Although nonoperative treatment of appendicitis (NOTA) in the pediatric population has been well reported recently, patient selection and treatment scheme varies among studies, making it difficult to establish treatment standards for NOTA.
In a single medical center, patients younger than 18 years who were diagnosed with appendicitis: 1) with abdominal pain not exceeding 24 hours, 2) without radiologic evidence of appendicolith or appendiceal perforation or pelvic abscess, and 3) without signs of frank generalized peritonitis were offered NOTA, and their data were prospectively collected.
Twenty-two patients with uncomplicated appendicitis agreed to NOTA and were enrolled in the study. The initial success rate (resolution of abdominal pain and hospital discharge without appendectomy) was 100% (22 out of 22 patients). At a median follow-up period of 23.8 months, two patients had recurrence at two and three months after completion of NOTA. These patients underwent laparoscopic appendectomy.
Stringent patient selection may be necessary to apply NOTA safely for all children with uncomplicated appendicitis. Further studies concerning patient selection and conformed treatment protocols for NOTA are required.
This study aimed to evaluate the relationship between nutritional support and growth velocity after abdominal surgery in neonates.
The electronic medical records of 45 neonates who underwent abdominal surgery in neonatal intensive care unit from 2012 to 2016 were collected to see how surgery and postoperative nutrition affect for the growth of neonate with abdominal surgery. The growth velocity was measured from the time of surgery to the time of discharge based on body weight.
In neonates who achieve their protein requirement on the first day after surgery, the growth velocity was better than that in neonates who did not achieve their protein requirement on the first day after surgery (4.31 vs. 15.21; p=0.004). Based on the type of surgery, length of bowel resection and surgical complications, this study showed better growth velocity in neonates who had no surgical complications (5.34 vs. 12.74; p=0.775), reoperation (5.25 vs. 22.19, p=0.987), or bowel resection (6.79 vs. 9.95, p=0.302). However, there was no statistically significant difference among these factors.
We concluded in this study that adequate protein supplement from the first day of surgery could have a positive effect on the growth velocity of neonates who underwent abdominal surgery.
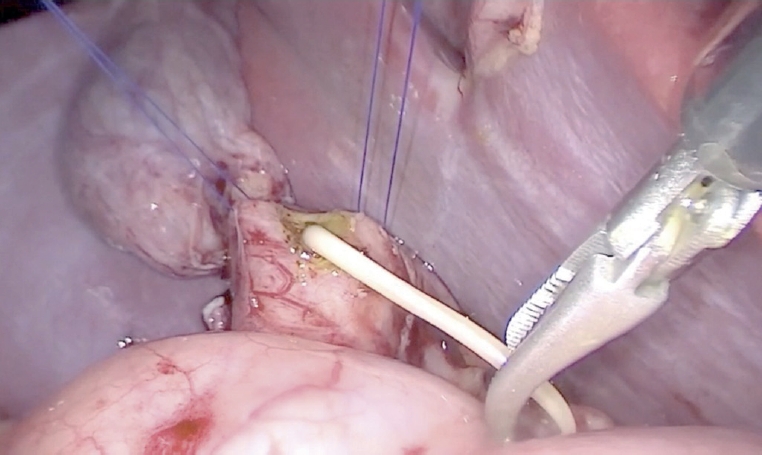
Single-port laparoscopy-assisted surgery is being performed for various operations in pediatric patients recently. The aims of this study were to prove the safety and find well-matched indications of small bowel resection using single-site umbilical laparoscopic surgery (SSULS).
From 2011 to 2016, 29 pediatric patients underwent SSULS. Medical records were retrospectively reviewed.
A total of 29 patients were included and 30 SSULS were performed in this study. The mean age at operation was 5.7 years, and the mean weight was 21.9 kg. Meckel's diverticulum was the most common indication for SSULS, followed by small bowel intussusception due to leading point mass, small bowel duplication, and Crohn's disease. In most cases, estimated blood loss was negligible except in Crohn's disease with severe inflammation. While answering post-discharge questions about scars, most parents responded that they were satisfied with the postoperative wound.
SSULS is a useful operation to try even for surgeons who do not have advanced laparoscopic skills. Complication rates of single-port operations do not differ from those of conventional laparoscopic operations. Most lesions of the small bowel could be indications of SSULS. Careful attention is required when performing SSULS in patients with Crohn's disease.
A 6-year-old male who lived with a mother in a single-parent family was referred to the emergency room with multiple traumas. There was no specific finding on CT scan of the other hospital performed 55 days before admission. However, CT scan at the time of admission showed common bile duct (CBD) stenosis, proximal biliary dilatation and bile lake formation at the segment II and III. Endoscopic retrograde biliary drainage was performed, but the tube had slipped off spontaneously 36 days later, and follow-up CT scan showed aggravated proximal biliary dilatation above the stricture site. He underwent excision of the CBD including the stricture site, and the bile duct was reconstructed with Roux-en-Y hepaticojejunostomy. Pathologic report of the resected specimen revealed that the evidence of trauma as a cause of bile duct stricture. While non-iatrogenic extrahepatic biliary trauma is uncommon, a level of suspicion is necessary to identify injuries to the extrahepatic bile duct. The role of the physicians who treat the abused children should encompass being suspicious for potential abdominal injury as well as identifying visible injuries.
Anorectal duplications account for only 5% of gastrointestinal duplications, and cases with involvement of the anal canal are much rarer. Nearly all anorectal duplications are posterior to the rectum; duplications located anterior to the normal rectum are highly unusual, and only a few cases have been reported. We report the case of an anterior anorectocolonic duplication presenting as a rectovaginal fistula in a 2-month-old infant. After diagnosis, the duplication was excised completely without further intestinal complications.
Thyroid cancer is a rare disease in pediatric population, but its incidence rate is increasing. The aim of this report is to present a single institution experience of pediatric thyroid cancer and to identify clinical features, predisposing factors, and postoperative course of pediatric thyroid cancer.
We retrospectively reviewed 35 pediatric patients who underwent operation due to thyroid cancer at Seoul National University Children's Hospital between May 1997 and January 2017. The median follow-up period was 70 months (range, 5–238 months).
