We describe our experience in managing congenital diaphragmatic hernia (CDH) in neonates.
From February 1995 to July 2014, 64 neonates diagnosed with CDH were managed. The medical records of these neonates were retrospectively reviewed.
There were 40 males and 24 females. CDH was on the left side in 44 cases (68.8%), on the right side in 19 cases (29.7%) and bilateral in 1 case (1.6%). Forty-six patients (71.9%) received surgical repair of the hernia while 18 patients (28.1%) died prior to surgery. The timing of surgery was mean 7.0 days after birth. Extracorporeal membrane oxygenation was used in six patients (9.4%), High-frequency oscillation ventilation was used in 49 patients (76.6%), and nitric oxide was used in 42 patients (65.6%). Thirty-three cases (71.7%) of CDH repair were done via open laparotomy, 3 cases (6.6%) by open thoracotomy. and minimally invasive thoracoscopic repair was done in 10 cases (21.7%). Ten cases (21.8%) required patch repair of the CDH. Barotrauma and pneumothorax of the contralateral lung was seen in 16 cases, leading to death in 15 of these cases. The overall survival rate was 48.4% (31/64) and postoperative survival rate was 67.4% (31/46). When all patients are divided into 3 groups by era and analyzed by logistic regression models, the mortality outcome of recent era (2009–2014) was significantly better than that of intermediate era (2002–2008) (29% vs. 71%, p=0.006) and tended to be better than that of past era (1995–2001) (42% vs. 71%, p=0.062).
The overall survival of neonates with CDH at our center has improved over the last two decades. Sixty-four neonates with CDH were managed at a single center and their overall survival was 48.4%. The risk factors for mortality include the occurrence of pneumothorax and right side lesions.
Congenital esophageal stenosis (CES) is a rare disease that has been reported to occur once in every 25,000 to 50,000 births. According to its etiology, CES is divided into 3 subtypes, tracheobronchial remnants (TBR), fibromuscular hypertrophy (FMH) and membranous diaphragm (MD). Symptoms begin at the weaning period and the introduction of solid food around 6 months with dysphagia and vomiting. Esophagography is first screening test and endoscopic ultrasonography plays important roles to diagnose subtypes deciding therapeutic plan. TBRs were generally treated with surgical resection and end-to-end anasotomosis, whereas FMH and MD had good response rate to endoscopic or radiologic guided dilatation. This article reviews the literature on the etiology, clinical course, diagnosis and management of CES including recent opinion.
It has been known that extramedullary hematopoiesis occurring after birth can be developed in various diseases, and it is often found in hematologic diseases. Among these, congenital dyserythropoietic anemia is a rare disease characterized with increase of ineffective hematopoiesis and morphological abnormalities of erythroblasts. In congenital dyserythropoietic anemia, extramedullary hematopoiesis is very rare and only a few cases have been reported. Although treatment is not required if there is no symptom in extramedullary hematopoiesis, surgery or radiation therapy is effective in case that there is symptom or unresponsive anemia despite blood transfusion. This case report is about surgical treatment for extramedullary hematopoiesis in 23-year-old patients diagnosed of congenital dyserythropoietic anemia.
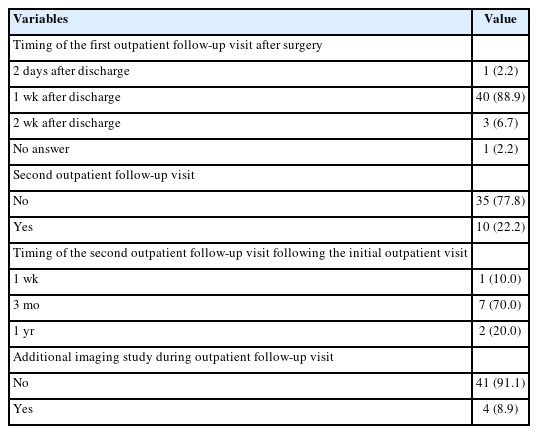
This is a survey on congenital posterolateral diaphragmatic hernia, conducted by Korean Association of Pediatric Surgeons (KAPS). A registration form for each patient during the 5-year period between 2010 and 2014 and a questionnaire were sent to each member. Twenty-six members in 16 institutions returned completed forms. Total patients were 219. Prenatal diagnoses were done in 181 cases (82.6%). Preoperative mortality was 11.4%. Minimal invasive surgery was done in 61 cases (31.8%). Risk factors related with death were Apgar score, oxygenation index, preoperative pH and bicarbonate, O2 saturation, the presence of hernia sac, and the size of defect. The neonatal survival and 1-year survival of total patients were 77.6% and 75.3%.
