Lymphatic malformations are benign congenital malformations of the lymphatic system that occur predominantly in children. Most lymphatic malformations occur in the head and neck region, with those in abdominal locations, such as the mesentery, omentum and retroperitoneum, being less common, accounting for fewer than 5% of lymphatic malformations in children. This study analyzed the clinicopathologic characteristics and treatment outcomes of abdominal lymphatic malformations in children.
The medical records of 12 pediatric patients treated for abdominal lymphatic malformations at our institution between April 1999 and September 2017 were retrospectively reviewed. Demographic and clinical characteristics, including gender, age, symptoms and signs, diagnostic modalities, and treatment results, were analyzed.
The 12 patients included 11 boys and 1 girl, ranging in age from 3 months to 17 years (median 36.5 months) at presentation. The primary signs and symptoms included abdominal pain, abdominal mass and abdominal distention. Other symptoms and signs included fever, vomiting, scrotal pain and mass, and right inguinal mass. All patients were diagnosed by abdominal ultrasonography and computed tomography, and all underwent surgical excision with or without bowel resection. The lymphatic malformations occurred in the retroperitoneum (n=4), omentum (n=4), jejunal mesentery (n=2), and retroperitoneum and mesentery (n=2). Seven patients underwent complete mass excision, including 3 who underwent laparoscopic excisions, and 3 who underwent mass excision with segmental resection of the adjoining bowel. Two patients underwent incomplete excision because the lesion was extensive and invaded the superior mesenteric vessels. There was no major perioperative morbidity in any patient. At a median follow-up of 50 months (range, 8–183 months), only 1 patient experienced recurrence.
Although abdominal lymphatic malformations are benign, most children present with acute abdominal symptoms, necessitating early surgical treatment.
Citations

Although gallbladder (GB) hydrops in childhood is uncommon, it is most commonly associated with Kawasaki disease (KD) and can be a risk factor of poor outcomes in patients with KD. Our patient presented with a fever, diffuse abdominal pain, maculopapular rash, bilateral conjunctivitis, red and fissured lip tissue, and 3 days of right cervical swelling. Abdominal examination revealed abdominal distension and tenderness. Abdominal ultrasonography was performed to identify the source of abdominal symptoms, which revealed dilatation of the GB. Abdominal computed tomography scan was also performed to exclude other hepatobiliary disease, which showed normal hepatobiliary systems. The GB of our patients returned to a normal size without any complications, but it regressed very slowly. We report a case of a 6-year-old boy with KD who presented with markedly distended and unusually prolonged GB hydrops.
Citations

Preoperative ultrasonography (USG) in pediatric inguinal hernia has controversy. In this study, we analyzed the cases of pediatric inguinal hernia with/without preoperative USG and discussed whether USG is necessary.
We reviewed medical records of 1,441 patients who underwent inguinal hernia repair in Seoul National University Children's Hospital between January 2011 and August 2016 retrospectively.
Male were 69.3% and age at operation was 37.8±36.5 months old. There were 150 patients (10.4%) performed USG preoperatively. The department ordered to perform USG included department of surgery (n=71), emergency medicine (n=42), pediatrics (n=26), urology (n=10) and outside hospital (n=1). The reasons of performing USG included evaluation for hernia laterality (n=82), incarceration (n=28), testis (n=15), request of parents (n=14), scrotal mass (n=6) and incidentally found during evaluation for another disease (n=5). Excepting 5 cases of incidental finding, of 145 cases with USG, 12 (8.3%) cases changed the surgical plan; change to bilateral repair from unilateral repair (n=5), emergency operation due to incarceration (n=4) which include 1 salpingo-oophorectomy, 1 open abdomen surgery and 2 hernia repair after reduction of ovary, change to co-operation of orchiopexy (n=2) and change to laparoscopic surgery from open surgery due to herniation of both ovaries into one inguinal canal (n=1). In group without USG (n=1,291), 5 patients (0.4%) had unexpected problems during operation; 2 co-operation of orchiopexy because of transverse testicular ectopia (n=1) and right undescended testis (n=1), 2 hypertrophy of major labia and 1 retroperitoneal lymphangioma at inguinal area misdiagnosed as inguinal hernia.
It was difficult to interpret the meaning of preoperative USG because not all patients had performed it. In this study, 10.4% of patients performed USG and 8.3% of them changed surgical plan. About 0.4% of patients without preoperative USG would have benefited from it for surgery if they had performed it. Since the percentage is too low, it is unreasonable to conclude that USG has diagnostic utility in inguinal hernia in this study.
A 6-year-old male who lived with a mother in a single-parent family was referred to the emergency room with multiple traumas. There was no specific finding on CT scan of the other hospital performed 55 days before admission. However, CT scan at the time of admission showed common bile duct (CBD) stenosis, proximal biliary dilatation and bile lake formation at the segment II and III. Endoscopic retrograde biliary drainage was performed, but the tube had slipped off spontaneously 36 days later, and follow-up CT scan showed aggravated proximal biliary dilatation above the stricture site. He underwent excision of the CBD including the stricture site, and the bile duct was reconstructed with Roux-en-Y hepaticojejunostomy. Pathologic report of the resected specimen revealed that the evidence of trauma as a cause of bile duct stricture. While non-iatrogenic extrahepatic biliary trauma is uncommon, a level of suspicion is necessary to identify injuries to the extrahepatic bile duct. The role of the physicians who treat the abused children should encompass being suspicious for potential abdominal injury as well as identifying visible injuries.
Congenital esophageal stenosis (CES) is a rare disease that has been reported to occur once in every 25,000 to 50,000 births. According to its etiology, CES is divided into 3 subtypes, tracheobronchial remnants (TBR), fibromuscular hypertrophy (FMH) and membranous diaphragm (MD). Symptoms begin at the weaning period and the introduction of solid food around 6 months with dysphagia and vomiting. Esophagography is first screening test and endoscopic ultrasonography plays important roles to diagnose subtypes deciding therapeutic plan. TBRs were generally treated with surgical resection and end-to-end anasotomosis, whereas FMH and MD had good response rate to endoscopic or radiologic guided dilatation. This article reviews the literature on the etiology, clinical course, diagnosis and management of CES including recent opinion.
Gardner-associated fibroma (GAF) is a benign lesion of soft tissue which has recently been described and is exceedingly rare in children. GAF is associated with adenomatous polyposis coli gene mutation, familial adenomatous polyposis and desmoid. We report a case of patient with soft tissue tumor on her lower back which was turned out to be GAF. The patient was a 19-month-old female who visited out-patient clinic with palpable mass on her lower back and we performed surgical excision. The tumor was located at subcutaneous and we excised the tumor including surrounding soft tissue. She discharged without any complication on surgery day. The pathologic report showed dense collagenous tissue with spindle cell and adipose tissue, suggestive of GAF. We are planning to check gene study and to perform endoscopy and abdominal ultrasonography for at the age of 4.
The aim of this study was to analyze of the risk factors for surgical procedure on ileo-colic intussusception without leading point in children.
We retrospectively reviewed medical records of patient treated for ileo-colic intussusception between January 2003 and December 2014. We exclude the patients who had leading point. Because of the large difference on patient's numbers between non-operative group (cases of ileo-colic intussusceptions successfully reduced by air reduction) and operative group (cases underwent operation due to failed air reduction), we compared the data of operative group of patients without leading point between 2003 and 2014 with the data of non-operative group as control group from 2013 to 2014. Clinical features such as gender, age, body temperature, body weight in diagnosis, growth curves for age-gender-body weight, and laboratory data of blood test were compared.
In non-operative group, total 94 patients who were treated successfully by the non-operative air reduction. In operative group, total 21 patients treated by surgical procedure. The age under 12 months, weight over upper 75 percentile group, increased segment neutrophil count, decreased hemoglobin level and lymphocyte count were significantly associated with a requirement for surgical procedure.
We conclude that younger age, higher weight percentile group, increased segment neutrophil, decreased hemoglobin and lymphocyte are the independent risk factors related to operative treatment for ileo-colic intussusception in children. If primary air reduction is failed in patients with such risk factors, operative treatment over ultrasonography or secondary reduction can prevent unnecessary effort and complications, thus emphasizing the consideration of operative treatment when selecting treatment methods.
Citations