The mean age at operation was 12.0±5.91 years and 27 patients were female. The underlying conditions in patients included history of chemoradiotherapy for previous other malignancies (n=4), hypothyroidism (n=3), history of chemotherapy (n=2), family history of thyroid cancer (n=1) and history of radiation therapy (n=1). The initial symptoms were palpable neck mass (n=21) and incidental findings (n=11). Total thyroidectomy (n=30) or unilateral lobectomy (n=5) were performed. There were 15 postoperative complications including transient hypocalcemia in 14 patients and Horner's syndrome in 1 patient. The most common pathologic cell type was papillary thyroid cancer (n=29). Extrathyroid extension and lymph node invasion were found in 25 patients and 27 patients, respectively. Thirteen patients showed multifocality. During follow-up period, 5 patients underwent additional operation because of tumor recurrence in lymph nodes. Lung metastasis was detected in 3 patients at the time of diagnosis and in 3 patients during follow-up period. The mortality rate was zero and mean disease-free survival was 83.7±47.9 months.
Pediatric thyroid cancer has lower mortality rate and recurrence rate as seen in this study despite the advanced stage at diagnosis. A thorough follow-up of patients with an underlying condition such as history of chemoradiotherapy and understanding new pediatric guideline can be helpful to maximize patients' survival and prognosis.
We report a neonatal case of “intraluminal” pyloric duplication cyst, causing gastric obstruction after birth. Endoscopy revealed a submucosal cystic lesion approximately 15 mm in size arising from the anterior and inferior surfaces of the pylorus obliterating the pyloric canal. After laparotomy, intraoperative cholangiography was performed, which documented no communication between the cyst and the bilio-pancreatic duct. Gastrotomy was performed transversally over the antrum, and the cyst delivered through the incision. The cyst was incised, the upper part of the cyst wall removed, and a mucosectomy performed on the inner cyst wall of the lower part. The mucosa and muscle of the margin of the cyst were approximated. At follow up of 10 months, the patient is well without any sign of gastric obstruction.
There have been a few reports of familial anorectal malformations extending over more than one generation. We experienced a case of a family with 3 members spanning 2 generations affected with isolated low type anorectal malformations. They had same low type of anorectal malformations. In all 3 patients, a perianal anoplasty was performed.
Number of pediatric cholecystectomy has been recently showing a gradually increasing trend. The purpose of this study was to investigate the clinical features of patients who underwent pediatric cholecystectomy, and the latest trend in cholecystectomy.
In the present study, we conducted a retrospective chart review on 47 patients who had undergone cholecystectomy at a single center. The entire patient population was divided into two groups, according to the time of cholecystectomy (early group, January 1999 to December 2006; late group, January 2007 to August 2014).
The comparison between the early and late groups showed that the number of cholecystectomy increased from 13 to 34 cases representing a 2.6-fold increase. The mean patient age also increased from 5.94±4.08 years to 10.51±5.57 years (p=0.01). Meanwhile, laparoscopic surgery also increased from 15.4% to 79.4%, respectively (p<0.001). However, sex, mean body mass index, comorbidities, indications of cholecystectomy, and previous total parenteral nutrition were not statistically significant.
The results of this study showed that pediatric cholecystectomy cases are increasing, particularly in the 10 to 19 years age group and laparoscopic cholecystectomies are also being performed at an increasing rate. When the patients were compared according to the time of cholecystectomy, there were no differences in other risk factors or indications for cholecystectomy.
The congenital H-type rectovestibular fistula, a fistula between the anorectum and genital tract besides a normal anus is a rare variant of anorectal deformities. This disease needs proper treatment but there are no standard of diagnosis and treatment. The purpose of this report is to review a 13-year experience of approach and management for H-type rectovestibular fistula at a single institution.
From February 2002 to August 2015, we cared for 11 patients who had congenital H-type rectovestibular fistula and reviewed their clinical presentation, accompanied anomalies, diagnostic modalities, operative technique, and postoperative progress.
Most patients with H-type rectovestibular fistula presented with symptoms including vestibular defecation and major labial abscess. We could find the fistula tract in most of patients by fistulography using contrast dye. All of the patients had been operated. There were 2 recurrences after surgical treatment who had inflammation and infection associated with the fistula. All other patients recovered without complications.
We think the operation including fistulectomy and repair of perineal body through a transanal approach can be a feasible option to the congenital H-type rectovestibular fistula. Also, combined inflammation and infection should be treated prior to surgery to reduce postoperative complications.
The aim of this study was to analyze of the risk factors for surgical procedure on ileo-colic intussusception without leading point in children.
We retrospectively reviewed medical records of patient treated for ileo-colic intussusception between January 2003 and December 2014. We exclude the patients who had leading point. Because of the large difference on patient's numbers between non-operative group (cases of ileo-colic intussusceptions successfully reduced by air reduction) and operative group (cases underwent operation due to failed air reduction), we compared the data of operative group of patients without leading point between 2003 and 2014 with the data of non-operative group as control group from 2013 to 2014. Clinical features such as gender, age, body temperature, body weight in diagnosis, growth curves for age-gender-body weight, and laboratory data of blood test were compared.
In non-operative group, total 94 patients who were treated successfully by the non-operative air reduction. In operative group, total 21 patients treated by surgical procedure. The age under 12 months, weight over upper 75 percentile group, increased segment neutrophil count, decreased hemoglobin level and lymphocyte count were significantly associated with a requirement for surgical procedure.
We conclude that younger age, higher weight percentile group, increased segment neutrophil, decreased hemoglobin and lymphocyte are the independent risk factors related to operative treatment for ileo-colic intussusception in children. If primary air reduction is failed in patients with such risk factors, operative treatment over ultrasonography or secondary reduction can prevent unnecessary effort and complications, thus emphasizing the consideration of operative treatment when selecting treatment methods.
A case of congenital ectopic scrotum in neonatal period is described. The ectopic scrotum was located in the right inguinal area and the left hemiscrotum was found in normal location and each hemi-scrotum contained their testis. The neonate also had imperforate anus as low anorectal malformation with spinal abnormalities (hemi-sacrum and hemi-pelvis), right knee flexion contracture and right club foot. The embryological explanation in the literature of ectopic scrotum and its associated anomalies is discussed.
Recent data suggest that monotherapy with a broad-spectrum antibiotic may be as efficacious as, and potentially less costly than, standard multi-drug therapy. We compared mono-therapy with intravenous piperacillin-tazobactam (PT) with multi-drug therapy with cefotaxime and metronidazole (CM) in aspect of postoperative complications and hospital stay.
We reviewed the hospital records and medical costs of the pediatric patients who were managed for perforated appendicitis between April 2013 and May 2014 retrospectively.