Congenital duodenal obstruction is a one of the emergent surgical conditions in neonates. Almost of them were diagnosed with double-bubble sign in prenatal ultrasonography. However, partial obstruction caused from duodenal web could be overlooked. We reported a duodenal web in early childhood. A three-year-old girl visited at our pediatric clinic for constipation. She had been showed non-bilious vomiting after weaning meal since 6 months old of her age, but her weight was relevant for 50-75 percentile of growth curve. Barium enema was initially checked, but any abnormal finding was not found. We noticed the severely distended stomach and 1st portion of duodenum. Upper gastrointestinal series revealed partial obstruction in 2nd portion of duodenum. After laparotomy, we found the transitional zone of duodenum and identified a duodenal web via duodenotomy. We performed duodeno-duodenostomy without any injury of ampulla of Vater. She was recovered uneventfully. During 6 months after operation, she does well without any gastrointestinal symptoms or signs, such as vomiting or constipation.
Experimental tracheal ligation (TL) has been shown to reverse the pulmonary hypoplasia associated with congenital diaphragmatic hernia (CDH) and to normalize gas exchange. The purpose of this study was to determine whether the TL would correct the surfactant deficiency present in the fetal rabbit model of CDH by using lamellar body count. Lamellar bodies are synthesized and secreted by the type II pneumocytes of fetal lung. The phospholipids present in these bodies constitute the major component of pulmonary surfactant. Twenty-one pregnant New Zealand rabbits underwent hysterotomy and fetal surgery on gestational day 24. Two fetuses of each pregnant rabbit were operated. In the fetus of one end of bicornuate uterus, left DH was created by excision of fetal diaphragm through open thoracotomy (DH Group). In the fetus of the other end of bicornuate uterus, left DH and TL were created (TL Group). The fetuses were delivered by Cesarean section on gestational day 31. Fourteen in control group, 12 in the DH group and 13 in TL group were born alive. En bloc excision of lungs, bronchi and trachea was done in all newborn rabbits. A five Fr catheter was inserted through trachea and repeated irrigations with 10 cc normal saline were done. The irrigated fluid was centrifuged at 280 xg for 5 minutes and the lamellar bodies were counted with the upper level fluid in platelet channel of electronic cell counter. The average lamellar body counts were 37.1 ± 14.2 × 103/µL in control group, 11.5 ± 4.4 × 103/#x00B5;L in DH group, and 6.5± 0.9 × 103/#x00B5;L in TL group. Lamellar body count in DH group was lower than in control group and did not increase after TL. This study shows TL has no therapeutic effect on decreased surfactant level of CDH and the pregnant rabbit is appropriate for the animal model of CDH.