Nodular hidradenoma was diagnosed in a 29-month-old girl on her axilla. Hidradenoma, sometimes designated as acrospiroma, is a benign sweat gland neoplasm, which mostly occurs in adults. Very few cases of hidradenoma have been documented in children in their first decade of life. This case demonstrates that when a child develops a skin nodule, nodular hidradenoma can be a diagnostic option.
Citations

Congenital duodenal obstruction is a one of the emergent surgical conditions in neonates. Almost of them were diagnosed with double-bubble sign in prenatal ultrasonography. However, partial obstruction caused from duodenal web could be overlooked. We reported a duodenal web in early childhood. A three-year-old girl visited at our pediatric clinic for constipation. She had been showed non-bilious vomiting after weaning meal since 6 months old of her age, but her weight was relevant for 50-75 percentile of growth curve. Barium enema was initially checked, but any abnormal finding was not found. We noticed the severely distended stomach and 1st portion of duodenum. Upper gastrointestinal series revealed partial obstruction in 2nd portion of duodenum. After laparotomy, we found the transitional zone of duodenum and identified a duodenal web via duodenotomy. We performed duodeno-duodenostomy without any injury of ampulla of Vater. She was recovered uneventfully. During 6 months after operation, she does well without any gastrointestinal symptoms or signs, such as vomiting or constipation.
Gallbladder stones in children are not common without underlying hemolytic diseases or other risk factors like obesity. Ceftriaxone, a third generation cephalosporin, is known to make biliary precipitations that can be mistaken for biliary stones. We here report two children with biliary pseudolithiasis with different treatment modalities. One child was mistaken for symptomatic gallbladder stones and underwent elective laparoscopic cholecystectomy, while the other child, after thorough history taking on the ceftriaxone medication, was suspected of biliary pseudolithiasis and was treated conservatively. Both children had the history of usage of ceftriaxone in previous hospitals for infectious diseases. The ceftriaxone history of the first child was missed before the surgery. When gallbladder stones are found in children without any underlying diseases, specific history taking of the usage of ceftriaxone seems to be absolutely required. In this case, immediate interruption of the antibiotic could resolve the episode and avoid unnecessary surgical procedure.
Currently the substantial clinical benefits of single-port laparoscopic appendectomy (SLA) over conventional three-port laparoscopic appendectomy (CLA) are equivocal. The aim of this study was to compare surgical outcomes between SLA and CLA in children with acute appendicitis.
A single blind prospective randomized single center study was performed to compare the surgical outcomes of SLA and CLA. A total of 105 patients were randomized and various parameters were analyzed, 52 patients with SLA and 53 patients with CLA between July 2013 and March 2014. Patients with sonographically confirmed acute appendicitis were randomly assigned to receive either SLA or CLA. The outcome measurements were operating time, wound complication, and intraperitoneal morbidities, postoperative pain score and cosmetic result score.
Operating time is significantly longer in SLA (70.4±26.7 minutes vs. 58.0±23.4 minutes; p=0.016). There were no significant differences in the postoperative wound complication rate and intraperitoneal morbidities between two groups. There were no significant differences in postoperative resting pain score (6.6±2.5 vs. 6.3±2.5; p=0.317) and activity pain score (6.9±2.4 vs. 6.3±2.5; p=0.189), and the cosmetic result score (9.2±1.1 vs. 9.1±1.4; p=0.853).
Although SLA would be a safe and feasible procedure in children, SLA could not demonstrate the clear benefit over CLA.
Laparoscopic appendectomy (LA) has become a gold standard for children even in complicated appendicitis. The purpose of this study was to compare the postoperative surgical site infection rates between laparoscopic and open appendectomy (OA) group in pediatric complicated appendicitis.
A total of 1,158 pediatric patients (age ≤15 years) underwent operation for appendicitis over a period of 8 years. Among these patients, 274 patients (23.7%) were diagnosed with complicated appendicitis by radiologic, operative and pathologic findings, and their clinical outcomes were retrospectively analyzed.
Of the 274 patients with complicated appendicitis, 108 patients underwent LA and 166 patients underwent OA. Patients in the LA group returned to oral intake earlier (1.9 days vs. 2.7 days; p<0.01) and had a shorter hospital stay (5.0 days vs. 6.3 days; p<0.01). However, rate of postoperative intra-abdominal infection (organ/space surgical site infection) was higher in the LA group (LA 15/108 [13.9%] vs. OA 12/166 [7.2%]; p<0.01). Readmission rate was also higher in the LA group (LA 9/108 [8.3%] vs. OA 3/166 [1.8%]; p<0.01).
The minimally invasive laparoscopic technique has more advantages compared to the open procedure in terms of hospital stay and early recovery. However, intra-abdominal infection and readmission rates were higher in the laparoscopy group. Further studies should be performed to evaluate high rate of organ/space surgical infection rate of laparoscopic procedure in pediatric complicated appendicitis.
Citations

Laparoscopic hernia repair in children is still controversial. The aim of this study was to report our long-term results of the laparoscopic hernia technique, which is based on the same surgical principles as conventional open herniotomy.
Five hundred fourteen pediatric patients with inguinal hernia were included in this study under informed consent. All patients underwent a laparoscopic technique of sac transection and intracorporeal ligation. The asymptomatic contralateral inguinal ring was routinely explored and repaired if a patient had patent processus vaginalis on the contralateral side. Patients were prospectively followed for 5 years. Those who were lost to follow-up were excluded from the study. Perioperative complications and recurrences were evaluated.
The mean follow-up period was 29 months. Mean operation time was 27.5 minutes. Forty one percent of the patients had contralateral patent processus vaginalis. Only one hernia recurred (0.19%). We had one case of contralateral metachronous hernia (0.21%) during follow-up period.
The long-term follow-up results of our study revealed that laparoscopic hernia sac transection and ligation can be a safe and effective alternative for conventional herniorraphy.
Citations

