This study aimed to compare the outcomes of open fundoplication (OF) and laparoscopic fundoplication (LF) in children with gastroesophageal reflux disease (GERD).
We retrospectively reviewed the electronic medical charts of pediatric patients who underwent fundoplication for GERD between January 2005 and May 2018 at the Korean tertiary hospital. Patient characteristics, operation type, associated diagnosis, operation history, neurologic impairment, postoperative complication, recurrence, and operation outcomes were investigated. The Mann-Whitney U test or Student's t-test was used to evaluate continuous data as appropriate. The χ2 test was used to analyze categorical data.
A total of 92 patients were included in this study; 50 were male and 42 were female. Forty-eight patients underwent OF and 44 patients underwent LF. Patient characteristics, such as sex ratio, gestational age, symptoms, neurological impairment, and history of the previous operation were not different between the two groups. A longer operative time (113.0±56.0 vs. 135.1±49.1 minutes, p=0.048) was noted for LF. There was no significant difference in operation time when the diagnosis was limited to only GERD, excluding patients with other combined diseases. Other surgical outcomes, such as intraoperative blood loss, transfusion rate, hospital stay, and recurrence rate were not significantly different between the 2 groups. The complication rate was slightly higher in the OF group than in the LF group; however, the difference was not significant (20.8% vs. 11.4%, p=0.344).
LF is as safe, feasible, and effective as OF for the surgical treatment of GERD in children.
Single-port laparoscopy-assisted surgery is being performed for various operations in pediatric patients recently. The aims of this study were to prove the safety and find well-matched indications of small bowel resection using single-site umbilical laparoscopic surgery (SSULS).
From 2011 to 2016, 29 pediatric patients underwent SSULS. Medical records were retrospectively reviewed.
A total of 29 patients were included and 30 SSULS were performed in this study. The mean age at operation was 5.7 years, and the mean weight was 21.9 kg. Meckel's diverticulum was the most common indication for SSULS, followed by small bowel intussusception due to leading point mass, small bowel duplication, and Crohn's disease. In most cases, estimated blood loss was negligible except in Crohn's disease with severe inflammation. While answering post-discharge questions about scars, most parents responded that they were satisfied with the postoperative wound.
SSULS is a useful operation to try even for surgeons who do not have advanced laparoscopic skills. Complication rates of single-port operations do not differ from those of conventional laparoscopic operations. Most lesions of the small bowel could be indications of SSULS. Careful attention is required when performing SSULS in patients with Crohn's disease.
Citations

Total proctocolectomy with ileal pouch-anal anastomosis (T-IPAA) in childhood is a surgical procedure mainly applied to familial adenomatous polyposis (FAP) or ulcerative colitis (UC), but it can be applied to non-FAP/non-UC disease (NFNU). Studies regarding the role of T-IPAA who underwent the operation in childhood, especially in terms of long-term gastrointestinal function, complications, and quality of life (QOL) are limited. The aim of this study was to evaluate the characteristics of patients receiving T-IPAA and to compare their bowel function outcomes and QOL.
Patients aged ≤18 years at the time of T-IPAA were included. Their medical records were retrospectively reviewed. Krickenbeck classification, Cleveland Clinic Incontinence (CCI) score, 36-item Short-form Health Survey Questionnaire, and Gastrointestinal Quality of Life Index were used for the evaluation of bowel function and QOL. The median follow-up period was 9.8 years.
Of the 25 patients, 9 had FAP, 9 had UC, and 7 had NFNU. NFNU include 3 of Hirschsprung disease, 2 of intestinal neuronal dysplasia, and 2 of imperforate anus. The median age at T-IPAA was 17.8, 14.2, and 9.3 years for FAP, UC, and NFNU, respectively (p=0.001). Bowel function was satisfactory in terms of voluntary bowel movement (VBM), soiling, and constipation. VBM and constipation were not different between the groups, but soiling was most in NFNU (100%, p=0.047). However, QOL was best in the NFNU group in surveys (p=0.034 and 0.004, respectively).
T-IPAA could be safely applied not only for FAP and UC but also for other diseases in selective cases, with caution.
Citations