Extracorporeal membrane oxygenation (ECMO) has been utilized in congenital diaphragmatic hernia (CDH) patients with severe respiratory failure unresponsive to conventional medical treatment. We retrospectively reviewed 12 CDH patients who were treated using ECMO in our center between April 2008 and February 2011. The pre ECMO and on ECMO variables analyzed included gestational age, sex, birth weight, age at the time of ECMO cannulation, arterial blood gas analysis results, CDH location, timing of CDH repair operation, complications and survival. There were 9 boys and 3 girls. All patients were prenatally diagnosed. Mean gestational age was 38.8 ± 1.7 weeks and mean birth weight was 3031 ± 499 gram. Mean age at the time of ECMO cannulation was 29.9 ± 28.9 hours. There were 4 patients who survived. Survivors showed higher 5 min Apgar scores (8.25 ± 0.96 vs. 7.00 ± 1.20,
This study was aimed to evaluate associated congenital anomalies in the patients with esophageal atresia with tracheoesophageal fistula (EA/TEF). Forty-two neonates with the diagnosis of EA/TEF treated over a 10 year period in a single institution were included in this study. The demography of EA/TEF was analyzed. Major associated anomalies including vertebral, anal, cardiac, renal, limb, neurologic and chromosome were reviewed and categorized. Males were slightly more dominant than females (1.47:1) and all patients had Gross type C EA/TEF. Only 19% of the patients had solitary EA/TEF without associated anomalies. Cardiac anomalies were the most common associated congenital anomaly in patients with EA/TEF (73.8%). But 47.6% were cured spontaneously or did not affect patients' life. Atrial septal defect (ASD) was the most common cardiac anomaly followed by patent ductus arteriosus (PDA) and ventricular septal defect (VSD). Among gastrointestinal anomalies (23.8%), anorectal malformations were the most frequent, 70% Vertebral and limb abnormalities accounted for 11.9% and urogenital malformations 9.5% of the anomalies in patients with EA/TEF. VACTERL associated anomalies were 23.8% and 4.8% had full VACTERL. Almost 12% of EA/TEF had neurologic anomalies. Patients with EA/TEF require preoperative evaluation including neurologic evaluation to detect anomalies not related to VACTERL. Though associated cardiac anomaly occurred in 73.8% of patients in our study, only 21.42% needed surgical correction. The authors suggesrs further studies with large numbers of patients with EA/TEF.
Congenital diaphragmatic disease is one of the common major congenital anomalies, and its mortality remained still high despite recent medical advances. The aim of this study is to examine the clinical characteristics of congenital diaphragmatic diseases. A total of 39 patients with congenital diaphragmatic disease that underwent surgery from January, 1997 to December, 2009 at Pusan National University Hospital were included in this study. Medical records were retrospectively reviewed. The male to female ratio was 30:9. Six out of 39 cases died (NS) before surgery, 17 patients had Bochdalek's hernia (BH), 11 patients hiatus hernia (HH), 4 diaphragmatic eventration (DE), and 1 Morgagni hernia (MH). There were no differences in mean birth weight and mean gestational age. NS (83.3%). BH (35.3%) was diagnosed more frequently than other diseases in the prenatal period. Three patients (17.6%) of BH expired due to pulmonary hypoplasia and 1 patient had co-existing congenital heart disease. BH was diagnosed more frequently in the prenatal stage and had a higher motality rate than other conditions. Therefore, BH needs to be concentrated more than other anomalies.
Sialoblastoma is a rare tumor of salivary gland origin, developing in the fetal or neonatal period. Most tumors arise in parotid gland, and rarely in submandibular gland. Because of its rare incidence, diagnosis of the sialoblastoma in head and neck tumors of children is not easy. The case of a congenital submandibular gland sialoblastoma is presented. A neonate was transferred right after birth due to a submandibular mass. CT scan showed a lobulating mass located posterior to the left submandibular gland, suggesting neurogenic tumor or myofibroma. The tumor was excised easily after division of a duct-like structure connecting with the submandibular gland. The microscopic findings showed the basaloid cells and ductules forming cellular nests, separated by thin fibrous tissue. Immunohistochemical staining was positive for cytokeratin, vimentin and Ki-67, which was consistent with sialoblastoma.
A vitelline duct (VD) anomaly is a relatively common congenital abnormality of the umbilical area. The anomalies include patent vitelline duct (PVD), cyst, fistula or sinus. The incidence is approximately 2% of the populations, but development of symptoms is rare. Recently, we experienced two cases; PVD accompanied by a smallomphalocele and intestinal volvulus due to mesenteric band between Meckel's diverticulum and the mesentery. Thereafter,we evaluated the data of vitelline duct anomalies for 27 years. From 1980 to 2006, 18 cases of VD anomalies were reviewed based on the hospital records retrospectively. There were 15 boys and 3 girls and age ranged from 2 days to 15 years. Among the 18 cases, 15 cases were symptomatic and consisted of Meckel's diverticulum (10 cases), PVD (4 cases) and umbilical polyp (1 case). Three asymptomatic cases of Meckel's diverticulum were found incidentally were and were observed without resection. Ten cases of Meckel's diverticulum were presented with intestinal bleedings (4 cases), intestinal obstructions (5 cases) and perforation (1 case). Wedge resections and segmental resections of ileum were performed in 8 patients and 2 patients, respectively. Postoperative complications were adhesive ileus (1 case) and wound seroma (1 case). Small omphaloceles were accompanied in two of 4 PVD patients. There was 1 small omphalocele case which was accompanied by a prolapse of ileum. In summary, VD anomalies were more common in male and more than half of them were found in patients less than 1 year of age. PVD was diagnosed most frequently in neonates. Meckel's diverticulum presented with intestinal obstruction more frequently than bleeding.