The present study compared the postoperative analgesic effects of ilioinguinal and iliohypogastric nerve block with infiltration of local anesthetics (bupivacaine) into the wound in children after inguinal hernia repair. Ninety children below 7 years old who were scheduled elective inguinal hernia repair were randomly allocated into one of three groups. The patients in nerve block (NB) group, ilioinguinal and iliohypogastric nerve block was done with 0.5 mL/kg of 0.25% bupivacaine. The patients in infiltration of local anesthetics (LI) group, 0.5 mL/kg of 0.25% bupivacaine was infiltrated into the wound after surgery. The patients in control group were allocated as a Control group. Postoperative pain was assessed at 1, 3, 5, and 24 hours after operation with FLACC scale and additional analgesic consumption were counted. The three groups were not significantly different in age, sex, body weight, and duration of operation. Pain scores at 1 hour and 3 hours after operation were significantly higher in Control group than in NB group and LI group (
Citations

The aim of this study was to identify the risk factor related to the need for operative treatment and avoid unnecessary non-operative management for intussusception in children. We retrospectively reviewed medical records of patient treated for intussusception at our institution between January 2006 and January 2013. Clinical features such as gender, age, seasonal variation, symptoms and signs, treatment results were analyzed. Univariate and multivariate analyses including a chi-square test for categorical variables and logistic regression analysis were performed. During the study period, 356 patients were treated for intussusception. 328 (92.1%) was treated successfully by the non-operative pneumoreduction, and 28 (7.9%) required operative management. On univariate analysis, risk factors which were related to the need for operative treatment were age, vomiting, bloody stool, lethargy, and symptoms duration. A logistic regression analysis in order to assess for independent predictors of operative treatment was performed. Age (<6 vs ≥12 months) (OR 4.713, 95% CI 1.198~18.539,
Citations

Foreign body ingestion is a common problem among paediatric populations. Most of the ingested foreign bodies spontaneously pass through the gastrointestinal tract, but approximately less then 10% of them remain without being discharged, and trigger complications. Therefore, proper evaluation and treatment according to the situation is required. In this study, clinical progress and complications were analyzed according to the clinical features and treatment in children who ingested foreign bodies. Among pediatric patients under 18 who were admitted to Chonnam National University Hospital after ingesting foreign bodies between January 2008 to June 2012, only the patients who had their foreign body in the gastrointestinal tract were included in this study. Based on medical records, age, type of foreign body, time spent till admission, and whether the endoscopy was done or not, complication were researched retrospectively. According to symptoms and plain abdomen X-ray findings, treatment was chosen and conducted among endoscopy, observation and emergency operation. Among 273 patients, 9 (3.3%) of them had surgical removal. Seven (2.6%) of them had an emergency operation on the day of admission, and the rest 2 (0.7%) had operation during observation. Removal through initial endoscopic approach was tried in 157 (57.5%) patients. Eleven (70.8%) of them had their foreign body removed at the initial trial, and 5 (4.9%) of them at the second trial. Among 109, who were on observation status, 9 (8.3%) of them needed endoscopic removal, and 2 (1.8%) of them suffered from surgical removal. It is thought to be better to approach slowly considering the type, size and symptoms in foreign body ingestion of pediatric patients, rather than immediate and invasive removal.
Citations

Debates exist about the appropriate treatment for pancreatic trauma in children. We intended to examine the safety of the operation of pancreatic trauma in children. This is a retrospective study of 13 patients, younger than 15, who underwent surgery for pancreatic trauma, between 1993 and 2011 in Seoul National University Children's Hospital. Medical records were reviewed for mechanism of trauma, clinical characteristics, radiological findings, operation and outcomes. Organ injury scaling from the AAST (American Association for Surgery of Trauma) was used. All injuries were caused by blunt trauma. Patients with grade III, IV, and those who were difficult to distinguish grade II from IV, underwent surgery due to severe peritonitis. Three patients with grade II were operated for reasons of mesenteric bleeding, tumor rupture of the pancreas, and progression of peritonitis. Distal pancreatectomy was performed in 10 patients and subtotal pancreatectomy and pylorus preserving pancreaticoduodenectomy in 1 patient each. The remaining one underwent surgical debridement because of severe adhesions. The location of injury, before and after operation, coincided in 83.3%. The degree of injury, before and after the operation, was identical in all the patients except for those who were difficult to tell apart grade II from grade IV, and those cannot be graded due to severe adhesion. Postoperative complications occurred in 23.1%, which improved with conservative treatment. Patients were discharged at mean postoperative 12(range 8~42) days. Even though patients with complications took longer in time from diagnosis to operation, time of trauma to operation and hospital stay, this difference was not significant. In conclusion, When pancreatic duct injury is present, or patient shows deterioration of clinical manifestation without evidence of definite duct injury, or trauma is accompanied by other organ injury or tumor rupture, operative management is advisable, and we believe it is a safe and feasible method of treatment.
Citations

