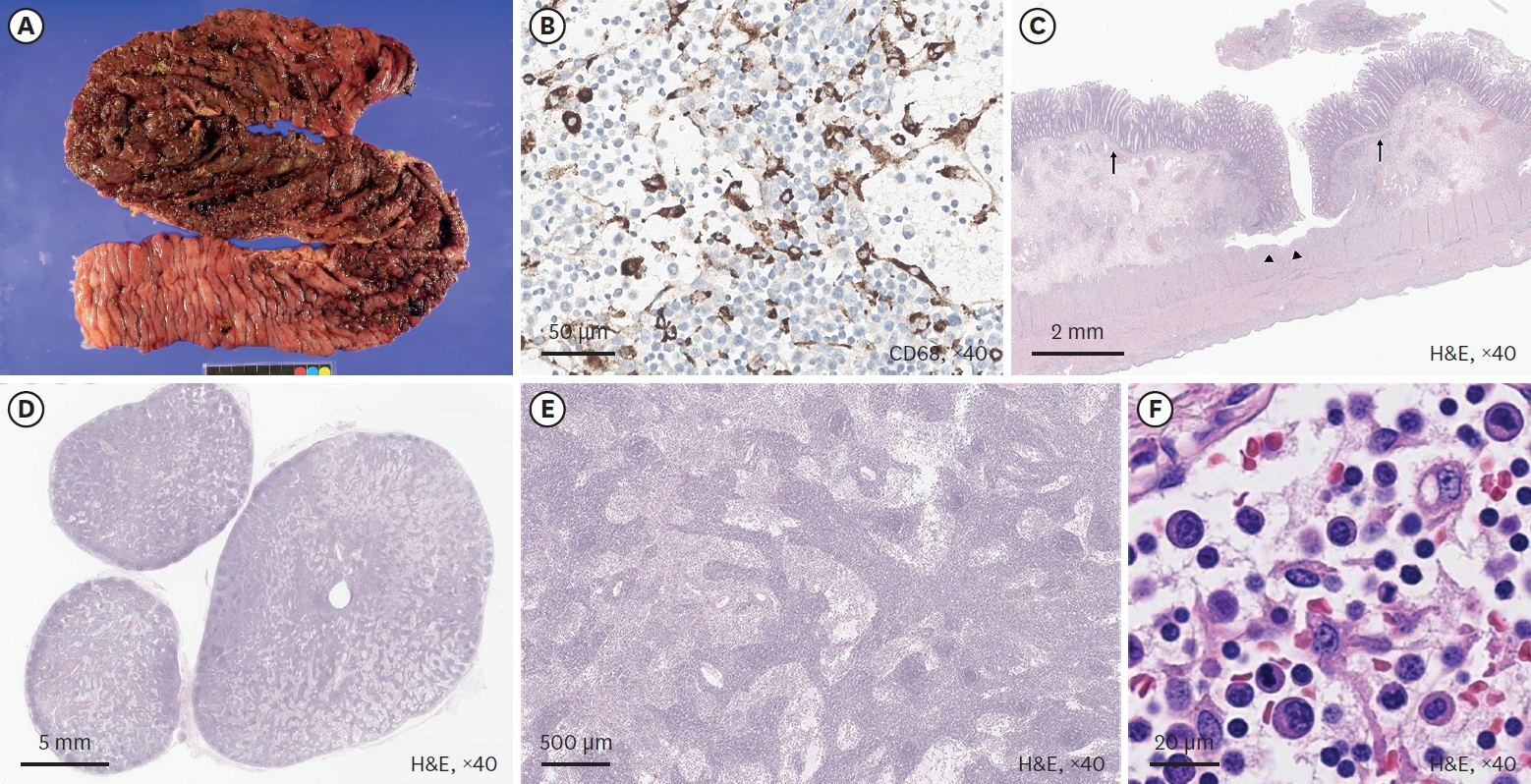
Catheter related and perianal problems are common surgical complications encountered during the treatment of pediatric malignancies. However acute surgical abdominal emergencies are rare. The aim of this study is to review acute surgical abdominal complications that occur during the treatment of childhood malignancies. Out of a total of 1,222 patients who were newly diagnosed with malignant disease, between January 2003 and May 2008, there were 10 patients who required surgery because of acute abdominal emergencies. Their medical records were reviewed retrospectively. Hematologic malignancies were present in 7 patients (4 leukemia, 2 lymphoma, 1 Langerhans cell histiocytosis) and solid tumors in 3 patients (1 adrenocortical carcinoma, 1 desmoplastic small round cell tumor, 1 rhabdomyosarcoma). Seven patients had intestinal obstruction, two had gastrointestinal perforation and one, typhlitis. Intestinal obstructions were treated with resection of the involved segment with (N=2) or without (N=3) enterostomy. Two patients had enterostomy alone when resection could not be performed. Intestinal perforation was treated with primary repair. Typhlitis of the ascending colon was treated with ileostomy. Right hemicolectomy was necessary the next day because of the rapidly progressing sepsis. Three patients are now alive on chemotherapy and one patient was lost to followed-up. Among six patients who died, five died of their original disease progression and one of uncontrolled sepsis after intestinal perforation. Although rare, acute surgical abdominal complications can occur in childhood malignancies. Rapid and accurate diagnosis and appropriate operation are required for effective treatment of the complications.