Thyroid cancer is a rare disease in pediatric population, but its incidence rate is increasing. The aim of this report is to present a single institution experience of pediatric thyroid cancer and to identify clinical features, predisposing factors, and postoperative course of pediatric thyroid cancer.
We retrospectively reviewed 35 pediatric patients who underwent operation due to thyroid cancer at Seoul National University Children's Hospital between May 1997 and January 2017. The median follow-up period was 70 months (range, 5–238 months).
The mean age at operation was 12.0±5.91 years and 27 patients were female. The underlying conditions in patients included history of chemoradiotherapy for previous other malignancies (n=4), hypothyroidism (n=3), history of chemotherapy (n=2), family history of thyroid cancer (n=1) and history of radiation therapy (n=1). The initial symptoms were palpable neck mass (n=21) and incidental findings (n=11). Total thyroidectomy (n=30) or unilateral lobectomy (n=5) were performed. There were 15 postoperative complications including transient hypocalcemia in 14 patients and Horner's syndrome in 1 patient. The most common pathologic cell type was papillary thyroid cancer (n=29). Extrathyroid extension and lymph node invasion were found in 25 patients and 27 patients, respectively. Thirteen patients showed multifocality. During follow-up period, 5 patients underwent additional operation because of tumor recurrence in lymph nodes. Lung metastasis was detected in 3 patients at the time of diagnosis and in 3 patients during follow-up period. The mortality rate was zero and mean disease-free survival was 83.7±47.9 months.
Pediatric thyroid cancer has lower mortality rate and recurrence rate as seen in this study despite the advanced stage at diagnosis. A thorough follow-up of patients with an underlying condition such as history of chemoradiotherapy and understanding new pediatric guideline can be helpful to maximize patients' survival and prognosis.
Minimally invasive surgery (MIS) in abdomen and thorax has been widely accepted for pediatric diseases. Thoracoscopic surgery has the advantage of less pain, better cosmetic outcomes and less musculoskeletal sequelae in comparison to open surgery. We would like to share our initial experience with thoracoscopic surgery performed by one pediatric surgeon.
We performed a retrospective review of patients who underwent thoracoscopic surgery by one pediatric surgeon between April 2010 and August 2017 in Department of Pediatric Surgery, Seoul National University Children's Hospital.
There were totally 18 cases; 8 cases for esophageal atresia, 3 cases for congenital diaphragm hernia, 2 cases for diaphragm eventration, 2 cases for esophageal duplication cyst, 2 cases for pleural mass and 1 case for esophageal bronchus. At the operation, median age was 9.5 months (range, 0-259 months) and median body weight was 9.4 kg (range, 1.9-49.4 kg). Median operative time was 157.5 minutes (range, 45-335 minutes). There was no case of open conversion and 2 cases of minor leakage at anastomosis site in case of esophageal atresia. Median follow-up month was 5 months (range, 0-87 months). During follow-up, 4 cases of esophageal atresia showed anastomosis site narrowing and average 2.5 times (range, 1-5 times) of esophageal balloon dilatation was done.
We performed thoracoscopic surgery in case of esophageal, diaphragm disease and pleural mass. Thoracoscopic surgery can be an effective and feasible option of treatment for well-selected pediatric patients of intra-thoracic disease including esophagus, diaphragm and mediastinum disease.
Hepatocellular carcinoma (HCC) is a rarely occurring disease in the pediatric population. We report our center's experience of management of HCC in children and adolescents.
From 1996 to 2012, 16 patients aged 18 or younger were diagnosed with HCC at our center. The medical records of these 16 patients were retrospectively reviewed.
There were 9 boys and 7 girls. Median age at diagnosis of HCC was 14.5 years. All patient had pathologically confirmed diagnosis of HCC. Three patients had distant metastasis at the time of HCC diagnosis. Eight patients were surgically managed, including 4 liver resections, 3 liver transplantations, and 1 intraoperative radiofrequency ablation. The remaining 8 patients received systemic chemotherapy. Overall, 6 patients are alive at median 63.6 months after diagnosis of HCC. All survivors were surgically managed patients.
HCC is a rare disease occurring in childhood. Patients with systemic disease have poor outcome. Liver transplantation may be a good option for treatment of pediatric HCC.
Lymph node enlargement is a common finding in children suggesting normal or benign. Palpable nodes which are large, hard or fixed must be examined carefully to rule out malignant diseases. In this case, a 15-year-old boy presented to our hospital to inspect the palpable mass at his post-auricular area being found 2 months ago. It was diagnosed as nodal marginal zone lymphoma (NMZL) through excisional biopsy and immunohistochemistry. NMZL is very rare, especially in children and young adults, but occurs locally in most cases with a good prognosis compared to adults. We described a rare case of NMZL diagnosed in adolescent.
Number of pediatric cholecystectomy has been recently showing a gradually increasing trend. The purpose of this study was to investigate the clinical features of patients who underwent pediatric cholecystectomy, and the latest trend in cholecystectomy.
In the present study, we conducted a retrospective chart review on 47 patients who had undergone cholecystectomy at a single center. The entire patient population was divided into two groups, according to the time of cholecystectomy (early group, January 1999 to December 2006; late group, January 2007 to August 2014).
The comparison between the early and late groups showed that the number of cholecystectomy increased from 13 to 34 cases representing a 2.6-fold increase. The mean patient age also increased from 5.94±4.08 years to 10.51±5.57 years (p=0.01). Meanwhile, laparoscopic surgery also increased from 15.4% to 79.4%, respectively (p<0.001). However, sex, mean body mass index, comorbidities, indications of cholecystectomy, and previous total parenteral nutrition were not statistically significant.
The results of this study showed that pediatric cholecystectomy cases are increasing, particularly in the 10 to 19 years age group and laparoscopic cholecystectomies are also being performed at an increasing rate. When the patients were compared according to the time of cholecystectomy, there were no differences in other risk factors or indications for cholecystectomy.
Citations

This is a survey on congenital posterolateral diaphragmatic hernia, conducted by Korean Association of Pediatric Surgeons (KAPS). A registration form for each patient during the 5-year period between 2010 and 2014 and a questionnaire were sent to each member. Twenty-six members in 16 institutions returned completed forms. Total patients were 219. Prenatal diagnoses were done in 181 cases (82.6%). Preoperative mortality was 11.4%. Minimal invasive surgery was done in 61 cases (31.8%). Risk factors related with death were Apgar score, oxygenation index, preoperative pH and bicarbonate, O2 saturation, the presence of hernia sac, and the size of defect. The neonatal survival and 1-year survival of total patients were 77.6% and 75.3%.
Citations