Forty-six patients with laparoscopic appendectomy for perforated appendicitis were included in our study. PT group was 20 and CM group was 26 patients. On admission, there were no significance in sex distribution, duration of symptoms, leukocyte count, and CRP levels. At postoperative third, fifth, and seventh day of each regimen, PT group have no statistical difference with CM group in leukocyte count, percentage of neutrophil, and CRP. There was no difference in abscess formation rate, wound infections, and hospital stay between two groups. There was only one patient who was readmitted with elevation of CRP and leukocyte count in CM group.
Daily dosing with the mono-therapy of PT offers as efficient as multi-drug therapy of CM. To evaluate the efficacy of broad-spectrum antibiotics monotherapy in perforated appendicitis children, the cohort included more patients should be needed.
The duplication of gastrointestinal tract has been known to be a rare condition and two different forms, cystic and tubular type. This study was conducted to examine its clinical characteristics, especially cystic enteric duplication which was detected antenatally or postnatally.
There were 13 patients, who confirmed as cystic enteric duplication after operation between July 1996 and June 2015. Clinical data, including a gender, age at operation, presenting symptoms, diagnostic modalities, locations of lesion, and results of surgical treatment, were reviewed retrospectively according to cases detected antenatally and postnatally.
Five cases were included in antenatal diagnosis group and 8 cases in postnatal diagnosis group. Both groups show slightly common in female and the lesion most common in ileum. Antenatal diagnosis group shows 2 males and 3 females and the mean age at operation was 12±52 days (range, 5 to 90 days). They received operation regardless of symptom. Postnatal group shows 3 males and 5 females and the mean age at operation was 462.5±777.0 days (range, 4 days to 6 years). Moreover, 6 patients (75.0%) were age before 2 years. They usually presented abdominal pain with vomiting.
Cystic enteric duplication could present symptoms at any time during childhood, mainly before 2 years old, and so a proper management should be considered when suspect it. Although it is uncommon, surgical management including a minimal invasive procedure could be attempted despite the neonatal period.
Cervical lymphangiomas are rare lymphovascular malformations arising in the neck, which form huge fluid-containing cysts. Treatment of the malformation consists of surgery and sclerotherapy. However, the optimal approach is still controversial. Here, we describe a series of cervical lymphangiomas which have been treated with surgical approaches.
We retrospectively investigated the medical records of 82 patients who had been diagnosed with cervicofacial lymphangioma from 2001 to 2012 in our center. A closed suction drainage with negative pressure was placed on the operative lesion following excision to prevent reaccumulation of lymphatic fluid and the drainage tube was removed after injecting OK-432 through the tube.
Twelve patients underwent surgical excision of cervical lymphangioma. The median patient age was 3 months at the time of the operation. The patients have been followed-up over a period of 34 months. When lesions were located near vital organs such as the trachea or carotid artery or did not respond to repetitive OK-432 injections, surgical treatment might bring good outcomes. However, swallowing difficulty, lip palsy, or dyslalia due to adjacent nerve damage temporarily appeared as postoperative complications. Five children had tracheostomy due to tracheal or subglottic stenosis and 2 patients had gastrostomy due to aspiration while they eat after surgery.
Surgery for cervicofacial lymphangioma should be conducted carefully in selective cases. A well thought-out surgical plan with a multidisciplinary surgical team approach and placement of closed suction drainage tube after surgery and adjuvant OK-432 sclerotherapy through drainage tube seem to be helpful for good outcome.
Abdominal actinomycosis is a rare and chronic progressive disease, especially in children. Clinically, it has non-specific symptoms and diagnostic findings as well as low prevalence, making it very difficult to diagnose prior to intraoperative pathological confirmation. For this reason, abdominal actinomycosis is commonly misdiagnosed as appendicitis. After the histopathological diagnosis of abdominal actinomycosis is made, patients should be administered an appropriate antibiotic such as penicillin. Here we describe a case of appendiceal actinomycosis in an 18-year-old girl who was initially diagnosed with acute appendicitis.
Although Meckel's diverticulum is the most common vitellointestinal duct (VID) anomaly, patent vitellointestinal duct (PVID) is the most common symptomatic embryological defect. Patient may present with the anomaly itself or due to complications like intestinal obstruction secondary to volvulus, intussusception or adhesions. Prolapse occurs if the diverticulum is wide-mouthed enough to allow bowel to come out or due to increased intra-abdominal pressure like cry or cough. Bowel prolapse through PVID is rare and double prolapse of proximal as well as distal loop in a newborn is extremely rare. Omphalocele with prolapsing bowel through PVID as found in our index case is even rarer in literature. The pediatric surgeon should be familiar with these varied manifestations in the newborn because the prolapsed bowel can progress to gangrene and complications if not identified and operated upon early.
Congenital duodenal obstruction is a one of the emergent surgical conditions in neonates. Almost of them were diagnosed with double-bubble sign in prenatal ultrasonography. However, partial obstruction caused from duodenal web could be overlooked. We reported a duodenal web in early childhood. A three-year-old girl visited at our pediatric clinic for constipation. She had been showed non-bilious vomiting after weaning meal since 6 months old of her age, but her weight was relevant for 50-75 percentile of growth curve. Barium enema was initially checked, but any abnormal finding was not found. We noticed the severely distended stomach and 1st portion of duodenum. Upper gastrointestinal series revealed partial obstruction in 2nd portion of duodenum. After laparotomy, we found the transitional zone of duodenum and identified a duodenal web via duodenotomy. We performed duodeno-duodenostomy without any injury of ampulla of Vater. She was recovered uneventfully. During 6 months after operation, she does well without any gastrointestinal symptoms or signs, such as vomiting or constipation.
Currently the substantial clinical benefits of single-port laparoscopic appendectomy (SLA) over conventional three-port laparoscopic appendectomy (CLA) are equivocal. The aim of this study was to compare surgical outcomes between SLA and CLA in children with acute appendicitis.
A single blind prospective randomized single center study was performed to compare the surgical outcomes of SLA and CLA. A total of 105 patients were randomized and various parameters were analyzed, 52 patients with SLA and 53 patients with CLA between July 2013 and March 2014. Patients with sonographically confirmed acute appendicitis were randomly assigned to receive either SLA or CLA. The outcome measurements were operating time, wound complication, and intraperitoneal morbidities, postoperative pain score and cosmetic result score.
Operating time is significantly longer in SLA (70.4±26.7 minutes vs. 58.0±23.4 minutes; p=0.016). There were no significant differences in the postoperative wound complication rate and intraperitoneal morbidities between two groups. There were no significant differences in postoperative resting pain score (6.6±2.5 vs. 6.3±2.5; p=0.317) and activity pain score (6.9±2.4 vs. 6.3±2.5; p=0.189), and the cosmetic result score (9.2±1.1 vs. 9.1±1.4; p=0.853).