Inflammatory myofibroblastic tumor (IMT) is a rare reactive lesion characterized by the feature of myofibroblasts and a mixed inflammatory infiltrate that rarely undergoes malignant transformation. Extrapulmonary IMTs in children have been described involving the mesentery, omentum, retroperitoneum, abdominal soft tissues, liver, bladder, mediastinum, head and neck, extremity, appendix, and kidney. Medical records of children treated with abdominal IMT between 1985 and 2005 were reviewed retrospectively. Seven children were treated for IMT with the mean age of 3y 2m (range, 1y 1m to 14y). Tumors were located in transverse mesocolon (n=2), omentum (n=1), porta hepatis (n=2), complex site (antrum, duodenum, common bile duct, porta hepatis) (n=2). The symptoms included abdominal mass, fever, jaundice, abdominal pain and anemia. The masses were excised totally in transverse mesocolon, omentum IMT and there is no evidence of recurrence (follow-up periods: 6y 8m, 8y 9m, 4y 10m). In porta hepatis IMT, liver transplantations were performed and there is no evidence of recurrence (follow period: 6y 8m, 8y 7m). In one case of complex site IMT, partial excision of mass was performed and he still survived with no change of the residual tumor during follow-up period. The other one of complex site IMT denied further treatment after the biopsy. In conclusion, complete surgical excision including liver transplantation and close follow-up are mandatory for the abdominal IMT in child.
Children who underwent reparative operations for esophageal atresia (EA) with or without tracheoesophageal fistula (TEF), are confronted with many gastrointestinal or respiratory problems, especially during the early years of life. We reviewed the medical records of 50 patients who underwent repairs of EA with or without TEF at the Division of Pediatric Surgery, Samsung Medical Center, from December 1994 to December 2005. Current status of children was accessed by telephone-interview, but only 27 of them were accessible. Of 50 patients, 3 patients (6%) were type A, 45 patients (90%) were type C, and 2 patients (4%) were type E. The mean interval between primary operation and interview was 5.5 years. The incidences of growth retardation (<10 percentile of height/weight) were 39% and 21 % during the first 5 years after repairs, respectively. The incidences of dysphagia or gastroesophageal reflux and recurrent respiratory infections were 33% and 39 %, respectively. However, these problems were likely to improve as the children grew. The incidences of growth retardations (<10 percentile of height/weight) were 11% and 11% for the children more than five years postoperative. The incidences of dysphagia or gastroesophageal reflux and recurrent respiratory infections were 22% and 22%, respectively. Children with EA with or without TEF are faced with many obstacles. Close observation and adequate treatment for delayed postoperative complications are necessary to improve the quality of life for these children.
Lipoblastoma is a rare benign soft tissue tumor occurring in infancy and early childhood. It is characterized by fat lobules with varying degrees of maturity, multivaculoated lipoblasts, fibrocapillary networks and myxoid stroma. Lipoblastoma has a good prognosis with no metastases despite its potential for local invasion. From Jan, 1990 through April, 2007, 12 children underwent the operation for lipoblastoma, 7 boys and 5 girls, diagnosed at median 22 months (5~43 months). Median follow up was 6 year 7 months. Primary sites included back (n=5), intraabdominal (n=2) and one in each of buttock, chest wall, neck, nose and scalp. Tumors presented with a growing mass in 9 patients, abdominal distension in 2, and an incidental finding on chest radiography in one. Complete excisions were done in all patients. There was one recurrence in a patient with a scalp mass. After reoperation, he has been doing well without evidence of recurrence. Lipoblastoma has a favorable prognosis, but recurrence can occur even with complete excision. Regular follow up is necessary to detect recurrences.