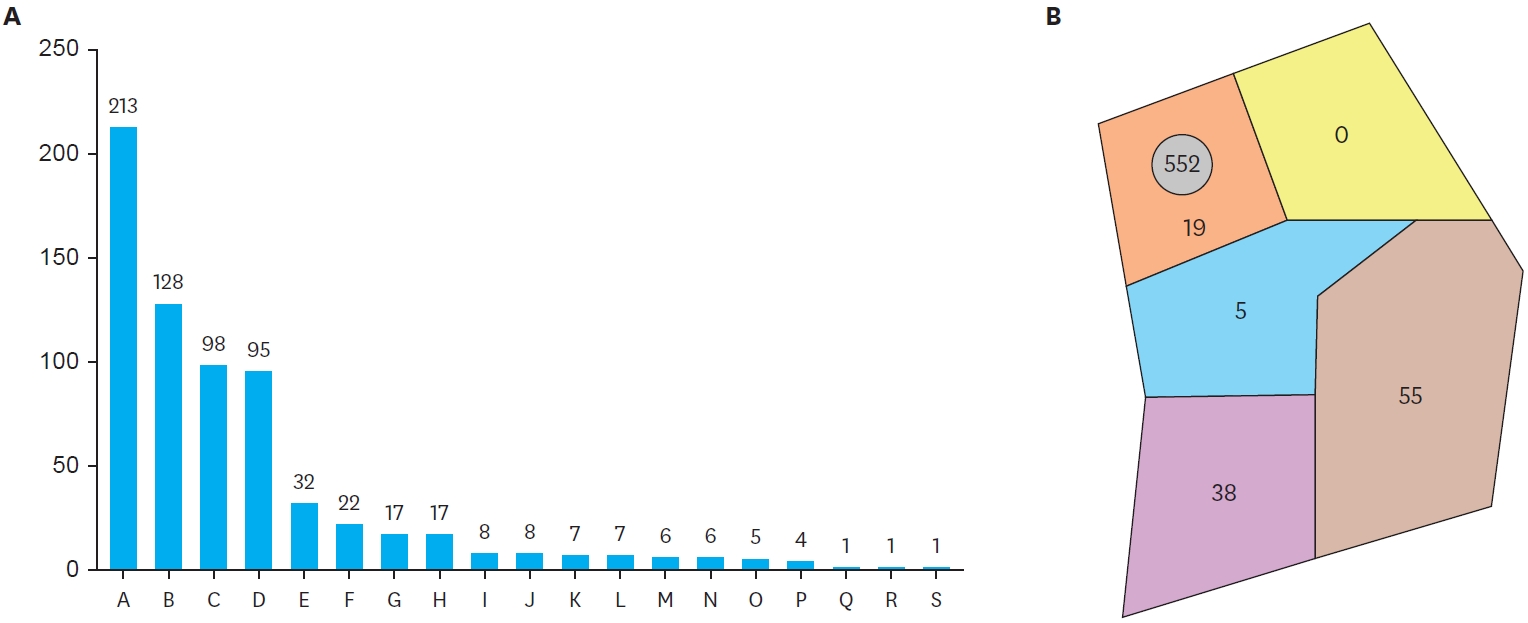
Minimal invasive surgery (MIS) has rapidly gained acceptance for the management of a wide variety of pediatric diseases. A questionnaire was sent to all members of the Korean Association of Pediatric Surgeons. Thirty one members (25.4%) took part in the survey that included data for the year 2012: demographic details, opinion regarding minimal invasive surgery and robotic surgery, spectrum of minimally invasive operations, and quantity of procedures. 48.4% of the respondents had more than 10 years experience, 35.5% less than 10 years experience, and 16.1 % had no experience. The respondents of the recommend MIS and perform MIS for surgical procedures are as follow; inguinal hernia (61.3%), simple appendicitis (87.1%), complicated appendicitis (80.6%), reduction of intussusceptions (83.9%), pyloromyotomy (90.3%), fundoplication (96.8%), biopsy and corrective surgery of Hirschsprung's disease (93.5%/90.3%), imperforate anus (77.4%), congenital diaphragmatic hernia (80.6%), and esophageal atresia (74.2%). The MIS procedures with more than 70% were lung resection (100%), cholecystectomy (100%), appendectomy (96.2%), ovarian torsion (86.7%), fundoplication (86.8%), hiatal hernia repair (82.6%), and splenectomy (71.4%). The MIS procedures with less than 30% were congenial diaphragmatic hernia reapir (29.6%), esophageal atresia (26.2%), correction of malroatation (24.4%), inguinal hernia repair (11.4%), anorectal malformation (6.8%), Kasai operation (3.6%).
Citations

Laparoscopic surgery has become popular in the past few decades, owing to less postoperative pain, fast recovery, and better cosmetic outcomes. The laparoscopic approach has been employed in pediatric surgery for the same reasons. After the first attempts of single incision laparoscopic appendectomy in pediatrics in 1998, single incision laparoscopic surgery (SILS) has recently been proven to be safe and feasible for the pediatric population. However, limitations have been reported for SILS, such as the wide learning curve, compared to standard laparoscopic surgery, and the restricted number of hospitals with surgical training programs including SILS. In this study, we intend to present our initial experiences with SILS in children, and to describe the technique, instruments used, and outcomes. This is a retrospective study of 71 pediatric patients who underwent SILS, at a tertiary medical center, between September, 2012 and August, 2013. Electronic medical records were reviewed for demographics, type of procedure, operation time, use of additional ports, conversion to open surgery, complications and hospital stay. Additional ports were inserted in 4 cases, for the purpose of traction. Postoperative complications were noted in 13 cases, which were mostly related to wound inflammation or formation of granulation tissue. According to our analyses, patients with complications had significantly longer use and more frequent use of pain killers. Notwithstanding the small sample size, many of the procedures performed in pediatric patients seem to be possible with SILS.
Citations