There are considerable controversies in the management of congenital diaphragmatic hernia. By 1997, early operation, routine chest tube on the ipsilateral side and maintainingrespiratory alkalosis by hyperventilation were our principles (period I). With a transition period from 1998 to 1999, delayed operation with sufficient resuscitation, without routine chest tube, and permissive hypercapnia were adopted as our practice. High frequency oscillatory ventilation (HFOV) and nitric oxide (NO) were applied, if necessary, since year 2000(period II). Sixty-seven cases of neonatal Bochdalek hernia from 1989 to 2005 were reviewed retrospectively. There were 33 and 34 cases in period I and II, respectively. The neonatal survival rates were 60.6 % and 73.5 %, respectively, but the difference was not significant. In period I, prematurity, low birth weight, prenatal diagnosis, inborn, and associated anomalies were considered as the significant poor prognostic factors, all of which were converted to nonsignificant in period II. In summary, improved survival was not observed in later period. The factors considered to be significant for poor prognosis were converted to be nonsignificant after change of the management principle. Therefore, we recommend delayed operation after sufficient period of stabilization and the avoidance of the routine insertion of chest tube. The validity of NO and HFOV needs further investigation.
This is a survey on congenital posterolateral diaphragmatic hernia, conducted by the Korean Association of Pediatric Surgeons(KAPS). A registration form for each patient during the 5-year-period between 1998 and 2002 and a questionaire were sent to each member. Twenty-ninemembers in 22 institutions returned completed forms. The average number of patients per surgeon was 1.4 cases a year. The male to female ratio was 1.64: 1, and annual incidencewas 1/14,522 live births. In this review, factors influencing survival in congenital posterolateral diaphragmatic hernia were age at admission, birth weight, time of antenatal diagnosis, birth place, Apgar score, onset time of symptoms and signs, preoperative cardiopulmonary resuscitation, associated anomalies of themusculoskeletal system, central nervous system, or chromosomes, preoperative stabilization, levels of preoperative FiO2, pH, and AaDO2, perioperative complications, bilaterality of defect, size of the defect, and presence or absence of hernia sac.
Chronic duodenal obstruction related to a congenital web is a rare anomaly that is sometimes difficult to diagnose preoperatively. A case of partial duodenal obstruction along with a foreign body by a congenital duodenal web in a 10-year-old girl is presented. She has had one year history of intermittent epigastric discomfort without nausea, vomiting and growth retardation. The studies including UGI series and gastroduodenoscopy disclosed a perforated web in the 2nd portion of the duodenum and a dark go stone just proximal to the web. Via a longitudinal duodenotomy across the web, the web was partly excised with preservation of ampulla of Vater and the duodenum was closed in transverse fashion. The aperture of ampulla of Vater was located at 7 o'clock direction of posterior surface of the duodenal web. This particular case reminds clinicians to consider a duodenal web in a youngster presenting with a longstanding foreign body in the duodenum as one of the underlying pathologies.
Slide tracheoplasty, as a treatment for congenital tracheal stenosis, has been recently reported to have good results and quite a number of advantages as compared with conventional tracheoplasties. The aim of this study is to report a new surgical technique modified from the slide tracheoplasty, “the slide cricotracheoplasty” for the congenital cricotracheal stenosis. A girl was born by Cesarean section and the diagnosis of esophageal atresia (Gross type C) and cricotracheal stenosis (30% of total length of trachea) was established. Esophageal atresia was successfully corrected at the 8th day of life. At the 31st day of life, corrective surgery for congenital cricotracheal stenosis, the slide cricotracheoplasty, was performed with success. Slide cricotracheoplasty is almost the same procedure as slide tracheoplasty except for two technical features. First the cricoid cartilage was split on its anterior surface. Second the split cricoid cartilage was fixed to pre vertebral fascia to maintain enough space to accommodate the sliding caudal segment of trachea because of the stiffness of the cricoid cartilage. We believe that the sliding cricotracheoplasty is a new surgical technique for congenital cricotracheal stenosis that has similar results and advantages as the sliding tracheoplasty.