Teratomas arising from totipotential primitive germ cell are composed of 2 or 3 germ cell layers. We reviewed the records of 166 children who underwent the operation for teratoma from Jan, 1990 through April, 2007. There were 40 boys and 126 girls (average age 6.93±5.83 years). Primary sites were ovary (n=88), sacrococcygeum (n=24), testis (n=16), retroperitoneum (n=16), mediastinum (n=8), brain (n=4), thymus (n=3) and a single tumor involved the adrenal gland, neck, middle ear, oropharynx, stomach, pelvis, omentum, chest wall and scalp. Teratomas were mature in 141 patients, and immature in 25. Six patients who had ovarian immature teratomas grade 2 or 3 with peritoneal gliomatosis underwent adjuvant chemotherapy. During follow up period, 6 mature teratomas recurred at sacrococcygeal area (n=1) and contralateral ovary (n=5). Five patients of them underwent reoperation and diagnosed as a mature teratoma, but one who had underwent a left salpingooophrectomy with right ovary cystectomy at initial operation was observed carefully. Teratomas were dominant in female patients and developed at various organs. Complete excision was needed for good prognosis. In case of immature teratoma, complete excision and appropriate chemotherapy according to grading can contribute to favorable results.
Adrenocortical tumors are very rare in children and the clinical course is not clearly understood. The aim of this study is to review the clinical characteristics and courses of pediatric adrenocortical tumors. The medical records of patients who underwent surgery for primary adrenal tumor at the Department of Surgery, Seoul National University hospital, from Jan. 1986 to Feb. 2006 were reviewed. There were 10 adrenocortical tumor patients; 5 had adrenocortical adenoma and 5 adrenocortical carcinoma. All of the adrenocortical adenomas presented as functioning tumors,
Pancreatic tumors in children are very rare but have a better prognosis compared with that in adult. Pediatric pancreatic tumors are more often benign and easier to resect. To evaluate the characteristics and prognosis, the records of 13 patients who underwent pancreatic resection, from June 1997 to May 2005, at Samsung Medical Center were reviewed. The mean follow up period was 48 months. The male to female ratio was 1: 1.6. Mean age was 10.3 years. Signs and symptoms included abdominal pain (7), abdominal palpable mass (5), jaundice (1), hypoglycemic (1), and non-specific GI symptoms (4). The commonly used diagnostic tools were CT and abdominal sonography. In addition, MRI, ERCP, EEG, and hormone test were also done when indicated. Surgical procedures included distal pancreatectomy (5), pylorus preserving pancreaticoduodenectomy (4), tumor excision (3), and subtotal pancreatectomy (1). Locations of lesions in pancreas were head (4), tail (5), and body and tail (4). Postoperative complications developed in 3 cases; postoperative ileus (1), wound problem (1), and pancreatitis (1). The pathologic diagnosis included solid-pseudopapillary tumor (6), congenital simple cyst (1), pancreatic duplication cyst (1), serous oligocystic adenoma (1), mucinous cystadenocarcinoma (1), rhabdomyosarcoma (1), insulinoma (1), and pancreatoblastoma (1). Three cases received adjuvant chemotherapy and radiotherapy. Overall survival rate was 81%. One patient with a mucinous cystadenocarcinoma died. In this study, pancreatic tumors in children were resectable in all patients and had good survival. Surgery of pancreatic tumors should be regarded as the gold standard of treatment and a good prognosis can be anticipated in most cases of benign and malignant tumors.
Liver tumors in children are rare, relatively complex, and encompass a broad spectrum of disease processes. This study reviews our experience of liver tumors during the last 10 years. Medical records of 36 cases of liver tumors?in children, treated at Samsung Medical Centers, from October 1994 to December 2005, were reviewed in this study. We analyzed disease characters and survival rates as a whole and by specific disease. The median age was 3.6 years. Male and female ratio was 1:1. The most common symptom was the palpable mass in 15 cases. Others were abdominal distension in 9 cases, jaundice in 2, vomiting in 2, weight loss in 2, and pubic hair growth in 1. CT or US and liver biopsy were performed for diagnosis. There were 28 malignant tumors: malignant rhabdoid tumor (1 case), hepatocellular carcinoma (3 cases), hemangioendothelioma type II (3 cases), angiosarcoma (1 case), and hepatoblastoma (20 cases). Eight tumors were benign; hepatic adenoma (1 case), focal nodular hyperplasia (2 cases), hemangioendothelioma type I (2 cases), mesenchymal hamartoma (3 cases). In this study the clinical characteristics were not different from the other reports. Liver transplantation was performed in 3 cases-1 with hepatoblastoma and 2 with hepatocelleular carcinoma. Accurate and early diagnosis, and individualized multi- modality therapeutic approaches might be important for better outcome.