Ketamine is a safe and effective drug for pediatric anesthesia, sedation and analgesia. We hoped to identify that surgeons could operate a pediatric hernia with the ketamine anesthesia without general anesthesia. The study was a consecutive case series of 2230 inguinal hernia patients aged 1 months to 17 years in a Joo's day-surgical clinic during 11-year period. The patients had pediatric inguinal hernia surgery without general anesthesia under the day-surgery system. We retrospectively analyzed the medical record of patients who were registered with the Diagnosis Related Group (DRG) system. All patients received ketamine (5mg/kg) and atropine (0.01mg/kg) intramuscularly before surgery. After anesthesia, we injected 1~2% lidocaine (Less than 5ml) subcutaneously at the site of incision and started operation. The surgical method was the high ligation method of the hernia sac.) In total 2230 patients, male were 1756 and female were 474. 2076 patients were a unilateral inguinal hernia at the time of surgery and 154 were bilateral hernia patients. Less than three months, depending on the age of the patients was 391, and less than 12 months the patient was 592 people (26.5%). After surgery, there were no accidents or long term complications associated with ketamine anesthesia. We think the surgeon can safely do the pediatric inguinal hernia surgery using ketamine and lidocaine without anesthesiologist through 11 years of our surgical experiences.
Pediatric liver transplantation has evolved into a definite and effective therapeutic modality for various liver diseases in the pediatric patient. During the last 25 years, liver transplant outcomes in Korea have reached international standards and Korea has become the leader in living-donor liver transplantation. This review will present the cumulative outcomes of pediatric liver transplantation performed in Korea and will focus on other issues of interest involving pediatric liver transplant recipients, especially in the field of immunosuppression and post-transplant lymphoproliferative disease.
Citations

Meckel's diverticulum (MD) has various clinical presentations and due to the limitation of imaging studies, pre-operative diagnosis is a challenge in pediatric patients. Recently, laparoscopic exploration has been suggested as a favorable method for the diagnosis and treatment of complicated MD. We investigated the results of laparoscopic-assisted surgery compared with open technique. We retrospectively studied patients who underwent resection of complicated MD at our institute from 1997 to 2010 and compared 11 treated by laparoscopic-assisted diverticulectomy (LD) with 11 treated by open diverticulectomy (OD) for complicated MD. Operation time was not significantly different in the two groups. Hospital stay and time to diet were not significantly different. Two patients were re-admitted due to mechanical ileus in the LD group. None of patients in either group needed re-operation. Considering the possibility of false-positive results with imaging studies and the cosmetic benefit, laparoscopic-assisted surgery is a safe and effective treatment modality to diagnose and treat complicated Meckel's diverticulum.
Citations

Unreduced small bowel intussusception requires operative treatment although the rate of spontaneous reduction is 60 to 70%. The aim of this study is to compare clinical characteristics and outcome between spontaneous reduction and operation group and to analyze factors related to decisions to treat small bowel intussusceptions. The records of 25 patients with small bowel intussusceptions treated in Seoul National University Children's Hospital from January 1999 to August 2009 were reviewed respectively. Spontaneous reduction group (n=12, 48%) had signs and symptoms of vomiting, abdominal pain, currant jelly stool, abdominal distension, fever, increased CRP but no rebound tenderness. One of them had been diagnosed with Henoch-Schonlein purpura and no one displayed pathologic leading point by image study. Operation group (n=13, 52%) consisted of patients who had primary surgery. Their signs and symptoms were similar to spontaneous reduction group. Seven of them had underlying diseases such as Crohn' disease, ALL, Lymphoma, Peutz-Jeghers syndrome (n=3), post-transplanted state of liver and 2 of them displayed Peutz-Jeghers polyp and Meckel's diverticulum as pathologic leading point by preoperative ultrasonography. Mean relieve interval (interval between onset of symptoms and reduction/operation) was 1.78 days in spontaneous reduction group and 2.25 days in operation group (p=0.341). Seven of operation group had manual reduction and 6 out of 7 received segmental resection of the small bowel. No one of them underwent manual reduction and all of them underwent segmental resection were found to have pathologic leading points [Peutz-Jeghers polyp (n=3), Meckel's diverticulum (n=2), lymphoma (n=1)] during operation. In conclusion, 48% of small bowel intussusceptions resolved spontaneously. Patients' symptoms and relieve intervals were not related to the operative decisions. We therefore recommend significant factors for determining treatment plan such as change of clinical symptoms, underlying disease or pathologic leading point by imaging.
This study is a retrospective analysis of 1244 cases of the inguinal hernia in children under the age of fifteen years who were operated at the department of pediatric surgery, Inje University Busan Paik Hospital from March, 1997 to February, 2007. The ratio of male to female was 3.6:1. The type of hernia was indirect in all of the cases. The hernia was on the right side in 656 cases (53.9 %), left side in 467 cases (37.5 %), and bilateral in 121 cases (9.7 %). The hernia presented most frequently in infants under age 12 months; 364 cases (29.2 %). Fifty-nine cases (21.7 %) were in female and 305 cases (31.3 %) in male. There were 428 cases (33.6 %) in 1-3 years age group, 295 cases (23.7 %) in 4-6 years, 112 cases (9.0 %) in 7-9 years, 39 cases (3.1 %) in 10-12 years and 16 (1.2 %) in 13-15 years. The content of hernia sac was small bowel (59 %), omentum (31 %) in males and the ovary and tube (54 %) and small bowel (26 %) in female. The incidence of combined operation at the time was 3.2 %, and consisting of orchiopexy (67.5 %), frenulotomy (12.5 %), appendectomy (10 %), circumcision (5 %), and fistulotomy (5%). The incidence of combined disease was 2.8 % and consisting of undescended testis, Hirschsprung's disease, idiopathic hypertrophic pyloric stenosis, imperforate anus, and congenital heart disease. After unilateral inguinal hernia repairs, contralateral hernias developed in 34 patients. The laterality of the primary site of hernias were left in 19 cases (55.8 %), and right 15 cases (44.1 %). The 936 cases (75.2 %) were operated under general anesthesia; Mask bagging 663 cases (53.2 %), endotracheal intubation 257 cases (20.6 %), and laryngeal mask 16 cases (1.2 %). The remainder 308 cases (24.7 %) were operated under regional caudal anesthesia.
Citations