Although SLA would be a safe and feasible procedure in children, SLA could not demonstrate the clear benefit over CLA.
The purpose of this study was to compare the diagnostic accuracy of the non-invasive diagnostic methods and rectal suction biopsy for the detection of Hirschsprung disease (HD).
We reviewed diagnostic methods and results retrospectively in patients who underwent anorectal manometry, barium enema and rectal suction biopsy for the diagnosis of HD at Asan Medical Center from January 2000 to December 2012.
There were 97 patients (59 neonates and 38 infants) in the study period. The overall accuracy of anorectal manometry for the diagnosis of HD was 71.1% and its sensitivity was 51.4% (48.1% in neonate and 62.5% in infant, respectively) and its overall specificity was 82.3% (81.3% in neonate and 83.3% in infant, respectively). The Overall accuracy of barium enema was 66.0% (72.8% in neonate and 55.3% in infant, respectively) and specificity of barium enema was 53.2% (56.3% in neonate and 50.0% in infant, respectively). These results were lower than those of anorectal manometry. The overall sensitivity of barium enema was 88.6% (92.6% in neonate and 75.0% in infant, respectively) and it was higher than the sensitivity of anorectal manometry. Histological studies confirmed HD in 35 patients, in one of whom the suction biopsy showed negative finding.
Accuracy of non-invasive methods for diagnosis of HD in our study is lower than those in previous study, so we need to improve the quality of diagnostic tools in our hospital. We conclude that the rectal suction biopsy is the most accurate test for diagnosing HD, so the biopsy to confirm the diagnosis of the HD is very important.
Laparoscopic appendectomy (LA) has become a gold standard for children even in complicated appendicitis. The purpose of this study was to compare the postoperative surgical site infection rates between laparoscopic and open appendectomy (OA) group in pediatric complicated appendicitis.
A total of 1,158 pediatric patients (age ≤15 years) underwent operation for appendicitis over a period of 8 years. Among these patients, 274 patients (23.7%) were diagnosed with complicated appendicitis by radiologic, operative and pathologic findings, and their clinical outcomes were retrospectively analyzed.
Of the 274 patients with complicated appendicitis, 108 patients underwent LA and 166 patients underwent OA. Patients in the LA group returned to oral intake earlier (1.9 days vs. 2.7 days; p<0.01) and had a shorter hospital stay (5.0 days vs. 6.3 days; p<0.01). However, rate of postoperative intra-abdominal infection (organ/space surgical site infection) was higher in the LA group (LA 15/108 [13.9%] vs. OA 12/166 [7.2%]; p<0.01). Readmission rate was also higher in the LA group (LA 9/108 [8.3%] vs. OA 3/166 [1.8%]; p<0.01).
The minimally invasive laparoscopic technique has more advantages compared to the open procedure in terms of hospital stay and early recovery. However, intra-abdominal infection and readmission rates were higher in the laparoscopy group. Further studies should be performed to evaluate high rate of organ/space surgical infection rate of laparoscopic procedure in pediatric complicated appendicitis.
The aim of this study was to identify the risk factor related to the need for operative treatment and avoid unnecessary non-operative management for intussusception in children. We retrospectively reviewed medical records of patient treated for intussusception at our institution between January 2006 and January 2013. Clinical features such as gender, age, seasonal variation, symptoms and signs, treatment results were analyzed. Univariate and multivariate analyses including a chi-square test for categorical variables and logistic regression analysis were performed. During the study period, 356 patients were treated for intussusception. 328 (92.1%) was treated successfully by the non-operative pneumoreduction, and 28 (7.9%) required operative management. On univariate analysis, risk factors which were related to the need for operative treatment were age, vomiting, bloody stool, lethargy, and symptoms duration. A logistic regression analysis in order to assess for independent predictors of operative treatment was performed. Age (<6 vs ≥12 months) (OR 4.713, 95% CI 1.198~18.539,
Foreign body ingestion is a common problem among paediatric populations. Most of the ingested foreign bodies spontaneously pass through the gastrointestinal tract, but approximately less then 10% of them remain without being discharged, and trigger complications. Therefore, proper evaluation and treatment according to the situation is required. In this study, clinical progress and complications were analyzed according to the clinical features and treatment in children who ingested foreign bodies. Among pediatric patients under 18 who were admitted to Chonnam National University Hospital after ingesting foreign bodies between January 2008 to June 2012, only the patients who had their foreign body in the gastrointestinal tract were included in this study. Based on medical records, age, type of foreign body, time spent till admission, and whether the endoscopy was done or not, complication were researched retrospectively. According to symptoms and plain abdomen X-ray findings, treatment was chosen and conducted among endoscopy, observation and emergency operation. Among 273 patients, 9 (3.3%) of them had surgical removal. Seven (2.6%) of them had an emergency operation on the day of admission, and the rest 2 (0.7%) had operation during observation. Removal through initial endoscopic approach was tried in 157 (57.5%) patients. Eleven (70.8%) of them had their foreign body removed at the initial trial, and 5 (4.9%) of them at the second trial. Among 109, who were on observation status, 9 (8.3%) of them needed endoscopic removal, and 2 (1.8%) of them suffered from surgical removal. It is thought to be better to approach slowly considering the type, size and symptoms in foreign body ingestion of pediatric patients, rather than immediate and invasive removal.
Intussusception is common cause of intestinal obstruction in children. Most of intussusceptions can be treated with non-operative reduction using air or barium. However, about 10% patients need operative treatment due to failure of reduction, peritonitis, and recurrence after reduction. We introduce our experience of laparoscopic surgery for intussusception. From April 2010 to March 2013, we reviewed 57 children who diagnosed intussusception. Twelve patients underwent an operation. The cause of operation was 7 of failure of air reduction and 5 of recurrence after air reduction. Median age was 21.5 months (range: 5.0~57.7 months) and 11 children (91.7%) underwent successful laparoscopic reduction. Median operating time was 50 minutes (range: 30~20 minutes) and median hospital days was 4.5 days (range: 3~8 days). One patient had a leading point as a heterotopic pancreas and underwent bowel resection through conversion. There was neither intra-operative nor postoperative complication. Laparoscopic reduction for intussusception can bring an excellent cosmetic effect with high success rate.