Meckel's diverticulum is the most common congenital anomaly of gastrointestinal tract in children. The incidence of complicated Meckel's diverticulum is about 4%. The major complications of Meckel's diverticulum are bleeding, intussusception, obstruction and perforation. The aim of this study was to investigate the clinical manifestations and the role of laparoscopic surgery in complicated Meckel's diverticulum in children. We retrospectively reviewed the medical records of 19 patients with complicated Meckel's diverticulum who underwent operation at Asan Medical Center between Jan. 1990 and Apr. 2007. Male to female ratio was 11:8, and median age was 1 year (1 day-13 years). The most frequent symptom was hematochezia (68%), followed by irritability or abdominal pain (16%), vomiting (11%), and abdominal distension (5%). Two operative procedures were performed; small bowel resection with anastomosis (68%) and diverticulectomy (32%). The operation proven complications of the Meckel's diverticulum were bleeding (68%), intussusception (16%), perforation (11%) and obstruction (5%). Ectopic tissues found by postoperative pathologic examination were gastric (84%) and pancreatic (11%). Hospital stay after laparoscopic operation for bleeding Meckel's was 5 days (median) and average first postoperative feeding was 1.5 days. On the contrary, hospital stay for open surgery was 7 days and first feed was 3 days. In summary, the most common compliation of Meckel's diverticulum in children was bleeding and ectopic gastric tissues were present in 84%. Laparoscopic procedure seemed to be useful for diagnosis as well as for definitive treatment.
Trauma is one of the leading causes of death in children. Abdominal trauma is about 10% of all pediatric trauma. This study describes the sex and age distribution, injury mechanism, site of intraabdominal injury, management and mortality of children aged 16 years or less who suffered abdominal trauma. The hospital records of 63 patients treated for abdominal injury between March 1997 and February 2007 at the department of surgery, Inje University Pusan Paik Hospital, were analyzed retrospectively. The peak age of incidence was between 2 and 10 years (78%) and this report showed male predominance(2.7:1). The most common mechanism of blunt abdominal trauma was pedestrian traffic accident (49%). The most common injured organ was liver. More than Grade IV injury of liver and spleen comprised of 4(12%) and 5(24%), respectively. Fourteen cases (22%) had multiple organ injuries. Forty nine cases (78%) were managed nonoperatively. Three patients (4.8%) died, who had Grade IV liver injury, Grade IV spleen injury, and liver and spleen injury with combined inferior vena cava injury, respectively. All of the three mortality cases had operative management. In conclusion, the liver or spleen injury which was more than Grade 4 might lead to mortality in spite of operation, although many cases could be improved by nonoperative management.
Pediatric laparoscopic appendectomy is controversial particularly in complicated appendicitis. We evaluated the outcomes of laparoscopic appendectomy (LA) and open appendectomy (OA) in simple appendicitis and complicated appendicitis respectively. Since June 2004, initial LA has been our policy in all appendicitis including complicated ones. A total of 160 patients were included in this study, consisting of 80 OA (August 2001 . August 2003) and 80 LA (June 2004 . June 2006). We compared the operating time, the length of hospital stay, the length of antibiotics use, and the postoperative complications between LA and OA. In simple appendicitis (73), there were no differences between LA and OA. However in the 87 patients with complicated appendicitis, the operating time was longer in LA (64.8 min vs. 50.2 min) but the length of hospital stay was shorter in LA than OA (8.5 days vs. 9.6 days). There was one complication in simple appendicitis group and six in complicated appendicitis group (3 cases in LA, 3 cases in OA). There was no difference in the results of LA versus OA in simple appendicitis. Therefore for simple appendicitis, LA is recommended in consideration of the cosmetic effect (fewer scar). In complicated appendicitis, early discharge was an advantage and there were no differences in complications in LA despite a longer operative time. So we conclude LA can be considered as the first choice of treatment for all pediatric appendicitis including complicated appendicitis. To confirm our impressions, more well controlled randomized prospective studied need to be done.