Prophylactic contralateral exploration in unilateral inguinal hernia repair is still controversial. The purpose of this study is to analyze the contralateral incidence of hernia and to verify the necessity of the simultaneous contralateral exploration. Infants and children operated on for inguinal hernia or hydrocele at the Department of Pediatric Surgery of Asan Medical Center from January 1996 to December 2005 were analyzed retrospectively. A total of 383 patients (9.8 %) out of 3,925 patients underwent a simultaneous bilateral operation. A total of 222 patients (6.2 %) out of 3,542 patients underwent a secondary metachronous contralateral operation after primary unilateral inguinal hernia or hydrocele repair. Because simultaneous bilateral operation cases included true bilateral inguinal hernia or hydrocele, and unilateral hernia and simultaneous contralateral exploration, bilateral incidence of inguinal hernia and hydrocele could be maximally considered as 15.4% (605 patients). Therefore, the prophylactic contralateral exploration in unilateral inguinal hernia or hydrocele should be determined carefully in considering history and physical examination of the patients, and postoperative complications.
Citations

Thyroid nodules are less common in children than in adults and their management is still controversial. The clinical presentations, operations, complications, histopathologic findings, and postoperative progressions of 34 pediatric patients that underwent thyroidectomy for palpable thyroid nodule at the Department of Surgery, Seoul National University Children Hospital between 1986 and 2003 were studied retrospectively by reviewing medical records and telephone interviews. The mean age of the patients was 11.8 years old. There were 23 females (67.6 %) and 11 males (32.4 %). Surgical indications were clinical need of histological confirmation (n=15), unresponsiveness to thyroxin replacement therapy (n=10), suggestion of the carcinoma on fine needle aspiration cytology (n=5), cosmetic purpose-a huge benign nodule (n=2), completion thyroidectomy for medullary thyroid carcinoma (n=1), and prophylactic thyroidectomy in a MENIIpatient (n=1). Unilateral Lobectomy was performed in 20 patients (57.1 %), subtotal thyroidectomy in 8 (22.9 %), total thyroidectomy in 5 (14.7 %), and completion thyroidectomy in 1 (2.9 %). Lymph node dissection was performed in 9 cases. Benign tumor was found in 23 patients (67.6 %), adenomatous goiter (n=18) and follicular adenoma (n=5). Malignant tumor was found in 11 children (32.4 %), 9 papillary carcinomas (26.5 %), and 2 medullary carcinomas (5.9 %). Of the 9 papillary carcinomas, 7 cases (77.8 %) had lymph node metastasis. No lymph node metastasis was found in 2 medullary carcinomas. Complications developed in 5 cases - transient hypocalcaemia (n=2), and temporary hoarseness (n=3). There was no mortality. Median follow-up period was 7.4 years (0.5-18 years). One patient showed recurrence in cervical lymph nodes 10 years after surgery and modified radical neck dissection was performed. Because of the high incidence of malignancy and advanced stage at initial presentation, more meticulous diagnostic work up is necessary for children with thyroid nodule, and more radical surgical treatment should be performed when malignant nodule is suggested.
Citations

One day surgery in children has been practiced for last 10 years in this institution. This study is to examine its safety and effectiveness for patients younger than 15 years old treated at the Department of Pediatric Surgery, Asan Medical Center, from September. 1996 to December, 2005. A total of 3,709 patients, 37 % of the total pediatric operations, are included in this retrospective study. The most prevalent ages were between 1 and 3 years olds (1,199 patients). Twenty patients were younger than 6 months, and they all had one day surgery safely. Operations were herniorrhaphy in 3,126 patients,followed by excisional biopsy, chemoport removal, and OK 432 injection. There were 12 cases (0.32 %) of unplanned admissions, 7 occurred within 6 months of one day surgery. Perioperative fever was the most common cause of admission in 4 cases. The related conditions of unplanned admission were bleeding in 2 cases and radical surgery in 2. One day surgery in this institution was easily accessible and safe. This is to the result of appropriate selection of patients, cooperation with anesthesiologists, adequate control of postoperative pain, and home care programs.
The purpose of this retrospective study was to evaluate the effects of diagnostic sonography in pediatric patients with inguinal hernias. The patients were classified into two groups. Group A included the patients who had been operated upon for inguinal hernia in 1980's, when diagnostic sonography was not available. Group B included the patients, operated upon for inguinal hernia from 2001 to 2002, when inguinal sonography was employed to detect potential bilateral hernias. The age distribution, sex ratio, laterality, bilaterality, and concomitant symptoms were compared between group A and group B. There were 296 cases in group A and 377 cases in group B. The prevalent age group was from 1 to 5 years. There was no difference in age group distribution between both groups. The male to female ratio was 5.3:1 in group A and 3.5:1 in group B. The ratio of unilateral to bilateral hernia was 5:1 in group A and 3:1 in group B. In cases with a unilateral hernia, the ratio of right to left was 1.5:1 in group A and 1.8:1 in group B. In cases with bilateral hernia, the simultaneous bilateral hernia was 33 cases (67.4 %) in group A and 75 cases (80.6 %) in group B. The sequential bilateral hernia was 16 cases (32.7 %) in group A and 18 cases (19.4 %) in group B. Although the ratio of bilateral hernia was increased in group B, the portion of the sequential bilateral hernia was significantly decreased in group B. In conclusion, there were no differences in the age distribution and the laterality between group A and B. The ratio of female patients and the incidence of bilateral hernia were increased in group B even though the portion of the sequential bilateral hernia was decreased. This result shows that the preoperative inguinal sonography in unilateral hernia with potential bilateral hernia is useful in early detection of the sequential contralateral hernia.
Citations