The entity of negative appendectomies still poses a dilemma in chlidren. Focused computed tomography (CT) scanning has become the diagnostic test of choice in many hospitals. However, the impact of CT scans on the diagnosis in children is unknown exactly. The purpose of this study was to critically evaluate CT scans for the evaluation of acute appendicitis in children, to review utilization of this diagnostic test in our appendicitis population and to determine if diagnostic accuracy has improved. A retrospective analysis of efficacy of CT scan for diagnosis of appendicitis in children was conducted. Children undergoing appendectomy for acute appendicitis were reviewed from 2007 to 2012. Perforation and negative appendectomy (removal of a normal appendix) rates were determined by the final pathologic report. Statistical comparison were made using the χ2 test and significance was assigned at
Congenital segmental dilatation of the colon is a very rare entity of unknown etiology, characterized by a localized dilatation of a bowel segment of the colon of variable length and an abrupt transition between the normal and dilated intestine. It can affect any part of the colon, with the rectosigmoid colon being the most commonly affected site. The clinical and radiological features may resemble that of Hirschsprung disease, but differ in that the normal ganglion cells are found in the dilated and normal segment of the colon. We performed laparoscopic-assisted transanal endorectal pull-through for segmental dilatation of rectosigmoid colon in an 8-year-old boy with chronic constipation since the age of 5 months.
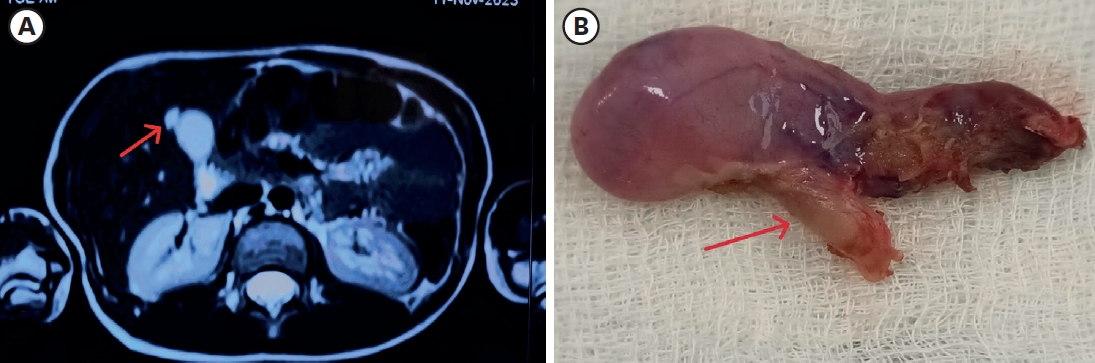
Adrenal venous malformation is an uncommon disease. We report a case of an incidentally diagnosed adrenal cystic mass during an evaluation for gastritis in a child. A 14-year-old girl admitted to our pediatric department for epigastric pain. After the gastroscopy, she was diagnosed with hemorrhagic gastritis. A 5.5 cm-sized cystic mass was incidentally found adjacent to her left adrenal gland during an ultrasound examination for evaluating her abdominal symptoms. She underwent laparoscopic surgery for the diagnosis and treatment of this cystic mass, which was confirmed to be venous malformation at pathologic diagnosis.
The application of laparoscopic techniques for the surgical management of Hirschsprung's disease is the recent trend. We described the surgical technique and postoperative long-term outcomes of the one-stage, laparoscopic-assiseted endorectal pull-through operation for Hirschsprung's disease. The technique uses three to four small abdominal ports. Laparoscopic mobilization of the sigmoid colon and rectum is performed and marginal artery-preserving colon pedicle is prepared. The rectal mobilization is performed using a transanal endorectal sleeve technique. The anastomosis is performed 0.5~1 cm above the dentate line. The age at surgery ranged from 6 days to 4 years. The average operative time was 144 minutes. Almost all of the patients passed stool and flatus within 36 hours of surgery. The average hospital stay after surgery was 6.5 days. Among 42 patients, 32 patients older than 3 years old were evaluated for function on defecation. All 32 patients have been continent, of those who needed laxatives were 11 (34.3%) due to constipation and overflow incontinence. Four children (12.5%) have remained dependent on laxatives. Laparoscopic-assisted endorectal pull-through operation for Hirschsprung's disease appears to be safe, provides the less pain, shorter time to full feeding, shorter hospital stay, and excellent cosmetic outcomes. Helping patients and parents ensure the quality of life, they should be provided with counseling, education, and longer-term follow-up care.
The purpose of this study is to analyze the early experience of the laparoscopic adhesiolysis for the intestinal obstruction due to postoperative adhesion. Seven patients were included in this study. The median age of those patients was 13, and there were 3 males and 4 females. Previous diagnosis and surgical procedure were various in seven cases, including small bowel resection with tapering enteroplasty, Boix-Ochoa fundopl ication, Ladd's procedure with appendectomy, mesenteric tumor resection with small bowel anastomosis, ileocecal resection and anastomosis, primary gastric repair, and both high ligation. A successful laparoscopic adhesiolysis was performed in one who had high ligation for inguinal hernia and had a single band adhesion. Six out of 7 (86%) cases needed to convert open surgery due to multiple and dense type of adhesion. In conclusion, laparoscopic approach with postoperative small bowel adhesion seems safe. However, it might be prudently considered because of high rates of conversion in children.
In one-stage transanal endorectal pull-through operation (TERPT) for Hirschsprung disease, preoperative evaluation by contrast enema (CE) is important tool in aspect of planning of surgical procedure as well as diagnosis. This study was to evaluate the significance of CE for identifying the extent of aganglionic bowel. A retrospective analysis was performed in 40 patients who underwent TERPT between 2003 and 2011. The authors reviewed the CE studies and their correlation with pathologic extent of aganglionosis. Total 66 contrast enemas were performed in 40 patients. Twenty patients underwent single CE, but 20 patients required multiple CEs. In single CE group, 17 had clear radiographic transition zone, but 3 had less definite transition zone. In multiple CE group, 17 patients who had equivocal finding in first or second CE had definite radiographic transition zone, but 3 patients of this group had less definite radiographic transition zones. Overall, 34 patients (85%) had clear radiographic transition zone by single or repeated CE. One (2.9%) out of 34 patients with clear radiographic transition zone had discordance between radiographic and pathologic transition zone. In contrast 4 (66.7%) out of 6 patients with equivocal radiographic transition zone had discordance between radiographic and pathologic transition zone. Observation of clear radiographic transition zone is important in preparation of TERPT, and repeated CE is helpful to reduce the discordance between radiographic and pathologic transition zone. Awareness of the possibility of discordance is also important if radiographic transitional zone is not clear.