Laparoscopic cholecystectomy has been increasingly used because of several advantages, less pain, better expectation for cosmesis (requires small incisions), and more rapid recovery compared with open cholecystectomy. Oral intake is tolerated on the day of operation or on the next. In this study, we evaluated the effectiveness and safety of laparoscopic cholecystectomy in children. Nine cases of laparoscopic cholecystectomy for acute and chronic cholecystitis in children were performed at Asan Medical Center between April 2002 and April 2004. Laparoscopic cholecystectomy was performed on a total of 10 patients, but one of them was excluded because of the simultaneous splenectomy for sickle cell anemia. Clinical presentation, operative findings, operation time, length of hospital stay, and postoperative complications were analyzed. Mean age was 10.4 (4–15) years, and only 3 of patients were less than 10 years. One patient was female. In 8 the diagnosis was calculous cholecystitis. Mild adhesions were found in 3 cases and intraoperative bile leakage in 2. There was no conversion to open surgery and there were no vascular, bowel, or bile duct injuries. Mean operation time was 82.2 (20–160) minutes ; mean length of hospital stay was 2.1 (1–3) day. There was no postoperative complication. Laparoscopic cholecystectomy in children was remarkably free of side effects and complications and had a short recovery time. Laparoscopic cholecystectomy for cholecystitis is considered to be a standard procedure in children.
Four children with solid and papillary epithelial neoplasm of the pancreas are reported. Three were girls. Mean age at operation was 12 years and 7 months (10-13 years). Clinical presentation included nausea, vomiting, and apalpable mass. One had hemoperitoneum due to tumor rupture. In two cases, tumors were in the body of the pancreas, and one the body and tail, and in one,the tail. Mean diameter of the tumors was 10.8 cm (8-15cm). Surgical procedures were distal pancreatectomy and splenectomy in 2 cases, distal pancreatectomy in one, and subtotal pancreatectomy and splenectomy in one. Mean follow-up period was 61 months (6-121 months). Three patients are still alive without any recurrence. However, in the one case of ruptured tumor, portal vein thrombosis and liver metastasis developed after subtotal pancreatectomy and splenectomy during the course of postoperative adjuvant chemotherapy.
Inguinal hernia is one of the most common surgical diseases in pediatric patients. But the management of the side opposite the clinically apparent inguinal hernia, the “silent side” is controversial. Four hundred fifty-eight cases of pediatric inguinal hernias, operated by one pediatric surgeon at the Divisionof Pediatric Surgery, Department of Surgery, Chonbuk National University Hospital from January 1998 to December 2002, were reviewed retrospectively to determine the characteristics and significances of the silk-glove test on the side opposite the clinically apparent inguinal hernia. Males were preponderant as 2.8:1. Allhernias were of the indirect type and were repaired by high ligation of the sac. There were 238 (52.0%) right sided hernias, 160 (35.0%) were on the left and 60 (13.0%) were bilateral. The number of patients with a positive silk-glove sign on the contralateral side was 158(39.7%), and 133 of these had a contralateral patent processus vaginalis. Positive predictive value of Silk-glove test was 84.2% (133/158). The silk-glove test is a simple, safe, and relatively accurate method for contralateral exploration in the unilateral inguinal hernias in children.
Neuroblastoma treatment remains challenging, but has been advanced by the establishment of clinical and biological variables that determine prognostic risks. Initially, stage and age were the prime determinants of survival used in clinical practice. Risk-based therapy currently is the hallmark of neuroblastoma treatment. This study reviewed the results of neuroblastoma in one center. Sixty-three patients with neuroblastoma were treated primarily at our institution from 1989 to 2003. All patients were graded according to the International Neuroblastoma Staging System (INSS) at diagnosis. There were 37 boys and 26 girls. The median age was 2.14 years (range, 33 days-10.2years). The primary site was the adrenal gland in 47, dumbbell shape extended into spinal canal in 6, retroperitoneum in 5, mediastinum in 3, and other sites in 2. The probability of 5-year overall survival (OS) and event free survival (EFS) were 46.7% and 44.2% by Kaplan-Meier method. According to INSS, there were stage 1 in 2, stage 2 in 5, stage 3 in 12, stage 4 in 42, and stage 4s in 2. There were statistically significant differences in the survival rates between patients with stage1, 2 and stage 3, 4(p<0.05). For the stage 3 and 4, the extent of surgical resection determined from the operative records and pathologic reports assessed extent of surgical resection as complete resection, no visible tumor (CR, n=17); minimal residual, visible tumor less than 5% (MR, n=15); partial resection, more residual tumor than MR (PR, n=11). The 5-year OS rate was 57.8, 51.4, and 13.6% for CR, MR, and PR. There is a trend toward higher OS with achieving the completeness of resection (p<0.05). We conclude that age and stage at diagnosis are prognostic factors, and complete excision of the primary tumor can provide better prognosis for patients with stage 3 and 4 neuroblastoma.