Ketamine is a safe and effective drug for pediatric anesthesia, sedation and analgesia. We hoped to identify that surgeons could operate a pediatric hernia with the ketamine anesthesia without general anesthesia. The study was a consecutive case series of 2230 inguinal hernia patients aged 1 months to 17 years in a Joo's day-surgical clinic during 11-year period. The patients had pediatric inguinal hernia surgery without general anesthesia under the day-surgery system. We retrospectively analyzed the medical record of patients who were registered with the Diagnosis Related Group (DRG) system. All patients received ketamine (5mg/kg) and atropine (0.01mg/kg) intramuscularly before surgery. After anesthesia, we injected 1~2% lidocaine (Less than 5ml) subcutaneously at the site of incision and started operation. The surgical method was the high ligation method of the hernia sac.) In total 2230 patients, male were 1756 and female were 474. 2076 patients were a unilateral inguinal hernia at the time of surgery and 154 were bilateral hernia patients. Less than three months, depending on the age of the patients was 391, and less than 12 months the patient was 592 people (26.5%). After surgery, there were no accidents or long term complications associated with ketamine anesthesia. We think the surgeon can safely do the pediatric inguinal hernia surgery using ketamine and lidocaine without anesthesiologist through 11 years of our surgical experiences.
Congenital segmental dilatation of the colon is a very rare entity of unknown etiology, characterized by a localized dilatation of a bowel segment of the colon of variable length and an abrupt transition between the normal and dilated intestine. It can affect any part of the colon, with the rectosigmoid colon being the most commonly affected site. The clinical and radiological features may resemble that of Hirschsprung disease, but differ in that the normal ganglion cells are found in the dilated and normal segment of the colon. We performed laparoscopic-assisted transanal endorectal pull-through for segmental dilatation of rectosigmoid colon in an 8-year-old boy with chronic constipation since the age of 5 months.
The purpose of this study is to analyze the early experience of the laparoscopic adhesiolysis for the intestinal obstruction due to postoperative adhesion. Seven patients were included in this study. The median age of those patients was 13, and there were 3 males and 4 females. Previous diagnosis and surgical procedure were various in seven cases, including small bowel resection with tapering enteroplasty, Boix-Ochoa fundopl ication, Ladd's procedure with appendectomy, mesenteric tumor resection with small bowel anastomosis, ileocecal resection and anastomosis, primary gastric repair, and both high ligation. A successful laparoscopic adhesiolysis was performed in one who had high ligation for inguinal hernia and had a single band adhesion. Six out of 7 (86%) cases needed to convert open surgery due to multiple and dense type of adhesion. In conclusion, laparoscopic approach with postoperative small bowel adhesion seems safe. However, it might be prudently considered because of high rates of conversion in children.
Pediatric liver transplantation has evolved into a definite and effective therapeutic modality for various liver diseases in the pediatric patient. During the last 25 years, liver transplant outcomes in Korea have reached international standards and Korea has become the leader in living-donor liver transplantation. This review will present the cumulative outcomes of pediatric liver transplantation performed in Korea and will focus on other issues of interest involving pediatric liver transplant recipients, especially in the field of immunosuppression and post-transplant lymphoproliferative disease.
Citations

Fundoplication is a common surgical procedure for gastroesophageal reflux Disease (GERD). Recently the procedure has been performed with increased frequency laparoscopically. The aim of this study is to compare laparoscopic Nissen fundoplication (LNF) and open Nissen fundoplication (ONF) for GERD in children. We studied retrospectively the 88 pediatric patients who underwent the Nissen fundoplication for GERD as primary antireflux surgery from 1994 and 2009. ONF was performed in 34 cases and LNF was in 54 cases. 58 patients have neurologic impairment. Time to initial food intake after the surgery were reduced in the LNF group (
Branchial cleft anomalies are the second most common head and neck congenital lesions seen in children. Amongst the branchial cleft malformations, second cleft lesions account for 95 % of the branchial anomalies. This article analyzes all the cases of second branchial cleft anomalies operated on at Seoul National University Hospital from September 1995 to February 2011. We analyzed sex, age, symptom and sign, accompanied anomaly, diagnosis, treatment, pathologic report and outcome via retrospective review of medical records. In this series, we had 61 patients (27 female and 34 male). The mean age at the time of operation was 38 months. 31 lesions were on the right, 20 were on the left and 10 were bilateral. The most frequent chief complaints at presentation were non-tender mass and cervical opening without any discharge. According to anatomic type, 29 patients had branchial cleft sinuses, 14 had cysts, 14 had fistulas and 4 had skin tags. Complete excision was attempted if possible and antibiotics challenged when infection was suspected. Complete excision was achieved in 96.7 % of cases. Incision and drainage was done in 2 cases due to severe inflammation, and both recurred. Postoperative complications included wound infection in 2 cases. Microscopic examonation revealed squamous epithelium in 90.2 % and squamous metaplasia in one case in the branchial cleft cyst wall. In summary, second branchial anomaly is found more frequently on right side of neck. Fistulas are diagnosed earlier than cystic forms. Most cases could be diagnosed by physical examination. The definitive treatment is complete excision and sufficient antibiotics coverage for cases with inflammation. After drainage of infected lesions, follow up excision after 1 year might be beneficial for preventing recurrence.
Acute appendicitis is one of the most common diseases of young people that requires emergency operation. This is especially true for those age 10 years old and older. However, the numbers of cases of appendicitis are increasing in both the young and the elderly. The main purpose of this study is to understand the clinical features of acute appendicitis in children and elderly patients. We retrospectively compared clinical characteristics in 4 groups of patients who underwent appendectomy in our hospital. There were 16 patients in the pre-school age group, 9 were males and 7 females. The total number of patients in the juvenile group were 287, 156 were males and 131 females. The total numbers of patients in the adult group were 794, 436 were males and 358 females. The numbers of elderly patients were 189, 91 were males and 98 females. Complicated appendicitis was found in 15 patients (93.7 %) in the pre-school age group, 79 patients (27.5 %) in the juvenile group, 332 patients (41.8 %) in the adult group, and 96 patients (50.7 %) in the elderly group. Four patients (40 %) had generalized panperitonitis in the pre-school group. The occurrence of perforated appendicitis was the highest in the pre-school age group and the lowest in the juvenile group. Since generalized panperitonitis has a higher incidence in the pre-school age group, prudent and careful diagnosis and treatment are required for the pre-school age group.
Minimally invasive techniques for pediatric inguinal hernia repair have been evolving in recent years. We applied the laparoscopic method to repair pediatric inguinal hernia using the techniques of sac transection and intra-corporeal ligation. Between November 2008 and August 2010, 67 pediatric patients (47 boys and 20 girls) with inguinal hernias were included in this study. Postoperative activities, pain, and complication were checked prospectively at regular follow-up. One patient presented with clinically bilateral hernia, and three patients had metachronous hernias. Thirty-two cases out of 63 patients with unilateral hernias had a patent processus vaginalis on the contralateral side. Mean operation time was 35±11.4 minutes for unilateral hernias and 43±11 minutes for bilateral hernias. There were no intra-operative complications. One patient had a small hematoma on the groin postoperatively, which subsided spontaneously in a week. Recurrence and metachronous hernia were not found at follow up. In summary, laparoscopic inguinal repair in children is safe, easy to perform and has an additional advantage of contralateral exploration. Further studies should include long term follow-up.
Citations