Diagnosis of acute appendicitis in children is sometimes difficult. The aim of this study is to validate a clinical scoring system and ultrasonography for the early diagnosis and treatment of appendicitis in childhood. This is a prospective study on 59 children admitted with abdominal pain at St. Mary's Hospital, the Catholic University of Korea from July 2002 to August 2003. We applied Madan Samuel's Pediatric Appendicitis Score (PAS) based on preoperative history, physical examination, laboratory finding and ultrasonography. This study was designed as follows: patients with score 5 or less were observed regardless of the positive ultrasonographic finding, patients with score 6 and 7 were decided according to the ultrasonogram and patients above score 8 were operated in spite of negative ultrasonographic finding. The patients were divided into two groups, appendicitis (group A) and non-appendicitis groups (group B). Group A consisted of 36 cases and Group B, 23 cases. Mean score of group A was 8.75 and group B was 6.13 (p<0.001). Comparing the diagnostic methods in acute appendicitis by surveying sensitivity, specificity, positive predictive value, negative predictive value, and accuracy, PAS gave 1.0000, 0.3043, 0.6923, 1.0000, and 0.7288, and ultrasonography gave 0.7778, 0.9130, 0.9333, 0.7241, and 0.8300 while the combined test gave 1.0000, 0.8696, 0.9231, 1.0000, and 0.9490, respectively. Negative laparotomy rate was 3 %. In conclusion, the combination of PAS and ultrasonography is a more accurate diagnostic tool than either PAS or ultrasonography.
Citations