The purpose of this study is to analyse clinical impact of specific MRI findings in liver in patients of long-term survivors after Kasai portoenterostomy (KPE). Twenty-eight patients who were underwent KPE were followed up more than 5 years. Macro-regenerative nodule (MRN) and beaded-duct dilatation (BDD) were considered as important findings in liver MRI. The association between these findings in MRI and clinical indicator, serum bilirubin level and history of cholangitis were evaluated. Sixteen patients (57.1%) were shown MRN in liver MRI. There were 14 patients(50%) whose MRI showed BDD. Serum total and direct bilirubin were 3.6mg/dL and 1.8mg/dL respectively in positive MRN group whereas 1.4mg/dL and 0.7mg/dL in negative MRN group (
Currarino syndrome is a hereditary syndrome characterized by the triad of a sacral bony defect, presacral mass and anorectal malformation. We retrospectively reviewed 13 Currarino syndrome patients who were treated in our center between 1997 and 2010. Demographic data, initial symptoms, initial diagnosis, pathologic diagnosis of presacral mass, associated anomalies and managements were analyzed. There were 8 boys and 5 girls. Four patients were diagnosed as Currarino syndrome immediately after birth with failure of passage of meconium and abdominal distension. Four patients underwent surgery for imperforate anus immediately after birth and were diagnosed as Currarino syndrome later and underwent reoperation. Three patients were diagnosed during work-up and management with of the tentative diagnosis of Hirschsprung's disease. Diagnosis of the remaining two patients was at the age of 26 months and 9 years and anorectal malformation was not associated. Twelve patients showed hemi-sacrum and one patient showed bilateral sacral subtotal agenesis. Two patients without anorectal malformation underwent presacral mass excision, untethering of spinal cord and repair of myelomeningocele. Six out of 8 patients, excluding 3 that expired or were lost to follow up, with anorectal malformation underwent colostomy, presacral mass excision, untethering of spinal cord, repair of myelomeningocele, posterior sagittal anorectoplasty and colostomy repair. One patient underwent only posterior sagittal anorectoplasty after colostomy. One waits the scheduled operation only with Hegar dilatation. Pathologic examation of presacral masses showed myelomeningoceles in 4 patients, lipomyelomeningoceles in 3 patients and dermoid cyst in one patient. Teratoma was combined in 2 patients. Eight patients needed neurosurgical operation for spinal cord problems. Seven patients had urologic anomalies and two of them underwent operation. Currarino syndrome should be considered as a differential diagnosis in pediatric patients with abdominal distension, constipation and anorectal malformation. For proper evaluation and treatment, a multi-disciplinary approach is recommended.
Thyroglossal duct cysts (TGDC) are the most common type of congenital developmental anomaly encountered in the anterior midline of the neck in childhood. The aim of the study was to evaluate the clinical characteristics of TGDC and identify any factors that could be related to recurrence after surgery. This study consisted of a retrospective chart review of 45 patients treated at Kyungpook National University Hospital for TGDC between 1990 and 2008. All records were reviewed for age and sex, length of history, presentation, diagnostic methods, sizes and locations of cyst, surgical management, histopathology of the lesion and recurrences. The statistical analysis of risk factors for recurrence was made using the Fisher's exact test with a significance level of p < 0.05. The male to female ratio was 2.2:1 with a male preponderance. The mean age at operation was 5 years and 2 months (4 months – 17 years). The most common presenting symptom was a nontender cervical mass (78%). Most TGDC were found in the midline position. Twenty four were infrahyoid, 17 were hyoid, and 4 were suprahyoid level. Forty one (91%) patients received the Sistrunk operation, and 4(9%) patients received cyst excision. Postoperative a seroma developed in six patients in the early postoperative days. There were a total of 3(6.6%) recurrences, 2 in patients who had excision only and in one patient who had the Sistrunk operation. Univariate analysis for risk factors with recurrence showed that there was no statistical relationship between the presence of preoperative infection and the development of recurrence. The removal of hyoid bone along with TGDC was a statistically significant risk factor for recurrent disease. This study suggests that the Sistrunk operation is the treatment of choice for TGDC in order to reduce recurrence.
We analyzed the clinical characteristics and outcome of ileocecal and small bowel intussusceptions (ICI and SBI) in the pediatric patients. From August 2003 to July 2010, 144 children with intussusception were included in this study. We retrospectively reviewed the clinical records and imaging study findings. A total of 86 children with ICI and 58 children with SBI were diagnosed. Children with SBI were older than ICI (36.6±24.6 months vs. 24.2±21.6 months, p=0.002). Typical symptoms such as irritability, abdominal mass, bloody stool were more frequent in ICI than SBI (p<0.05) patients. In the ICI group, intussusceptums were reduced with air reduction (84.5%), surgery (17.4%), and spontaneity (1.2%). All patients in the SBI group were reduced spontaneously. SBI occurred in older age and was reduced spontaneously more frequently than ICI. Conservative management with close observation with follow-up by ultrasonography is recommended for SBI.
Meconium obstruction (MO) in neonates arises from highly viscid meconium and the poor motility of the premature gut. Recently the incidence of the MO in neonates has been increasing, but, the diagnosis and treatment of this disease have not yet been clarified. Between March 2004 and April 2010, 24 neonates were treated for MO at Severance Children's Hospital. Their clinical characteristics and treatment were reviewed retrospectively. Twenty neonates were diagnosed with MO and 4 neonates were diagnosed with Hirschsprung's disease (HD). The mean birth weight and gestational age of the 20 neonates with MO were 1.45±0.90kg and 31.1±4.6 weeks, respectively. Thirteen neonates (65%) diagnosed with MO weighed less than 1.5kg and 10 neonates (50%) weighed less than 1kg. Half of the neonates with MO were treated by non-operative methods and the other half were treated by operative methods. Compared with the group that weighed over 1.5kg, the group that weighed less than 1.5kg were more frequently operated upon (61.5% vs. 28.5%), and contrast enemas were performed later and more frequently. Also the group that weighed less than 1.5kg had a higher mortality rate (15.4% vs. 0%). Three of the four neonates with HD were diagnosed with long-segment aganglionosis. In conclusion, MO occurred in very low birth weight neonates more often and must be differentiated from HD. Also, MO in very low birth weight neonates should be treated with special attention due to more a complicated clinical course.