Thyroglossal duct cysts (TGDC) are the most common type of congenital developmental anomaly encountered in the anterior midline of the neck in childhood. The aim of the study was to evaluate the clinical characteristics of TGDC and identify any factors that could be related to recurrence after surgery. This study consisted of a retrospective chart review of 45 patients treated at Kyungpook National University Hospital for TGDC between 1990 and 2008. All records were reviewed for age and sex, length of history, presentation, diagnostic methods, sizes and locations of cyst, surgical management, histopathology of the lesion and recurrences. The statistical analysis of risk factors for recurrence was made using the Fisher's exact test with a significance level of p < 0.05. The male to female ratio was 2.2:1 with a male preponderance. The mean age at operation was 5 years and 2 months (4 months – 17 years). The most common presenting symptom was a nontender cervical mass (78%). Most TGDC were found in the midline position. Twenty four were infrahyoid, 17 were hyoid, and 4 were suprahyoid level. Forty one (91%) patients received the Sistrunk operation, and 4(9%) patients received cyst excision. Postoperative a seroma developed in six patients in the early postoperative days. There were a total of 3(6.6%) recurrences, 2 in patients who had excision only and in one patient who had the Sistrunk operation. Univariate analysis for risk factors with recurrence showed that there was no statistical relationship between the presence of preoperative infection and the development of recurrence. The removal of hyoid bone along with TGDC was a statistically significant risk factor for recurrent disease. This study suggests that the Sistrunk operation is the treatment of choice for TGDC in order to reduce recurrence.
Traumatic injury is one of the leading causes of morbidity and mortality in children. This is a clinical review of pediatric blunt abdominal trauma. A retrospective analysis of the 112 children with blunt abdominal trauma aged 15 years or less treated at the Department of Pediatric Surgery, Chonbuk National University Hospital was performed. The analysis included age, sex, injury mechanism, number and site of the injured organ, management and outcomes. The average age of occurrence was 7.6 years, and the peak age was between 6 and 8 years. There was a male preponderance with a male to female ratio of 2.3:1. The most common cause of blunt abdominal trauma was traffic accidents (61.6%), principally involving pedestrians (79.7%). The accident prone times were between 8:00 AM and 8:00 PM, the weekends (40.2%), and the winter respectively. Thirthy-five patients (31.2%) had multiple intra-abdominal organ injuries and the most common injured organ was the liver. Seventy-four cases (66.1%) were managed non-operatively and eleven cases (9.8%) expired. Of the patients who were treated surgically or were to be operated on one patient died before surgery, the remainder died during or after surgery. Risk factors such as number of injured organ, systolic and diastolic blood pressure, and trauma scores by Glasgow coma scale (GCS), Pediatric trauma score (PTS), revised trauma score (RTS), injury severe score (ISS), TRISS were significantly correlated with mortality rate.
Citations

Malignant ovarian tumors in children are very rare, and consist of about 1% of all childhood malignant tumors. The purpose of this study is to examine the clinical characteristics, treatment, and prognosis for children with malignant ovarian tumors. We retrospectively reviewed the medical records of children under 15 years of age with malignant ovarian tumors who had been treated surgically at Asan Medical Center between 1989 and March 2009. There were 32 patients, ranged in age at surgery from 2 to 15 years (mean; 10.4 years). The median follow-up period was 64.7 months (from 1 month to 188 months). Pathologic diagnosis were; immature teratoma (n=10), mixed germ cell tumor (n=10), and dysgerminoma (n=6). Tumor stage was classified by the staging system of the International Federation of Gynecology and Obstetrics (FIGO). The number of patients in stage I, II, III, and IV were 24 (75%), 2 (6.2%), 4 (12.5%), and 2 (6.1%), respectively. The tumor recurred in 4 patients. Seven patients of group 1 did not receive postoperative adjuvant chemotherapy, and in three of them, the tumor recurred. Twenty-five patients (group 2) underwent postoperative adjuvant chemotherapy, and there was only one recurrence. One patient who did not receive postoperative adjuvant chemotherapy and expired 10 months after operation because of tumor recurrence and distant metastasis. The overall 5-year event free survival (EFS) was 84.2%: group 1 in 44.4%, and group 2 in 95.7%. Tumor recurrence was related to the postoperative adjuvant chemotherapy (p=0.004). In conclusion, proper surgical procedures with relevant postoperative adjuvant chemotherapy might improve clinical results in children with malignant ovarian tumors.
Condyloma acuminatum is an uncommon disease but there is an increased incidence reported in recent years in prepubertal children. Anal and perianal condyloma accuminatum in children may suggest sexual abuse and treatment should include the thorough social evaluation as well as medical treatment. A 25 month old girl presented with multiple sessile nodules around her anal and perianal area, Biopsy confirmed the diagnosis of condyloma accuminatum. There was no definite evidence of sexual abuse, but her father had condyloma accuminatum involving his penis. The patient's lesions were excised totally. At three week follow up there was no anal stricture but there were newly developed small lesions around perianal area. Imiquimod onit was applied for 2 weeks and the recurred lesion disappeared completely. At postoperative 5 month, the operative area was fully epithelialized without recurrence.
Citations

Hickman catheters are tunneled central venous catheters used for long-term venous access in children with malignancies. The appropriate management for various kinds of catheter related complications has become a major issue. We retrospectively analyzed the clinical, demographic, and surgical characteristics in 154 pediatric hemato-oncology patients who underwent Hickman catheter insertion between January 2005 and December 2009. There were 92 boys and 62 girls. The mean age at surgery was 7.6±5.1 years old. The mean operation time was 67.4±21.3 minutes and C-arm fluoroscopy was used in 47(30.5%). The causes of Hickman catheter removal were termination of use in 82 (57.3%), catheter related bloodstream infection in 44(30.8%), mechanical malfunction in 11(7.7%), and accidents in 6(4.2%). Univariate and multivariate analysis for associated factors with catheter related bloodstream infection showed that there were no statistically significant associated factors with catheter related infection complications. All cases except two showed clinical improvement with catheter removal and relevant antibiotics treatment. The mean catheter maintenance period in patients of catheter removal without complications was 214.9±140.2 days. And, The mean catheter maintenance period in patients of late catheter related bloodstream infection was 198.0±116.0 days. These data suggest that it is important to remove Hickman catheter as soon as possible after the termination of use. When symptoms and signs of complications were noticed, prompt diagnostic approach and management can lead to clinical improvements.
Pancreaticoduodenectomy is the treatment of choice for adult periampullary lesions. However there has been no studies on the clinical outcomes of pancreaticoduodenectomy in children. To evaluate the clinical outcomes, records of 13 patients who underwent pancreaticoduodenectomy, from 1989 to 2009, at Seoul National University Children's Hospital were reviewed. Mean follow up period was 83 (2-204) months, the male to female ratio was 1:3.3, and the mean age was 11 (2-14) years. Ten patients underwent PPPD and 3 patients had Whipple's operation. The postoperative diagnosis included solid pseudopapillary tumor (9), cavernous hemangioma (1), pseudocyst (1), benign cyst (1), pancreatic disruption (1). Two patients developed postoperative adhesive ileus and among them one patient required operative intervention. Four patients required pancreatin supplementation due to steatorrhea and other gastrointestinal symptoms. There were no postoperative mortality during the follow up period and no evidence of recurrence in SPT patients. This study demonstrates that the pancreaticoduodenectomy procedure in children is not only feasible but also safe, with no mortality and an acceptable complication rate.
Pancreatic tumors in children are relatively rare, and their prognosis differs from that in adults. The purpose of this study is to examine the clinical characteristics, treatment, and prognosis for children with pancreatic tumors. We retrospectively reviewed the medical records of children under 15 years of age with pancreatic tumors who were treated surgically at Asan Medical Center between January 1992 and November 2009. There were 16 patients, fourteen of whom were pathologically diagnosed with solid pseudopapillary tumor. The other two patients were diagnosed with pancreatoblastoma and acinar cell carcinoma, respectively. Six patients of the 16 patients (38%) were male, and there was a male-to-female ratio of 1:1.6. The initial presentations were upper abdominal pain in eight patients (50%), palpable abdominal mass in three, and vomiting in one. Four patients were diagnosed incidentally. Six patients' tumors were located in the pancreatic head, six in the pancreatic body, and four in the pancreatic tail, respectively. The surgical procedures performed included distal pancreatectomy (n=7, 44%), median segmentectomy (n=3), enucleation (n=3), pancreaticoduodenectomy (n=2), and pylorus-preserving pancreaticoduodenectomy (n=1). Three patients underwent laparoscopic surgery. The median tumor size was 6.5cm (1.8~20 cm). Early surgical complications included pancreatic fistula (n=4), bile leakage (n=1), and delayed gastric emptying (n=1). A late complication in one patient was diabetes. The median follow-up period was five years and four months, and all patients survived without recurrence. While pancreatic tumors in adults have a poor prognosis, pancreatic tumors of childhood are usually curative with complete resection and thus have a favorable prognosis.
Contralateral groin exploration (CGE) in children with unilateral inguinal hernia remains controversial. Between January 2002 and December 2007, 1967 pediatric patients with inguinal hernia were treated by two surgeons with different criteria of CGE (group A; boys younger than 2 years, older boys prematurely delivered, and all girls, B; birth weight lower than 2kg with inguinal hernia presentation within 6 months after birth, and suspicious physical findings) at Samsung medical center. Patient's age, sex, body weight, diagnosis, and metachronous contralateral inguinal hernia (MIH) incidence were analyzed retrospectively. Among 895 patients in group A, CGE was performed in 460 patients (66.4%) and MIH incidence was 1.7%. In group B, 31 patients (3.5%) had CGE among 1072 patients, and MIH incidence was 4.2%. The average hospital costs of group A and B were 763,956 won and 500,708 won, respectively. The CGE criteria of group B had advantage in total hospital cost. The primary site and the age at presentation had a signiticant effect on the incidence of MIH. But MIH incidence was low and the more contralateral explorations lead to increase of total costs. Therefore, routine contralateral groin exploration and surgery for a patent processus vaginalis could not be justified.
Citations