Ulcerative colitis, one of the inflammatory bowel disease, is primarily managed medically with combinations of 5-ASA and steroids. However, this chronic disease requires surgical management if symptoms persist or complications develop despite medical management. The clinical course, the indications and outcome for surgical management of pediatric ulcerative colitis patients were studied from medical records retrospectively. Twenty-one patients under the age of 15 who were endoscopically diagnosed with ulcerative colitis at the Seoul National University Children's Hospital between January, 1988 and January, 2003 were subjected to the study. Mean follow up period was 3 years and 10 months. The mean age was 10.3 years old. All patients received medical management primarily after diagnosis and 8 patients (38%) eventually required surgical management. Of 13 patients who received medical management only, 7 patients (53%) showed remission, 4 patients are still on medical management, and 2 patients expired due to congenital immune deficiency and hepatic failure owing to sclerosing cholangitis respectively. In 8 patients who received surgical management, 1 patient underwent surgery due to sigmoid colon perforation and 7 patients due to intractability of medical management. The perforated case received colon segmental resection and the other 7 patients recieved total protocolectomy with ileal pouch-anal anastomosis. One patient expired postoperatively due to pneumonia and sepsis. One patient is still on medical management because of mild persistent hematochezia after surgery. The other operated patients are showing good prognosis without any management. Pediatric ulcerative colitis patients can be surgically managed if the patient is intractable to medical management or if complications such as perforation is present. Total protocolectomy & ileal pouch-anal anastomosis is thought to be the adequate surgical method.
The purpose of this study is to review the operative management and outcome of operation for Crohn's disease. The medical records of 17 patients who underwent operations due to Crohn's disease at Seoul National University Children's Hospital from January of 1988 to June of 2005 were reviewed and retrospective study was carried out. The male-to-female ratio was 1.8: 1. The median age at the onset of symptom and the time of diagnosis was 9 years 6 months and 11 years 6 months respectively. The median interval time from diagnosis to operation was 2 years and 1 month (0 month~8 years). Ileocolic or ileocecal region was the most common site of involvement. The indications of operation were intractable symptoms (8 cases) and obstruction or stricture (7 cases). The median postoperative hospitalized days were 14.4 days (8~35 days). Five patients (29%) experienced postoperative complications. Symptom free state or symptom relief was observed in 11 cases after surgery and 6 cases had wax and wane course of aggravation and improvement. In pediatric Crohn's disease patients who present with intractable symptoms despite medical treatment or develop surgical complications, symptom free state or symptom relief can be achieved by minimal resection of involved lesion.
Primary liver tumors are uncommon in childhood, with a relative frequency of 3% of childhood tumors. Seventy three cases of pediatric primary liver tumors which were operated on at single institution between 1986 and 2002 were reviewed. There were 37 cases of hepatoblastoma, 11 hepatocellular carcinomas, 6 undifferentiated (embryonal) sarcomas, and 1 mixed germ-cell tumor in malignancies. Benign tumors constitute only 24.6% of liver tumors, including 7 hemangioendotheliomas, 5 mesenchymal hamartomas, 3 congenital cysts, and one each with focal nodular hyperplasia and hemangioma. The common presenting clinical features were abdominal mass or abdominal distension. Anatomical hepatic resections were carried out in 38 cases, and non anatomical resections in 34 cases. One patient died of a direct result of hepatic resection(1.4%), and complication rate was 16.4%.
Solid pseudopapillary tumor of pancreas in children is a tumor with low malignant potentiality, and is rarely associated with distant metastasis. A 13-year-old girl was hospitalized because of abdominal pain of one week duration. Abdominal CT revealed not only a 12×6cm sized mass at the pancreatic body and tail but also a 1cm sized mass in left lobe of the liver. The patient underwent a near-total pancreatectomy and tumorectomy of the liver. A solid pseudopapillary tumor with liver metastasis was confirmed by pathology. She has undergone 13 courses of chemotherapy and has been well for 13 months without any sign of recurrence.