The aim of this study is to review our clinical experience with patients with Hirschsprung's disease (HD) Medical records of 39 children who underwent definitive surgery for HD at Inha University Hospital from September 1996 to June 2008 were analyzed by age at presentation, sex, gestational age, birth weight, clinical presentation, diagnostic tools, level of aganglionosis, surgical procedures, postoperative complications, and postoperative bowel function. Twenty-five patients (64.1%) were males and 14 (35.9%) were females. Thirty patients (76.9%) were diagnosed and treated in the neonatal period. The transitional zone was at the rectosigmoid region in 89.7%. Twenty-seven patients (69%) were treated by preliminary colostomy or ileostomy. Twenty-four patients had the Duhamel operation, 6 patients anorectal myectomy, and 9 patients had transanal endorectal pull-through (TEP). Five of 9 patients who had the TEP procedure did laparoscopic assistance. Postoperatively, seventeen patients (83%) passed stool once or more times per day and 3 patients had stool soiling. This study demonstrated that the majority of the patients had good results. To determine which treatment is most effective comparative review by operation method would be required.
Pulmonary sequestration (PS) is a rare congenital malformation of the lower respiratory tract. The anomaly is characterized by absence of communication with the tracheobronchial tree and isolated blood supply from an anomalous systemic vessels. With the utilization of antenatal ultrasound, the diagnosis of asymptomatic neonatal PS has increased. Treatment options include observation, arterial embolization and surgical resection. The aim of the present study is to review the clinical course of PS and to share our experience with thoracoscopic resection. A total of 96 patients with PS were treated at Asan Children's Hospital between 1999 and 2010. The diagnosis of PS was established by CT in the cases managed by observation or embolization, and by tissue pathology in the surgical cases. Medical records and radiographic images were retrospectively reviewed. Thirty-nine patients were managed by embolization and 30 patients by surgery. The remaining 27 patients have been under observation without any procedures. Among 27 observation patients, 1 patient regressed completely and 10 patients were lost to follow up. Of the 39 embolizations patients, 2 had their lesion regress and sepsis was suspected after embolization. In 1 patient, the microcoil migrated to the iliac artery during the embolization procedure, and another patient developed renal abscess caused by renal artery embolization. Among 30 surgical cases, resection by thoracotomy was performed in 27 at the Department of Thoracic Surgery, and thoracoscopic resection in 3 at the Division of Pediatric Sugery. Only one wound complication ocurred. We conclud that surgical excision should be recommended for pulmonary sequestration, whether the sequestration is symptomatic or not because of the risk of infection, the low rate of natural regress, poor compliance, severe complications after embolization, and to exclude other pathology. In summary, thoracoscopic resection of the pulmonary sequestration is feasible, efficacious, safe and cosmetically superior even in neonatal period.
Unreduced small bowel intussusception requires operative treatment although the rate of spontaneous reduction is 60 to 70%. The aim of this study is to compare clinical characteristics and outcome between spontaneous reduction and operation group and to analyze factors related to decisions to treat small bowel intussusceptions. The records of 25 patients with small bowel intussusceptions treated in Seoul National University Children's Hospital from January 1999 to August 2009 were reviewed respectively. Spontaneous reduction group (n=12, 48%) had signs and symptoms of vomiting, abdominal pain, currant jelly stool, abdominal distension, fever, increased CRP but no rebound tenderness. One of them had been diagnosed with Henoch-Schonlein purpura and no one displayed pathologic leading point by image study. Operation group (n=13, 52%) consisted of patients who had primary surgery. Their signs and symptoms were similar to spontaneous reduction group. Seven of them had underlying diseases such as Crohn' disease, ALL, Lymphoma, Peutz-Jeghers syndrome (n=3), post-transplanted state of liver and 2 of them displayed Peutz-Jeghers polyp and Meckel's diverticulum as pathologic leading point by preoperative ultrasonography. Mean relieve interval (interval between onset of symptoms and reduction/operation) was 1.78 days in spontaneous reduction group and 2.25 days in operation group (p=0.341). Seven of operation group had manual reduction and 6 out of 7 received segmental resection of the small bowel. No one of them underwent manual reduction and all of them underwent segmental resection were found to have pathologic leading points [Peutz-Jeghers polyp (n=3), Meckel's diverticulum (n=2), lymphoma (n=1)] during operation. In conclusion, 48% of small bowel intussusceptions resolved spontaneously. Patients' symptoms and relieve intervals were not related to the operative decisions. We therefore recommend significant factors for determining treatment plan such as change of clinical symptoms, underlying disease or pathologic leading point by imaging.
Air reduction is a safe, effective, and fast initial treatment for pediatric intussusception. There is low dose radiation exposure. Factors affecting outcomes of air reduction were analyzed by reviewing the clinical features and results of treatment. A total of 399 out of 485 patients with pediatric intussusceptions were treated at the Seoul National University Children's Hospital from 1996 to 2009. All of the patients received air reduction as the first line of treatment. Clinical features such as gender, age, seasonal variation, symptoms, signs, types, pathologic leading point, and treatment results including success rate, complication, recurrence, NPO time, and duration of hospitalization were reviewed. The Pearson chi-square, student T-, and logistic regression tests were used for statistical analysis. P-value less than 0.05 was considered to be statistically significant. The prevalent clinical features were: male (65.4%), under one-year of age (40.3%), ileocolic type (71.9%), abdominal pain (85.4%), and accompanying mesentery lymph node enlargement (2.2%). The overall success rate for air reduction was 78.4% (313 of 399 patients), and the perforation rate during reduction was 1.5%. There were 23 recurrent cases over 21.6 months. All were successfully treated with re-do air reduction. Reduction failures had longer overall NPO times (27.067hrs vs. 43.0588hrs; p=0.000) and hospitalization durations (1.738d vs. 6.975d; p=0.000) compared to the successful cases. The factors affecting success rates were fever (p=0.002), abdominal distension (p=0.000), lethargy (p=0.000) and symptom duration (p=0.000) on univariate analysis. Failure rates were higher in patients with symptom durations greater than 24 hours (p=0.023), and lethargy (p=0.003) on multivariate analysis. Air reduction showed high success rates and excellent treatment outcomes as the initial treatment for pediatric intussusception in this study. Symptom duration and lethargy were significantly associated with reduced success rates.