Congenital diaphragmatic hernia (CDH) in the past was considered a surgical emergency requiring immediate operation. Several groups now advocate preoperative stabilization and delayed surgery. The treatment strategy for CDH in this institution is delayed surgery after preoperative stabilization. The aim of this study was to evaluate the results of delayed surgery. A retrospective review of 16 neonates with CDH was performed. Surfactant, conventional mechanical ventilation, high frequency oscillation, and nitric oxide were utilized for preoperative stabilization as necessary. The difference in outcome between two groups differentiated by the duration of the preoperative stabilization periods with mechanical ventilation (≤ 8 hours and >8 hours) was determined. Chi-square test was used to analyze the data. There were 7 right-sided hernias and 9 left. The average duration of stabilization was 32.4 hours. Hepatic herniation through the defect was found in 6 cases and all died. The most common postoperative complication was pneumothorax. The mortality rate of the right side hernia was higher than the left (85.7% vs. 33.3%, p=0.036). Mortality rate of the group (N=8) whose preoperative stabilization period was 8 hours or less was better than that (N=6) whose preoperative stabilization period was more than 8 hours (25.0% vs. 83.3%, p=0.031). The overall mortality rate was 56.3%. The better prognosis was noticed in left side hernia, no liver herniation, or shorter preoperative stabilization period.
Congenital esophageal stenosis (CES) is a narrowing of the esophageal lumen from birth. Three types of CES have been described; tracheobronchial remnants (TBR), membranous web (MW), and fibromuscular stenosis (FMS). We reviewed the clinical features and the surgical outcome of 14 patients, pathologically confirmed as CES. Nine patients had TBR, 3 FMS, and 2 MVV. The mean age at operation was 3.8 years. Five patients were boys and 9 girls. Four patients had other congenital anomalies. Segmental resection of the lesion and end to end anastomosis was utilized in all cases except one who underwent myotomy. The stenotic segment was located at the distal esophagus in all patients. There were 8 complications in 6 patients, but no mortality. The mean follow-up period was 68 months. There were no feeding problems but 3 patients had minor gastroesophageal reflux. Our result indicates that segmental resection and anastomosis is a satisfactory surgical procedure in the management of CES.
Neurocristopathy is characterized as having a common origin in aberrant neural crest development. Congenital central hypoventilation syndrome (Ondine's curse) is characterized by marked depression of respiratory drive during sleep and normal ventilation while awake because of no response to both hypercapnea and hypoxia. The girl was full-term, weighing 3020 grams. The girl had poor respiratory effort at birth, but improved with oxygen supply and stimulation. abdominal distention and calcification were noted. During laparotomy transitional zone was found at distal jejunum; a jejunostomy was constructed. Numerous attempts at extubation failed because of apnea. The results of an apnea work-up, including brain sonography, echocardiogram, were normal. The girl died of sepsis at 37 days of age. para-aortic ganglioneuroblastoma was found on autopsy. We experienced a newborn with congenital central hypoventilation syndrome, Hirschsprung's disease and congenital ganglioneuroblastoma representative of neurocristopathy.
Congenital afibrinogenemia is a rare disorder that refers to a congenital lack of production of fibrinogen, a key component of the hemostatic system. Bleeding manifestations of congenital afibrinogenemia vary in severity from mild to catastrophic. This is a case report of splenic rupture occurred in an eight-year-old boy with congenital afibrinogenemia. Nonoperative treatment with cryoprecipitate and virally inactivated, purified fibrinogen concentrates successfully avoided splenectomy.