Catheter related and perianal problems are common surgical complications encountered during the treatment of pediatric malignancies. However acute surgical abdominal emergencies are rare. The aim of this study is to review acute surgical abdominal complications that occur during the treatment of childhood malignancies. Out of a total of 1,222 patients who were newly diagnosed with malignant disease, between January 2003 and May 2008, there were 10 patients who required surgery because of acute abdominal emergencies. Their medical records were reviewed retrospectively. Hematologic malignancies were present in 7 patients (4 leukemia, 2 lymphoma, 1 Langerhans cell histiocytosis) and solid tumors in 3 patients (1 adrenocortical carcinoma, 1 desmoplastic small round cell tumor, 1 rhabdomyosarcoma). Seven patients had intestinal obstruction, two had gastrointestinal perforation and one, typhlitis. Intestinal obstructions were treated with resection of the involved segment with (N=2) or without (N=3) enterostomy. Two patients had enterostomy alone when resection could not be performed. Intestinal perforation was treated with primary repair. Typhlitis of the ascending colon was treated with ileostomy. Right hemicolectomy was necessary the next day because of the rapidly progressing sepsis. Three patients are now alive on chemotherapy and one patient was lost to followed-up. Among six patients who died, five died of their original disease progression and one of uncontrolled sepsis after intestinal perforation. Although rare, acute surgical abdominal complications can occur in childhood malignancies. Rapid and accurate diagnosis and appropriate operation are required for effective treatment of the complications.
Sertoli-Leydig cell tumor is a rare sex-cord stromal tumor of the ovary. They make up less than 0.5 % of all ovarian tumors. We experienced a case of an ovarian Sertoli-Leydig cell tumor in a 4 year-old girl who presented with nausea, vomiting, and lower abdominal pain of 2 days' duration. On physical examination, there was mild tenderness in the right lower quadrant of the abdomen. Abdominal ultrasonography and computed tomography (CT) scan revealed a pelvic mass measuring 5 × 3 cm that appeared to arise from the right ovary. At exploratory laparotomy, a 6 × 5 × 3 cm solid right ovarian mass without torsion was found. A right salpingo-oophorectomy was performed. The postoperative course was uneventful. The child was discharged 5 days after surgery.
Citations

Colorectal cancer is extremely rare in children. Unlike adult colorectal cancer, the overall prognosis of colorectal cancer in children is poor. Delayed diagnosis, advanced stages of the disease at presentation, and mucinous type of histology are the major determinants of poor outcome in childhood. A 13-year-old boy with abdominal pain visited our hospital. Physical examination andabdominal ultrasonography identified acute appendicitis with perforation. He underwent appendectomy and then the pathologic findings revealed mucinous adenocarcinoma. The cancer was located at the transverse colon and had metastases on peritoneal wall at 2nd laparotomy. Extended right hemicolectomy was performed. He underwent palliative chemotherapy. After 4 months later, hepatic metastasis and aggravated peritoneal seedings developed. He died of renal failure and pneumonia 13 months after operation. We need to have a high index of suspicion for the possibility of a malignant colorectal tumor in any childhood case with nonspecific signs and symptoms.
Wandering spleen is very rare condition in children characterized by migration of the spleen from its normal position due to laxity or absence of the supporting splenic ligaments. We experienced a case of splenic infarction due to torsion of a wandering spleen in a 6-year-old boy who presented with fever, vomiting, and abdominal pain of 2 day's duration. On physical examination, there was severe tenderness in the left upper quadrant of the abdomen. The plain abdominal radiograph showed marked colonic gaseous distension. Contrast-enhanced abdominal computed tomography scan showed decreased density of spleen in the normal position, consistent with infarction. At emergency laparotomy, a wandering spleen twisted 360° on its pedicle was found. Despite splenic detorsion, blood flow could not be restored. Splenectomy was therefore performed. The child was discharged 7 days after surgery without any complications.
Citations