A 12-year-old boy with severe periumbilical pain visited the emergency room. Physical examination, abdominal ultrasonography, colonoscopy and CT, identified a lesion of sigmoid colon. Endoscopic biopsy showed a signet ring cell carcinoma of the sigmoid colon. On explorative laparotomy, cancer invasions of the adjacent structures and metastases on peritoneal wall were noticed. We performed palliative loop-ileostomy. He underwent chemotherapy and radiotherapy for 3 months. The second case was a 16-year-old boy with abdominal pain and hematochezia, transferred to our hospital with the diagnosis of acute appendicitis with periappendiceal abscess. Although he underwent appendectomy, the abdominal pain persisted. Digital rectal examination revealed a lumen-obstructing fungating mass in the rectum. Endoscopic biopsy revealed a adenocarcinoma. Cancer invasion of the adjacent structures and metastases involving the mesentery of the small intestine were found at laparotomy. A palliative procedure, a Hartmann's operation and end-colostomy at the sigmoid colon were performed. The patient died 8 month later due to pneumonia and sepsis. Chemotherapy was not applied.
Appendectomy is the most common emergency surgical operation in children. The laparoscopic treatment of pediatric appendicitis is controversial, particularly in complicated cases. The purpose of this study is to evaluate laparoscopic appendectomy (LA) and open appendectomy (OA) for simple and perforated appendicitis (SA, PA) in children. A total of 188 patients, operated from January 1992 to September 2003, were reviewed. Ninety-one patients underwent OA (65 SA and 26 PA) and 97 had LA ( 67 SA, 30 PA). There was one conversion of LA to OA in PA. Operative time for LA was longer for OA in PA (55.8 vs. 45.7 min; p=0.0467). Recovery of bowel movement, diet starting time, length of hospital stay for LA were significantly shorter than those for OA. Postoperative complication rate was not different between LA and OA in each group. Laparoscopic appendectomy is a safe and effective method for both simple and perforated appendicitis.
Intestinal obstruction secondary to intraabdominal adhesion is a well-known postoperative complication occurring after appendectomy. The aim of this study was to measure the incidence and clinical manifestations of mechanical intestinal obstruction after appendectomy for perforated appendicitis. We reviewed all of the children (age <16 years) who had been treated for appendicitis at Asan Medical Center between January 1996 and December 2001. Inclusion criterion included either gross or microscopic evidence of appendiceal perforation. Exclusion criteria were interval appendectomy, and patients immune compromised by chemotherapy. Associations of intestinal obstruction with age, sex, operation time, and use of peritoneal drains were analyzed. Four hundred and sixty two open appendectomies for appendicitis were performed at our department. One hundred and seventeen children were treated for perforated appendicitis (78 boys, 39 girls). The mean age was 8.9 years (range 1.5 to 14.8 years). There were no deaths. Eight patients were readmitted due to intestinal obstruction, but there was no readmission due to intestinal obstruction in patients with non-perforated appendicitis. The interval between appendectomy and intestinal obstruction varied from 12 days to 2 year 7 months. Four patients needed laparotomies. In three of four, only adhesiolysis was performed. One child needed small bowel resection combined with adhesiolysis. There was no significant association between age or sex and the development of intestinal obstruction. This was no association with operative time or use of peritoneal drain. Patients who required appendectomy for perforated appendicitis have a higher incidence of postoperative intestinal obstruction than those with nonperforated appendicitis. For the patients with perforated appendicitis, careful operative procedures as well as pre and postoperative managements are required to reduce adhesions and subsequent bowel obstruction.