Although diaphragmatic eventration in newborn infants is generally regarded as a rare condition, the need for accurate diagnosis and appropriate intervention according to the etiological factors is well known. Recently the authors experienced five consecutive cases of diaphragmatic eventration below the age of two months(one to 55 days) requiring surgery. All were in males, and were left sided. Respiratory symptoms were present in 4 patients, and one patient showed inability to gain weight. Diaphragms were elevated to the level of the third to fifth intercostal spaces. Diaphragmatic plication through the abdomen gave excellent results. There was no postoperative mortality.
Seventy neonates with congenital intestinal atresia and stenosis who were treated at pediatric surgical service, Hanyang University Hospital from September 1979 to December 1996 were analyzed retrospectively. The lesion occurred in 27 cases at the duodenum, in 26 cases at the jejunum, in 13 cases at the ileum and in 2 cases at the pylorus and colon each. There were 10 multiple atresias and 7 apple-peel anomaly cases. The atresia predominated over the stenosis by the ratio of 4 : 1. Male to female ratio was 1.3 : 1. The average gestational age was 38 weeks, and the average birth weight was 2,754 grams. Though 22.9 % were borne prematurely and 34.3 % had low birth weight, 92.3 % of them had a weight appropriate for gestational age. Polyhydramnios(40 %) was more frequently observed in duodenal and jejunal atresia while microcolon in ileal atresia(58.3 %). Weight loss and electrolyte imbalance occurred more frequently in the duodenal stenosis cases because of delayed diagnosis. Twenty(55.6 %) of 37 jejunoileal atresia cases had evidence of intrauterine vascular accident: 4 intrauterine intussusception, 3 intrauterine volvulus and 3 strangulated intestine in gastroschisis, and 10 cases of intrauterine peritonitis. There were one or more associated anomalies in 45 patients(64.3 %). Preoperatively proximal loop volvulus developed in 3 cases and proximal loop perforation in 5 cases and one case each of distal loop perforation, duodenal perforation and midgllt volvulus occurred in the jejunoileal atresia. Overall mortality rate was 20 %.
The anatomical variations of the external genitalia including the hymen were observed prospectively in 1,500 female infants born between March, 1992 and July, 1992 at the Taegu Fatima Hospital. Careful inspection of the external genitalia was done within 24 hours after birth, and abnormal findings photographed. Almost all hymenal tissue appeared to be redundant. The hymen was annulus in 89.1 % of patients. Ninteen point nine percent had a central orifice and the remainder a ventral orifice. External ridges, intravaginal ridges, and clefts were present in 71.5 %, 50.7 % and 40.5 %, respectively. Congenital anomalies of the external genitalia were found in 20 patients(1.4 %). There were sixteen cases of hymenal cysts, two hymenal polyps, one imperforate hymen, and one Skene's duct cyst. Seven of the 16 hymenal cysts with stalks were excised and those without stalk were aspirated. Hymenal polyps were excised. Imperforate hymen was incised and drained, and Skene's duct cyst was aspirated successfully. The surgical procedure were done without anesthesia, and the results have been good. In conclusion, routine physical examination of the female newborn infant detects frequent developmental anomalies. The significance of those anomalies will be clarified after longitudinal long-term followup studies.
Pulmonary sequestration is a complex anomaly involving the pulmonary parenchymal tissue and its vasculature. It presents as a cystic mass of nonfunctional lung tissue without communication with the tracheobronchial system. Usually, it receives blood supply from anomalous systemic vessels. Therefore, preoperative diagnosis of the pulmonary sequestration is difficult, especially when it is located in the abdomen and combined with congenital cystic adenomatoid malformation (CCAM). We encountered such a mass(CCAM type 2) detected prenatally by ultrasonography. It was a kidney bean shaped, pinkish mass straddling the thorax and abdomen on the right side. Because of the sonographic appearance, neuroblastoma was diagnosed preoperatively. The mass was completely extirpated without difficulty.
This is a case report of a sliding hiatal hernia with severe gastroesophageal reflux (GER) after repair of congenital diaphragmatic hernia(CDH). It was not possible to determine whether the hiatal hernia is a de novo lesion which was missed at the original operation or a consequence of overzealous repair of the Bochdalek defect at the expense of weakening of the diaphragmatic crura. This case demonstrates that a sliding hiatal hernia can be a cause of severe gastroesophageal reflux that should be managed surgically.