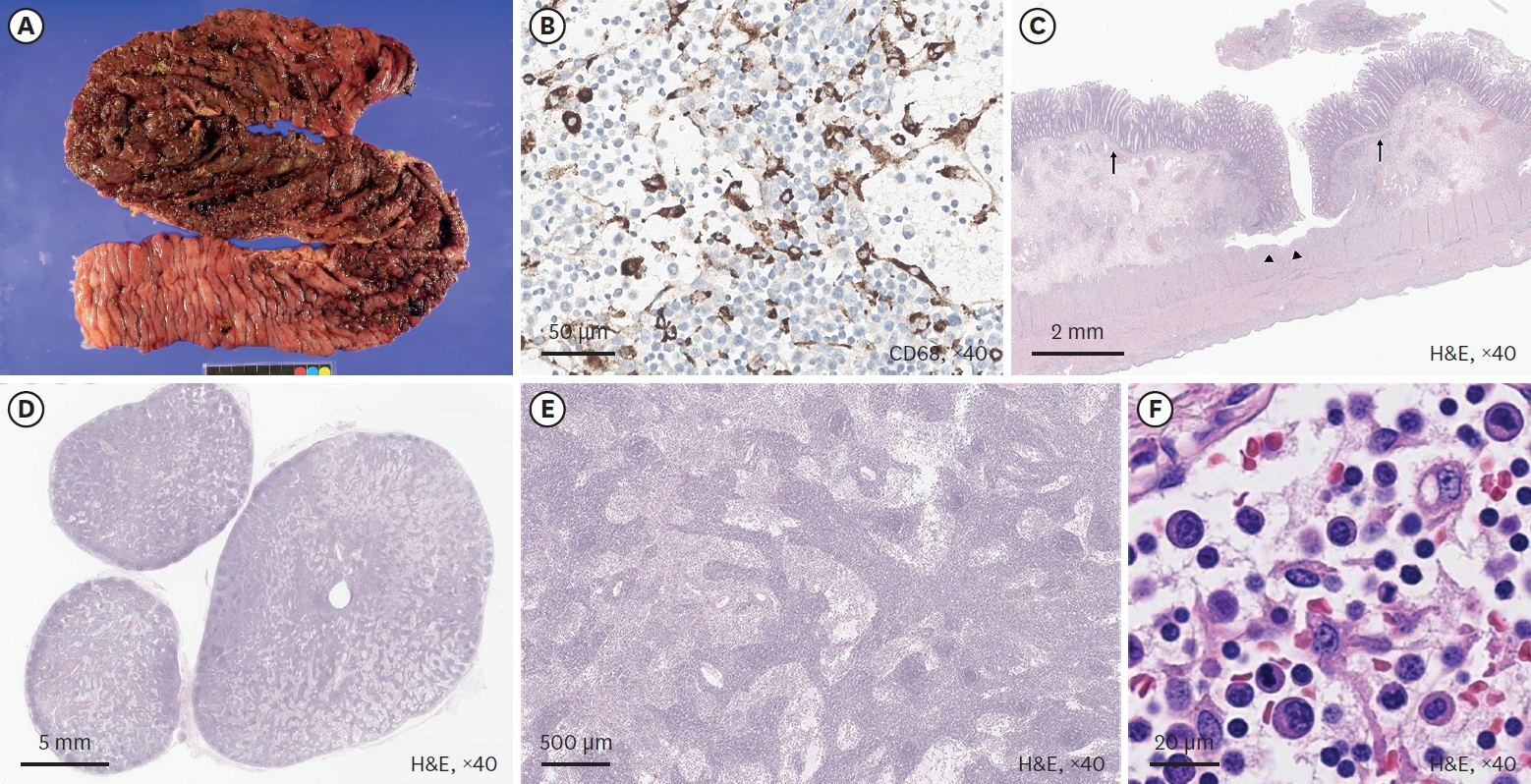
Inflammatory myofibroblastic tumor (IMT) is a rare reactive lesion characterized by the feature of myofibroblasts and a mixed inflammatory infiltrate that rarely undergoes malignant transformation. Extrapulmonary IMTs in children have been described involving the mesentery, omentum, retroperitoneum, abdominal soft tissues, liver, bladder, mediastinum, head and neck, extremity, appendix, and kidney. Medical records of children treated with abdominal IMT between 1985 and 2005 were reviewed retrospectively. Seven children were treated for IMT with the mean age of 3y 2m (range, 1y 1m to 14y). Tumors were located in transverse mesocolon (n=2), omentum (n=1), porta hepatis (n=2), complex site (antrum, duodenum, common bile duct, porta hepatis) (n=2). The symptoms included abdominal mass, fever, jaundice, abdominal pain and anemia. The masses were excised totally in transverse mesocolon, omentum IMT and there is no evidence of recurrence (follow-up periods: 6y 8m, 8y 9m, 4y 10m). In porta hepatis IMT, liver transplantations were performed and there is no evidence of recurrence (follow period: 6y 8m, 8y 7m). In one case of complex site IMT, partial excision of mass was performed and he still survived with no change of the residual tumor during follow-up period. The other one of complex site IMT denied further treatment after the biopsy. In conclusion, complete surgical excision including liver transplantation and close follow-up are mandatory for the abdominal IMT in child.
Citations

Children who underwent reparative operations for esophageal atresia (EA) with or without tracheoesophageal fistula (TEF), are confronted with many gastrointestinal or respiratory problems, especially during the early years of life. We reviewed the medical records of 50 patients who underwent repairs of EA with or without TEF at the Division of Pediatric Surgery, Samsung Medical Center, from December 1994 to December 2005. Current status of children was accessed by telephone-interview, but only 27 of them were accessible. Of 50 patients, 3 patients (6%) were type A, 45 patients (90%) were type C, and 2 patients (4%) were type E. The mean interval between primary operation and interview was 5.5 years. The incidences of growth retardation (<10 percentile of height/weight) were 39% and 21 % during the first 5 years after repairs, respectively. The incidences of dysphagia or gastroesophageal reflux and recurrent respiratory infections were 33% and 39 %, respectively. However, these problems were likely to improve as the children grew. The incidences of growth retardations (<10 percentile of height/weight) were 11% and 11% for the children more than five years postoperative. The incidences of dysphagia or gastroesophageal reflux and recurrent respiratory infections were 22% and 22%, respectively. Children with EA with or without TEF are faced with many obstacles. Close observation and adequate treatment for delayed postoperative complications are necessary to improve the quality of life for these children.
Citations

Chylous mesenteric cyst is a rare variant of mesenteric cystic lesions. Pathologically there is lack of communication of the main lymphatic vessels, resulting in cystic mass formation. Clinical presentation is diverse and can range from an incidentally apparent abdominal mass to symptoms of an acute abdomen. A 5-year-old girl presented with abdominal distension without pain. CT scan showed a huge and thin-walled cystic mass without solid portion. Laparotomy showed a 20 x 18 cm sized huge mesenteric cyst containing chylous fluid. Pathological diagnosis was cystic lymphangioma.
Lipoblastoma is a rare benign soft tissue tumor occurring in infancy and early childhood. It is characterized by fat lobules with varying degrees of maturity, multivaculoated lipoblasts, fibrocapillary networks and myxoid stroma. Lipoblastoma has a good prognosis with no metastases despite its potential for local invasion. From Jan, 1990 through April, 2007, 12 children underwent the operation for lipoblastoma, 7 boys and 5 girls, diagnosed at median 22 months (5~43 months). Median follow up was 6 year 7 months. Primary sites included back (n=5), intraabdominal (n=2) and one in each of buttock, chest wall, neck, nose and scalp. Tumors presented with a growing mass in 9 patients, abdominal distension in 2, and an incidental finding on chest radiography in one. Complete excisions were done in all patients. There was one recurrence in a patient with a scalp mass. After reoperation, he has been doing well without evidence of recurrence. Lipoblastoma has a favorable prognosis, but recurrence can occur even with complete excision. Regular follow up is necessary to detect recurrences.
Citations