A total of 30 cases of the peptic ulcer in children, who underwent operations from January 1981 to December 1995 because of complications at Department of the Surgery, Chonbuk National University Medical School, is reviewed. Twenty-three were males (76.7%), 7 females (23.3%) and male was preponderant at 3.3:1. There were 25 cases (83.3%) age 10 to 15 years, 3 (10.0%) between 2 and 9 years, and 2 (6.7%) below 2. The ulcer was located at duodenum in 27 (90.0%), and at stomach in 3 cases (10.0%). Complications were perforation in 19 cases (63.3%), pyloric obstruction in 9 (30.0%) and bleeding in 2 (6.7%). For perforation, truncal vagotomy with pyloroplasty was done in 11 cases, truncal vagotomy with hemigastrectomy and gastrojejunostomy in 6, and simple closure in 2 cases. For obstruction, truncal vagotomy with hemigastrectomy and gastrojejunostomy was done in 5, and truncal vagotomy and pyloroplasty in 3 cases. For bleeding lesions, truncal vagotomy and pyloroplasty was performed in 2 cases. Ten postoperative complications developed in 9 patients; adhesive ileus in 5, recurrence in 2, pneumonia 2, and wound seroma 1 case. One patient developed a primary duodenal perforation and another a recurrent obstruction. Both of patients had symptoms for more than 3 years and were treated with truncal vagotomy and pyloroplasty for the primary operations. Hospital stay was 11.5 days for the patient with perforated ulcer, 11.0 days for the patient with pyloric obstruction, and 14.5 days for the child with bleeding. Average hospital period was 11.6 days. To reduce recurrences after operation, extensive procedure such as distal gastrectomy with vagotomy at the first operation should be considered in case with severe complication or with patients who have been symptomatic for long periods.
The teratoma is a unique complex neoplasm and is one of the most frequent pediatric tumors originated from the extragonadal germ cells. Mature teratoma is composed of mature differentiated tissues, while immature teratoma always contains embryonic tissues of variable degrees of immaturity, especially in the neuroepithelial elements. Diagnosis of teratoma is relatively easy by conventional radiologic study, but the immaturity can be identified only by histopathological examination. Between January 1993 to December 2002, 63 cases of teratoma were operated and analysed retrospectively at the Chonnam University Hospital Female to male ratio was about 3:1 and age distribution was relatively even. Among 63 cases, gonadal teratoma was the most common (52.4%), followed by sacrococcygeal (25.4%), retroperitoneal (9.5%) and mediastinal teratoma (9.5%). Fifty-six cases were mature teratomas and seven were immature teratomas. Alpha-fetoprotein (AFP) was elevated in 4 of 6 immature cases, but in 2 of 51 mature ones Elevated AFP progressively returned to normal range by 1 month after operation in all. Complete excision of the mass was performed, and major complication was not noticed. In five immature cases, PEB chemotherapy (Cisplatin, Etoposide, Bleomycin) was performed. Two of 2 cases in histological grade II were well tolerated to the aggressive chemotherapy. One of three cases in grade III expired due to severe bone marrow depression, and two of them expired by tumor recurrences. In conclusion, immature teratoma in histological grade III showed high potentiality of recurrence. Therefore, postoperative chemotherapy has to be applied to the high graded immature tumors.
A lipomatous lesion of the cord is an accidentally encountered structure during the operative repair of inguinal hernia. This lesion has been reported as a lipoma of the cord in adults. However, there is only a limited number of reports in the pediatric age group. To evaluate the prevalence of this lesion in children and in order to review the surgical significancies, 600 hernia operations in 411 children during a period of 4 years from January, 2000 to December, 2003 in the Division of Pediatric Surgery, Department of Surgery, the Catholic University of Korea, were included in this study. There was a total of 31 (5.2%) lipomatous lesions in 25 (6.1%) cases; 3 cases in infants, 17 between 1 to 4 years, and 5 above 5 years of age. Male was more prevalent (male to female ratio 14:11). The laterality of clinical hernia with the lesions was 10 in the right, 13 in the left and 2 in both sides. The patients with ipsilateral lesions to the hernia were 14, contralateral in 5 and bilateral in 6 cases. Excluding 1 case of bilateral lesions in bilateral hernia, 10 lesions were contralateral to the clinical hernias. In 1 case, lipomatous lesion was the sole finding with nonsignificant patent processus vaginalis. Every lesion was suture ligated and resected with gentle traction of the dissected hernia sac. It has not been clearly defined whether the lesion is a stopper or a provocator of the hernia development. However, removal is highly recommended to make a differential diagnosis from the recurrent inguinal hernia in future. The term “lipomatous lesion” seems to be pathologically accurate and must be differentiate from the true lipomas.
Henoch-Schonlein purpura is a systemic vasculitis of unknown etiology that is probably related to autoimmune phenomenon. Henoch-Schonlein purpura is characterized by purpuric rash, arthragia, nephritis, and gastrointestinal manifestations. We reviewed 169 children hospitalized with a diagnosis of Henoch-Schonlein purpura at Asan Medical Center between 1989 and 1998. One- hundred thirty-nine (82.2%) had gastrointestinal manifestations including abdominal pain, nausea, vomiting and gastrointestinal bleeding. Surgical consultations were obtained for ten children, and laparotomy was performed on five children. Three children suspected of appendicitis underwent appendectomy. None had the evidence of appendicitis. One child who was suspected of intestinal strangulation revealed, in pathologic review, the hemorrhagic edema of the proximal jejunum and of the distal ileum at laparotomy. Another child underwent resection for hemorrhagic infarct of distal ileum. High suspicion of this disease entity in differential diagnosis of abdominal pain in children can avoid unnecessary laparotomy in most cases. However, the life-threatening gastrointestinal complications may occur in a small percent of cases. The prompt recognition and adequate radiologic evaluation of abdominal manifestation of this entity is needed for an early surgical intervention.
Pediatric laparoscopic splenectomy has gained increasing acceptance in the surgical management of a variety of splenic disorders, in particular hematologic diseases. We report our experience with 16 patients who underwent this procedure because of hematologic disorders during the past 3 and a half years at the Department of Surgery, St. Mary's Hospital, Catholic University Medical College. The mean age was 10 years (Range 6-16 years) and the mean spleen weight was 210 gm (Range 85-500 gm). The indications for splenectomy were hereditary spherocytosis (6 cases), idiopatic thrombocytopenic purpura (8 cases), autoimmune hemolytic anemia (1 case), and idiopatic splenomegaly (1 case). All splenectomies were performed safely with mean estimate blood loss of 233 ml. Mean operative time and mean postoperative hospital stay was 157 min and 4.5 days. Respectively postoperative pain medication was needed in 3 case, just one injection in immediate postoperative period. Diet was started on posterative second day or third day. In conclusions, Laparoscopic splenectomy in pediatric patients surely is a safe procedure, offering better cosmesis, much less pain, and shorter hospital stay with lower post operative mobidity.
Pediatric solid tumors have many similarity among different tumors. These tumors present small round cell types, and cause frequent diagnostic problems in pediatric pathology. An important advance in the investigation of these small round cell tumors has been the identification of consistent chromosomal translocations associated with several types of tumor. Eighteen patients with soft tissue sarcoma were available for review. Seventeen cell lines were also included in this study. The RNA from the specimens were analyzed by reverse transcriptase-polymerase chain reaction (RT-PCR). PAX3-FKHR fusion was present in four of five alveolar rhabdomyosarcoma and PAX7-FKHR fusion was detected in one of five alveolar rhabdomyosarcoma. None of the specimens expressed more than one chimeric transcript. EWS-FLI1 or EWS-ERG fusions were detected in all seven Ewings' sarcoma. No specimens showed EWS-WT1 fusion. These results corresponded well to the histopathologic diagnosis. There were no differences in the histologic appearances of tumors with the more frequent PAX3-FKHR or EWS-FLI1 fusions compared with those containing the variant PAX7-FKHR or EWS-ERG fusions. RT-PCR assay for chimeric transcript is an useful tool for a rapid and
objective
diagnosis of pediatric solid tumors. Through these tools, we can approach genetically to the differential diagnosis of undifferentiated small round tumors.
This is a clinical review of 2,191 pediatric surgical patients under the age of 15 years, operated upon at the Division of Pediatric Surgery, Department of Surgery, Chonnam University Hospital from January 1988 to December 1997. The total number of operations in the pediatric age for all specialties were 13,144(13.2 %). The total operations including those performed on adults were 99,555. The most common age group operated upon was under 5 year of age(44.4 %). The number of operations in Division of General Pediatric Surgery were 2,191(16.7 %) out of total 13,144 operations in all pediatric specialties. The patients under 1 year of age in general pediatric surgery was 42.9 %(941/2,191). The most common diseases in neonates were anorectal malformation(20.6 %) and hypertrophic pyloric stenosis( 20.3 %). Infants older than neonates most commonly were operated upon for inguinal hernia(32.4 %) and intussusception(19.6 %). The total mortality rate in the neonatal intensive care unit was 31.3 %. Gastroschisis had the highest mortality.
Citations