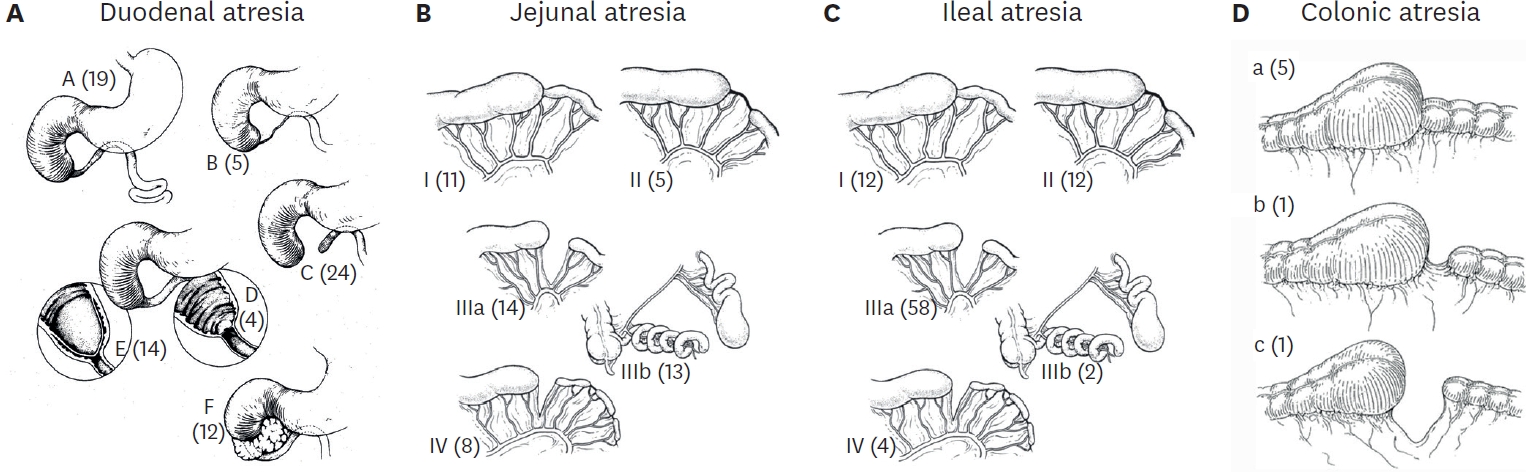
Midgut volvulus secondary to intestinal malrotation usually presents within the first month of life. Diagnostic delay may result in midgut infarction and mortality. In this retrospective study, we review seventeen cases of midgut volvulus to assess the importance of early recognition for midgut volvulus in pediatric patients of any age.. These patients were diagnosed as having a midgut volvulus by operation at Ewha Womans University Hospital. Eleven patients (64.7 %) were less than 1 month of age, and fifteen were boys (88.2 %). The mean gestational age was 38.3 weeks and the birth weight was 3.1 kg. Eight patients (47.1 %) had one or more combined anomalies such as heart malformation, brain ischemia, Down's syndrome or duodenal atresia. Vomiting was the most common symptom. Only thirteen patients underwent preoperative diagnostic procedures; 13 abdominal sonography demonstrated the whirlpool sign in 8 patients, upper gastrointestinal tract roentgenography showed a cork-screw pattern in 7 patients, and barium enema or small bowel series demonstrated positive findings in 7 patients. A Ladd's procedure was was formed on all patients.. There was no mortality or severe morbidity such as short bowel syndrome. Midgut volvulus should be included in the differential diagnosis in any infant or child who presents with the symptoms of acute abdomen, especially with vomiting.
The laparoscopic splenectomy (LS) became popular over the last 10 years. The advantage of LS over open splenectomy (OS) includes short hospital stay, improved cosmesis, less development of postoperative intestinal ileus, and less analgesics required. The purpose of this study is to evaluate the outcome of LS at Asan Medical Center from January 1999 to January 2003. The records of 14 consequent children who underwent splenectomy were reviewed retrospectively. Patients characteristics, morbidity, mortality, operative time, blood loss, and hospital stay were analyzed., Seven patients age 5 to 15 years underwent LS under the indications: idiopathic thrombocytic purpura (ITP, n=3), hereditary spherocytosis (n=3), and myelodysplastic syndrome (n=1). Seven patients, age 7 to 16 years, underwent OS during the same period for ITP (n=7). Median operative time was 120 minutes (80 to 170 mins.) in OS, and 270 minutes (110 to 480 mins.) in LS (p<0.05). Median length of hospital stay was 6 days (3 to 8) in OS, and 4 days (3 to 6) in LS (p>0.05). Median splenic length was 12.0 cm (9.2 to 18.0) in OS, 14.0 cm (10.0 to 19.5) (p>0.05). Accessory spleens were identified in 3 of 7 LS and 1 of 7 OS cases. In the LS group, there was no conversion to open surgery. Two patients in LS required blood transfusion postoperatively. LS in children can be performed as effectively and safely as OS.
Continuous Ambulatory Peritoneal Dialysis (CAPD) has now become an established form of renal replacement therapy in children. Despite of technical improvements, there are various complications in CAPD. We reviewed medical records of children who received CAPD at Seoul National University Children's Hospital in the period between May 1991 and June 2002. Ninety-three procedures of CAPD catheter insertion in 70 patients were included in this study. Complication rate was 64.5%, and CAPD catheter related peritonitis was most common. In conclusion, CAPD catheter related peritonitis develops in considerable number of pediatric patients. Although the peritonitis could be treated with empirical antibiotics therapy, further investigation to prevent complication is required.