Teratomas arising from totipotential primitive germ cell are composed of 2 or 3 germ cell layers. We reviewed the records of 166 children who underwent the operation for teratoma from Jan, 1990 through April, 2007. There were 40 boys and 126 girls (average age 6.93±5.83 years). Primary sites were ovary (n=88), sacrococcygeum (n=24), testis (n=16), retroperitoneum (n=16), mediastinum (n=8), brain (n=4), thymus (n=3) and a single tumor involved the adrenal gland, neck, middle ear, oropharynx, stomach, pelvis, omentum, chest wall and scalp. Teratomas were mature in 141 patients, and immature in 25. Six patients who had ovarian immature teratomas grade 2 or 3 with peritoneal gliomatosis underwent adjuvant chemotherapy. During follow up period, 6 mature teratomas recurred at sacrococcygeal area (n=1) and contralateral ovary (n=5). Five patients of them underwent reoperation and diagnosed as a mature teratoma, but one who had underwent a left salpingooophrectomy with right ovary cystectomy at initial operation was observed carefully. Teratomas were dominant in female patients and developed at various organs. Complete excision was needed for good prognosis. In case of immature teratoma, complete excision and appropriate chemotherapy according to grading can contribute to favorable results.
Adrenocortical tumors are very rare in children and the clinical course is not clearly understood. The aim of this study is to review the clinical characteristics and courses of pediatric adrenocortical tumors. The medical records of patients who underwent surgery for primary adrenal tumor at the Department of Surgery, Seoul National University hospital, from Jan. 1986 to Feb. 2006 were reviewed. There were 10 adrenocortical tumor patients; 5 had adrenocortical adenoma and 5 adrenocortical carcinoma. All of the adrenocortical adenomas presented as functioning tumors,
Citations

Pancreatic tumors in children are very rare but have a better prognosis compared with that in adult. Pediatric pancreatic tumors are more often benign and easier to resect. To evaluate the characteristics and prognosis, the records of 13 patients who underwent pancreatic resection, from June 1997 to May 2005, at Samsung Medical Center were reviewed. The mean follow up period was 48 months. The male to female ratio was 1: 1.6. Mean age was 10.3 years. Signs and symptoms included abdominal pain (7), abdominal palpable mass (5), jaundice (1), hypoglycemic (1), and non-specific GI symptoms (4). The commonly used diagnostic tools were CT and abdominal sonography. In addition, MRI, ERCP, EEG, and hormone test were also done when indicated. Surgical procedures included distal pancreatectomy (5), pylorus preserving pancreaticoduodenectomy (4), tumor excision (3), and subtotal pancreatectomy (1). Locations of lesions in pancreas were head (4), tail (5), and body and tail (4). Postoperative complications developed in 3 cases; postoperative ileus (1), wound problem (1), and pancreatitis (1). The pathologic diagnosis included solid-pseudopapillary tumor (6), congenital simple cyst (1), pancreatic duplication cyst (1), serous oligocystic adenoma (1), mucinous cystadenocarcinoma (1), rhabdomyosarcoma (1), insulinoma (1), and pancreatoblastoma (1). Three cases received adjuvant chemotherapy and radiotherapy. Overall survival rate was 81%. One patient with a mucinous cystadenocarcinoma died. In this study, pancreatic tumors in children were resectable in all patients and had good survival. Surgery of pancreatic tumors should be regarded as the gold standard of treatment and a good prognosis can be anticipated in most cases of benign and malignant tumors.
Liver tumors in children are rare, relatively complex, and encompass a broad spectrum of disease processes. This study reviews our experience of liver tumors during the last 10 years. Medical records of 36 cases of liver tumors?in children, treated at Samsung Medical Centers, from October 1994 to December 2005, were reviewed in this study. We analyzed disease characters and survival rates as a whole and by specific disease. The median age was 3.6 years. Male and female ratio was 1:1. The most common symptom was the palpable mass in 15 cases. Others were abdominal distension in 9 cases, jaundice in 2, vomiting in 2, weight loss in 2, and pubic hair growth in 1. CT or US and liver biopsy were performed for diagnosis. There were 28 malignant tumors: malignant rhabdoid tumor (1 case), hepatocellular carcinoma (3 cases), hemangioendothelioma type II (3 cases), angiosarcoma (1 case), and hepatoblastoma (20 cases). Eight tumors were benign; hepatic adenoma (1 case), focal nodular hyperplasia (2 cases), hemangioendothelioma type I (2 cases), mesenchymal hamartoma (3 cases). In this study the clinical characteristics were not different from the other reports. Liver transplantation was performed in 3 cases-1 with hepatoblastoma and 2 with hepatocelleular carcinoma. Accurate and early diagnosis, and individualized multi- modality therapeutic approaches might be important for better outcome.
Citations

Meckel's diverticulum is the most common congenital anomaly of gastrointestinal tract in children. The incidence of complicated Meckel's diverticulum is about 4%. The major complications of Meckel's diverticulum are bleeding, intussusception, obstruction and perforation. The aim of this study was to investigate the clinical manifestations and the role of laparoscopic surgery in complicated Meckel's diverticulum in children. We retrospectively reviewed the medical records of 19 patients with complicated Meckel's diverticulum who underwent operation at Asan Medical Center between Jan. 1990 and Apr. 2007. Male to female ratio was 11:8, and median age was 1 year (1 day-13 years). The most frequent symptom was hematochezia (68%), followed by irritability or abdominal pain (16%), vomiting (11%), and abdominal distension (5%). Two operative procedures were performed; small bowel resection with anastomosis (68%) and diverticulectomy (32%). The operation proven complications of the Meckel's diverticulum were bleeding (68%), intussusception (16%), perforation (11%) and obstruction (5%). Ectopic tissues found by postoperative pathologic examination were gastric (84%) and pancreatic (11%). Hospital stay after laparoscopic operation for bleeding Meckel's was 5 days (median) and average first postoperative feeding was 1.5 days. On the contrary, hospital stay for open surgery was 7 days and first feed was 3 days. In summary, the most common compliation of Meckel's diverticulum in children was bleeding and ectopic gastric tissues were present in 84%. Laparoscopic procedure seemed to be useful for diagnosis as well as for definitive treatment.
Citations