To evaluate the profitable central venous catheters (CVCs) in children, 320 CVCs placed in 255 neonate and children over a 10-year period were analyzed retrospectively. CVC was provided by one pediatric surgeon for a total of 6,116 patients days. The number of perioperative group including immediate TPN or chemo was 223, CVC just for TPN was 57 and chemotherapy 40. Local anesthesia was applied in 71 cases, and the others were under the general anesthesia. Subclavian vein catheterizations (SCVs) were 202 cases (82 infants and neonates), tunneled external jugular venotomy(EJV) 38, tunneled internal jugular venotomy(IJV) 2, facial venotomy (FV) 3, and umbilical venous catheterization (UVC) with vein transposition 74. In neonates, 72 UVCs were applied during laparotomy. SCV was increased with ages, 3 kg of minimal body weight. The average catheter-periods over-all were 19.1 days, of SCV 17 days, EJV 40, IJV 60 and UVC 14. Technical complications were; arterial puncture (6), puncture failure (5) and abnormal location(12) in SCV; insertion failure (3) in EJV; abnormal location in the portal vein (4) and the liver parenchyma (2) making cystic fluid accumulations in UVC. Twelve migrations (3.8%) out of position occurred; SCV(2), EJV (1) and UVC (9). For 4 cases (1.2 %) of catheter obstruction and 11 (3.4 %) of catheter infection (3 SCV, 2 EJV and 6 UVC), rescue procedures were applied with some achievements. There was one mortality (0.3 %) due to deep sedation in 1.06 kg baby for EJV. Cumulated surgeon's experience of the crafts, proper catheter selection and keeping the safety rouls would be the important factors for successful CVCs.
Citations

To understand the current status of pediatric surgical practice of the members of the Korean Association of Pediatric Sutgeons, a survey of the practice of the 31 members in both 1994 and 1995. Twenty five members(80%) representing 20 hospitals responded. An average of four hundred and seventy four cases pediatric surgical operations were performed at individual institution in 1995 with 40 newborn cases. Eighteen members(72%) ate currently working at university hospital. Fourteen institutions(70%) are currently classified as tertiary by the health insurance agency. The majority(l5 to 60%) of members are working in the metropolitan Seoul area, while five in Taegu area. Sixteen members reported having the title of department head/director. Four members reported occasional non-pediatric surgical practice. Nine members out of 20 reported having independent pediatric surgical out-patient clinic before the establishment of the association( 1985). Eight out of 15 members reported being appointed chief of pediatric surgery before 1985. In 20 institutions, 34 full time physicians(27 members, reportedly) are working in pediatric surgery. In regarding to pediatric surgical training, 16 members(64%) received an average of 16 months of training abroad, 5 members trained at home and abroad, and 4 from only at home. There are no differences in length of training periods in these groups. TWenty one members received their basic pediatric surgical training before 1985, the year of inauguration of the association. Twelve members received post-pediatric surgery refresher courses averaging 11 months' duration, after 2-11 years. Thirteen participants of this study belongs to the founding members of the association.
Thirty-four consecutive cases of thyroglossal duct lesions in children were reviewed at the Department of Surgery, Chonbuk National University Hospital. Twenty patients were males, and the most prevalent age of discovering was 2 to 4 years(52.9%). Resection was performed within .2 years after discovering the lesions in 19 cases, but was delayed untill 4 to 10 years in 6 cases. Cystic lesions(85.3%) were 5.8 times more common than fistulas. A midline upper neck mass was found in every cystic cases, and a draining sinus at hyoid region was noticed in fistula patients. The location of the lesion was on the hyoid bone in 34 cases, at the midline in 31 cases, slightly to the left in 2 cases, and slightly to the right in 1. Two cases were misdiagnosed as lymphadenopathy, and a single case of ectopic thyroid gland was misinterpreted as a thyroglossal duct cyst. Modified Sistrunk operation was performed in twenty-three cases(67.6%), Sistrunk operation in 9(26.5%), and cyst excision in 2(5.9%). Postoperative complications occurred in 4 cases(l1.8%); 2 wound infections and 2 recurrences. One of recurrences was a fistula treated by modified Sistrunk operation, and the other was a cyst treated by cyst excision.
The management of twenty-two cllildren with blunt abdominal trauma was analyzed. Nineteen cases had intraabciominal injuries; involving the spleen in 7 cases, the liver in 5, the pancreas in one and the bladder in one. There were five case multiple intraabdominal organ injuries. Seventeen out of 19 patients were treated non-operatively, but one was operated upon later because of delayed bleeding. Thirteen patients required transfusion in the non operated group, the mean values of the Pediatric Trauma Score (PTS) was 11.3. The mean lowest hemoglobulin(LHb) was 9.1 g/dL. The mean value of three cases with extraabdominal injuries were 9.0 and 8.3 g/dL respectively. The average amount of tranfusion was 17.3 ml/kg. In the operated group, 2 cases were transfused an average of 139.8 ml/kg and their mean PTS was 5 and LHb was 6.6 g/dL. In one out of 16 non-operated cases, intrahepatic hematoma developed and but resolved conservatively. However, two out of 3 operated cases suffer complications such as an intubation granuloma and an intraabdominal abscess with wound dehescence. In conclusion, non-operative managenent in child with blunt abdominal trauma was safe in Grade I and II solid organ injuries. The decision for operation should be based on the hemodynamic stability after initial resuscitation including transfusion.
Citations

Citations

Citations

Citations

Citations