Pancreaticoduodenectomy is the treatment of choice for adult periampullary lesions. However there has been no studies on the clinical outcomes of pancreaticoduodenectomy in children. To evaluate the clinical outcomes, records of 13 patients who underwent pancreaticoduodenectomy, from 1989 to 2009, at Seoul National University Children's Hospital were reviewed. Mean follow up period was 83 (2-204) months, the male to female ratio was 1:3.3, and the mean age was 11 (2-14) years. Ten patients underwent PPPD and 3 patients had Whipple's operation. The postoperative diagnosis included solid pseudopapillary tumor (9), cavernous hemangioma (1), pseudocyst (1), benign cyst (1), pancreatic disruption (1). Two patients developed postoperative adhesive ileus and among them one patient required operative intervention. Four patients required pancreatin supplementation due to steatorrhea and other gastrointestinal symptoms. There were no postoperative mortality during the follow up period and no evidence of recurrence in SPT patients. This study demonstrates that the pancreaticoduodenectomy procedure in children is not only feasible but also safe, with no mortality and an acceptable complication rate.
We report a case of nonfunctioning neuroendocrine tumor of the pancreas in a 15-year-old girl who presented with back pain. On physical examination, there was mild tenderness in the left upper quadrant of the abdomen. The patient had no pancreatic hormone-associated symptoms. An abdominal ultrasonography showed a well-demarcated hypervascular solid mass with calcification in the tail of the pancreas. An abdominal computed tomography scan showed a 6x5cm sized well-encapsulated enhancing solid mass with cystic component in the tail of the pancreas. Distal pancreatectomy was performed. Pathology revealed awell- differentiated nonfunctioning low grade malignant neuroendocrine tumor of the pancreas. The postoperative course was uneventful.
The purpose of this study was to determine the success rate of air reduction as the primary treatment of intussusception and whether the success of air reduction could be predicted by plain x-ray. The authors reviewed the medical records of 54 consecutive patients diagnosed with intussusception from Jan 2005 to Dec 2007 at the Department of Surgery, Masan Samsung Hospital. The natures of symptoms and findings of plain abdominal radiography performed in the emergency department (ED) were reviewed. Air reduction failed more frequently (26.3%) in patients who visited ED more than 24 hours after symptom onset (p=0.009). The mean duration of symptom for operated patients was longer than air reduction group (p=0.01). Also, 3/4 of patients having localized distension of small bowel in the left upper quadrant abdomen had unsuccessful air reduction (p=0.002). In conclusion, the time interval from symptom onset to arrival at ED and localized distension of small bowel in the left upper quadrant abdomen significantly increased the failure rate of air reduction.
Choledochal cyst is a congenital dilatation of the bile duct. Intrahepatic bile duct dilatation of type IVa by Todani's classification at the time of diagnosis resolved spontaneously after cyst excision and hepaticojejunostomy in many cases. It should be distinguished from the true cystic dilatation of the intrahepatic ducts, which tends to persist, albeit after some regression. We therefore studied postoperative intrahepatic duct dilatation changes in choledochal cyst. A total of seventy-six choledochal cysts were managed at the Division of Pediatric Surgery, Department of Surgery, Samsung Medical Center from May 1995 to December 2005. The ratio of males to females was 1:2.8. Preoperative radiologic diagnosis by Todani's classification was Type I (n=52, 68.4 %), II (n=1, 1.3 %), IVa (n=23, 30.3 %). Among fifty-five patients with intrahepatic bile duct dilatation we were able to follow up forty-eight by ultrasonography. Twenty-two patients were type IVa, and twenty-six patients were type I and showed intrahepatic duct dilatation. Mean follow-up duration was 35.3 months (9~105 months). Complete regression of dilated intrahepatic duct was observed in fifteen patients of type IVa and twenty-four patients of type I. Incomplete regression of dilated intrahepatic duct was observed in six patients in type IVa and two patients in type I. Only one patient in type IVa showed no change in ductal dilatation during a follow-up period of 15 months. We conclude that true type IVa is much less frequent than what was diagnosed preoperatively by imaging study. Therefore in type IVa patients who are diagnosed preoperatively the decision to perform liver resection should be carefully considered. Postoperative long term follow up of choledochal cyst with intrahepatic bile duct dilation is needed.
Colorectal cancer is extremely rare in children. Unlike adult colorectal cancer, the overall prognosis of colorectal cancer in children is poor. Delayed diagnosis, advanced stages of the disease at presentation, and mucinous type of histology are the major determinants of poor outcome in childhood. A 13-year-old boy with abdominal pain visited our hospital. Physical examination andabdominal ultrasonography identified acute appendicitis with perforation. He underwent appendectomy and then the pathologic findings revealed mucinous adenocarcinoma. The cancer was located at the transverse colon and had metastases on peritoneal wall at 2nd laparotomy. Extended right hemicolectomy was performed. He underwent palliative chemotherapy. After 4 months later, hepatic metastasis and aggravated peritoneal seedings developed. He died of renal failure and pneumonia 13 months after operation. We need to have a high index of suspicion for the possibility of a malignant colorectal tumor in any childhood case with nonspecific signs and symptoms.
The survival rate for rhabdomyosarcoma (RMS) has significantly improved after the introduction of combined multimodality treatment. We report the 20-year treatment outcome of pediatric rhabdomyosarcoma in a single institution. The medical records of 16 patients treated for rhabdomyosarcoma between December 1986 and August 2007 at the Department of Pediatric Surgery, Seoul National University Children's Hospital, were retrospectively reviewed. Mean age at diagnosis was 7.1 years (range: 1.3-14.2 years). Retroperitoneum was the most common primary site (n=7, 43.8%), and embryonal type was predominant (n=11, 6%). Before the treatment, most patients were in advanced TNM stage (stage III 50%, IV; 25%). The patient distribution according to the Intergroup Rhabdomyosarcoma Study Clinical Grouping System (IRS-CGS) was as follows; Group I 31.3%, Group II 12.5%, Group III 31.3% and Group IV 25%. Patients were classified into three groups according to the extent of resection of the primary tumor; complete resection (CR, n=5; 31.3%), gross total resection (GTR, n=7; 43.8%) and incomplete resection (IR, n=4; 25%). Recurrence was observed in 9 patients (56.3%) while there was no recurrence in CR patients. All patients with recurrence were identified as moderate or high-risk according to the IRS-V Risk Group. Pre-treatment TNM stage of RMS in our institution was advanced with aggressive clinical feature, however post-surgical conditions according to IRS-CGS were similar to the previous reports by IRS. This suggests that down-staging of IRS-CGS was achieved with multimodality treatment with CR or GTR. It also suggests that complete resection is the most important prognostic factor in the treatment of RMS in children. Patients classified as moderate or high-risk need close follow-up due to high recurrence rate. In case of localized recurrence, better outcome may be achieved with multimodality treatment including limited surgery.

